- Open access
- Published: 26 November 2021

Women’s Perceptions and Experiences of Breastfeeding: a scoping review of the literature
- Bridget Beggs 1 ,
- Liza Koshy 1 &
- Elena Neiterman 1
BMC Public Health volume 21 , Article number: 2169 ( 2021 ) Cite this article
15k Accesses
32 Citations
5 Altmetric
Metrics details
Despite public health efforts to promote breastfeeding, global rates of breastfeeding continue to trail behind the goals identified by the World Health Organization. While the literature exploring breastfeeding beliefs and practices is growing, it offers various and sometimes conflicting explanations regarding women’s attitudes towards and experiences of breastfeeding. This research explores existing empirical literature regarding women’s perceptions about and experiences with breastfeeding. The overall goal of this research is to identify what barriers mothers face when attempting to breastfeed and what supports they need to guide their breastfeeding choices.
This paper uses a scoping review methodology developed by Arksey and O’Malley. PubMed, CINAHL, Sociological Abstracts, and PsychInfo databases were searched utilizing a predetermined string of keywords. After removing duplicates, papers published in 2010–2020 in English were screened for eligibility. A literature extraction tool and thematic analysis were used to code and analyze the data.
In total, 59 papers were included in the review. Thematic analysis showed that mothers tend to assume that breastfeeding will be easy and find it difficult to cope with breastfeeding challenges. A lack of partner support and social networks, as well as advice from health care professionals, play critical roles in women’s decision to breastfeed.
While breastfeeding mothers are generally aware of the benefits of breastfeeding, they experience barriers at individual, interpersonal, and organizational levels. It is important to acknowledge that breastfeeding is associated with challenges and provide adequate supports for mothers so that their experiences can be improved, and breastfeeding rates can reach those identified by the World Health Organization.
Peer Review reports
Public health efforts to educate parents about the importance of breastfeeding can be dated back to the early twentieth century [ 1 ]. The World Health Organization is aiming to have at least half of all the mothers worldwide exclusively breastfeeding their infants in the first 6 months of life by the year 2025 [ 2 ], but it is unlikely that this goal will be achieved. Only 38% of the global infant population is exclusively breastfed between 0 and 6 months of life [ 2 ], even though breastfeeding initiation rates have shown steady growth globally [ 3 ]. The literature suggests that while many mothers intend to breastfeed and even make an attempt at initiation, they do not always maintain exclusive breastfeeding for the first 6 months of life [ 4 , 5 ]. The literature identifies various barriers, including return to paid employment [ 6 , 7 ], lack of support from health care providers and significant others [ 8 , 9 ], and physical challenges [ 9 ] as potential factors that can explain premature cessation of breastfeeding.
From a public health perspective, the health benefits of breastfeeding are paramount for both mother and infant [ 10 , 11 ]. Globally, new mothers following breastfeeding recommendations could prevent 974,956 cases of childhood obesity, 27,069 cases of mortality from breast cancer, and 13,644 deaths from ovarian cancer per year [ 11 ]. Global economic loss due to cognitive deficiencies resulting from cessation of breastfeeding has been calculated to be approximately USD $285.39 billion dollars annually [ 11 ]. Evidently, increasing exclusive breastfeeding rates is an important task for improving population health outcomes. While public health campaigns targeting pregnant women and new mothers have been successful in promoting breastfeeding, they also have been perceived as too aggressive [ 12 ] and failing to consider various structural and personal barriers that may impact women’s ability to breastfeed [ 1 ]. In some cases, public health messaging itself has been identified as a barrier due to its rigid nature and its lack of flexibility in guidelines [ 13 ]. Hence, while the literature on women’s perceptions regarding breastfeeding and their experiences with breastfeeding has been growing [ 14 , 15 , 16 ], it offers various, and sometimes contradictory, explanations on how and why women initiate and maintain breastfeeding and what role public health messaging plays in women’s decision to breastfeed.
The complex array of the barriers shaping women’s experiences of breastfeeding can be broadly categorized utilizing the socioecological model, which suggests that individuals’ health is a result of the interplay between micro (individual), meso (institutional), and macro (social) factors [ 17 ]. Although previous studies have explored barriers and supports to breastfeeding, the majority of articles focus on specific geographic areas (e.g. United States or United Kingdom), workplaces, or communities. In addition, very few articles focus on the analysis of the interplay between various micro, meso, and macro-level factors in shaping women’s experiences of breastfeeding. Synthesizing the growing literature on the experiences of breastfeeding and the factors shaping these experiences, offers researchers and public health professionals an opportunity to examine how various personal and institutional factors shape mothers’ breastfeeding decision-making. This knowledge is needed to identify what can be done to improve breastfeeding rates and make breastfeeding a more positive and meaningful experience for new mothers.
The aim of this scoping review is to synthesize evidence gathered from empirical literature on women’s perceptions about and experiences of breastfeeding. Specifically, the following questions are examined:
What does empirical literature report on women’s perceptions on breastfeeding?
What barriers do women face when they attempt to initiate or maintain breastfeeding?
What supports do women need in order to initiate and/or maintain breastfeeding?
Focusing on women’s experiences, this paper aims to contribute to our understanding of women’s decision-making and behaviours pertaining to breastfeeding. The overarching aim of this review is to translate these findings into actionable strategies that can streamline public health messaging and improve breastfeeding education and supports offered by health care providers working with new mothers.
This research utilized Arksey & O’Malley’s [ 18 ] framework to guide the scoping review process. The scoping review methodology was chosen to explore a breadth of literature on women’s perceptions about and experiences of breastfeeding. A broad research question, “What does empirical literature tell us about women’s experiences of breastfeeding?” was set to guide the literature search process.
Search methods
The review was undertaken in five steps: (1) identifying the research question, (2) identifying relevant literature, (3) iterative selection of data, (4) charting data, and (5) collating, summarizing, and reporting results. The inclusion criteria were set to empirical articles published between 2010 and 2020 in peer-reviewed journals with a specific focus on women’s self-reported experiences of breastfeeding, as well as how others see women’s experiences of breastfeeding. The focus on women’s perceptions of breastfeeding was used to capture the papers that specifically addressed their experiences and the barriers that they may encounter while breastfeeding. Only articles written in English were included in the review. The keywords utilized in the search strategy were developed in collaboration with a librarian (Table 1 ). PubMed, CINAHL, Sociological Abstracts, and PsychInfo databases were searched for the empirical literature, yielding a total of 2885 results.
Search outcome
The articles deemed to fit the inclusion criteria ( n = 213) were imported into RefWorks, an online reference manager tool and further screened for eligibility (Fig. 1 ). After the removal of 61 duplicates and title/abstract screening, 152 articles were kept for full-text review. Two independent reviewers assessed the papers to evaluate if they met the inclusion criteria of having an explicit analytic focus on women’s experiences of breastfeeding.
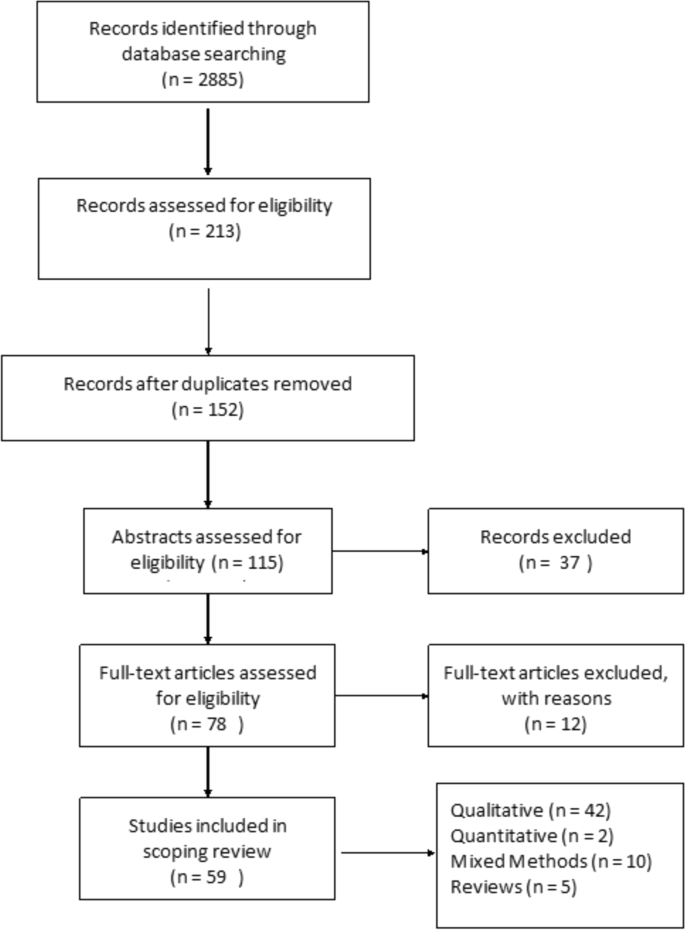
Prisma Flow Diagram
Quality appraisal
Consistent with scoping review methodology [ 18 ], the quality of the papers included in the review was not assessed.
Data abstraction
A literature extraction tool was created in MS Excel 2016. The data extracted from each paper included: (a) authors names, (b) title of the paper, (c) year of publication, (d) study objectives, (e) method used, (f) participant demographics, (g) country where the study was conducted, and (h) key findings from the paper.
Thematic analysis was utilized to identify key topics covered by the literature. Two reviewers independently read five papers to inductively generate key themes. This process was repeated until the two reviewers reached a consensus on the coding scheme, which was subsequently applied to the remainder of the articles. Key themes were added to the literature extraction tool and each paper was assigned a key theme and sub-themes, if relevant. The themes derived from the analysis were reviewed once again by all three authors when all the papers were coded. In the results section below, the synthesized literature is summarized alongside the key themes identified during the analysis.
In total, 59 peer-reviewed articles were included in the review. Since the review focused on women’s experiences of breastfeeding, as would be expected based on the search criteria, the majority of articles ( n = 42) included in the sample were qualitative studies, with ten utilizing a mixed method approach (Fig. 2 ). Figure 3 summarizes the distribution of articles by year of publication and Fig. 4 summarizes the geographic location of the study.
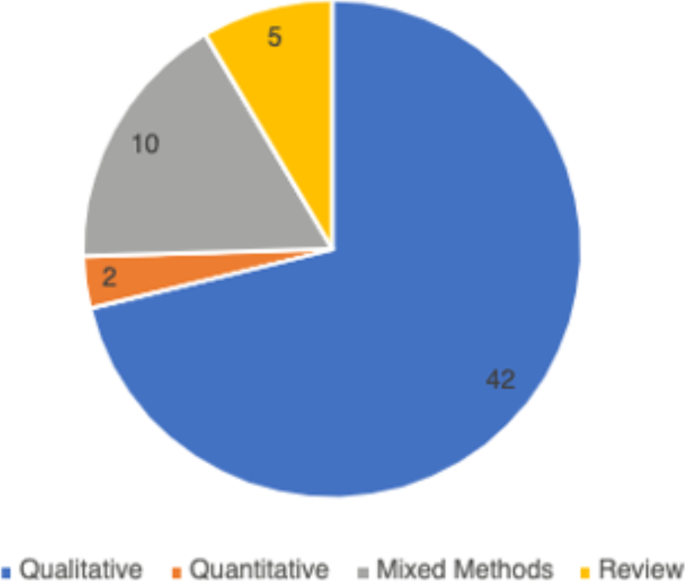
Types of Articles

Years of Publication
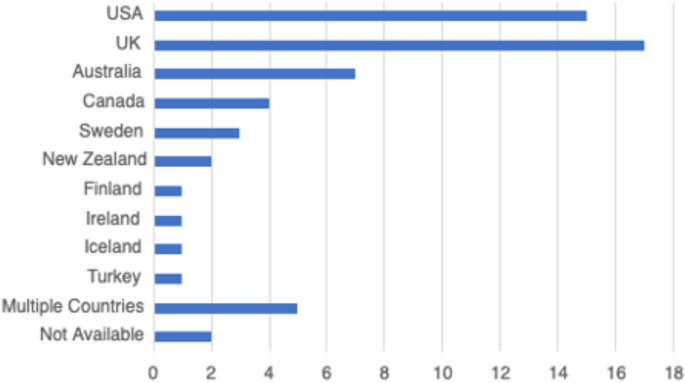
Countries of Focus Examined in Literature Review
Perceptions about breastfeeding
Women’s perceptions about breastfeeding were covered in 83% ( n = 49) of the papers. Most articles ( n = 31) suggested that women perceived breastfeeding as a positive experience and believed that breastfeeding had many benefits [ 19 , 20 ]. The phrases “breast is best” and “breastmilk is best” were repeatedly used by the participants of studies included in the reviewed literature [ 21 ]. Breastfeeding was seen as improving the emotional bond between the mother and the child [ 20 , 22 , 23 ], strengthening the child’s immune system [ 24 , 25 ], and providing a booster to the mother’s sense of self [ 1 , 26 ]. Convenience of breastfeeding (e.g., its availability and low cost) [ 19 , 27 ] and the role of breastfeeding in weight loss during the postpartum period were mentioned in the literature as other factors that positively shape mothers’ perceptions about breastfeeding [ 28 , 29 ].
The literature suggested that women’s perceptions of breastfeeding and feeding choices were also shaped by the advice of healthcare providers [ 30 , 31 ]. Paradoxically, messages about the importance and relative simplicity of breastfeeding may also contribute to misalignment between women’s expectations and the actual experiences of breastfeeding [ 32 ]. For instance, studies published in Canada and Sweden reported that women expected breastfeeding to occur “naturally”, to be easy and enjoyable [ 23 ]. Consequently, some women felt unprepared for the challenges associated with initiation or maintenance of breastfeeding [ 31 , 33 ]. The literature pointed out that mothers may feel overwhelmed by the frequency of infant feedings [ 26 ] and the amount as well as intensity of physical difficulties associated with breastfeeding initiation [ 33 ]. Researchers suggested that since many women see breastfeeding as a sign of being a “good” mother, their inability to breastfeed may trigger feelings of personal failure [ 22 , 34 ].
Women’s personal experiences with and perceptions about breastfeeding were also influenced by the cultural pressure to breastfeed. Welsh mothers interviewed in the UK, for instance, revealed that they were faced with judgement and disapproval when people around them discovered they opted out of breastfeeding [ 35 ]. Women recalled the experiences of being questioned by others, including strangers, when they were bottle feeding their infants [ 9 , 35 , 36 ].
Barriers to breastfeeding
The vast majority ( n = 50) of the reviewed literature identified various barriers for successful breastfeeding. A sizeable proportion of literature (41%, n = 24) explored women’s experiences with the physical aspects of breastfeeding [ 23 , 33 ]. In particular, problems with latching and the pain associated with breastfeeding were commonly cited as barriers for women to initiate breastfeeding [ 23 , 28 , 37 ]. Inadequate milk supply, both actual and perceived, was mentioned as another barrier for initiation and maintenance of breastfeeding [ 33 , 37 ]. Breastfeeding mothers were sometimes unable to determine how much milk their infants consumed (as opposed to seeing how much milk the infant had when bottle feeding), which caused them to feel anxious and uncertain about scheduling infant feedings [ 28 , 37 ]. Women’s inability to overcome these barriers was linked by some researchers to low self-efficacy among mothers, as well as feeling overwhelmed or suffering from postpartum depression [ 38 , 39 ].
In addition to personal and physical challenges experienced by mothers who were planning to breastfeed, the literature also highlighted the importance of social environment as a potential barrier to breastfeeding. Mothers’ personal networks were identified as a key factor in shaping their breastfeeding behaviours in 43 (73%) articles included in this review. In a study published in the UK, lack of role models – mothers, other female relatives, and friends who breastfeed – was cited as one of the potential barriers for breastfeeding [ 36 ]. Some family members and friends also actively discouraged breastfeeding, while openly questioning the benefits of this practice over bottle feeding [ 1 , 17 , 40 ]. Breastfeeding during family gatherings or in the presence of others was also reported as a challenge for some women from ethnic minority groups in the United Kingdom and for Black women in the United States [ 41 , 42 ].
The literature reported occasional instances where breastfeeding-related decisions created conflict in women’s relationships with significant others [ 26 ]. Some women noted they were pressured by their loved one to cease breastfeeding [ 22 ], especially when women continued to breastfeed 6 months postpartum [ 43 ]. Overall, the literature suggested that partners play a central role in women’s breastfeeding practices [ 8 ], although there was no consistency in the reviewed papers regarding the partners’ expressed level of support for breastfeeding.
Knowledge, especially practical knowledge about breastfeeding, was mentioned as a barrier in 17% ( n = 10) of the papers included in this review. While health care providers were perceived as a primary source of information on breastfeeding, some studies reported that mothers felt the information provided was not useful and occasionally contained conflicting advice [ 1 , 17 ]. This finding was reported across various jurisdictions, including the United States, Sweden, the United Kingdom and Netherlands, where mothers reported they had no support at all from their health care providers which made it challenging to address breastfeeding problems [ 26 , 38 , 44 ].
Breastfeeding in public emerged as a key barrier from the reviewed literature and was cited in 56% ( n = 33) of the papers. Examining the experiences of breastfeeding mothers in the United States, Spencer, Wambach, & Domain [ 45 ] suggested that some participants reported feeling “erased” from conversations while breastfeeding in public, rendering their bodies symbolically invisible. Lack of designated public spaces for breastfeeding forced many women to alter their feeding in public and to retreat to a private or a more secluded space, such as one’s personal car [ 25 ]. The oversexualization of women’s breasts was repeatedly noted as a core reason for the United States women’s negative experiences and feelings of self-consciousness about breastfeeding in front of others [ 45 ]. Studies reported women’s accounts of feeling the disapproval or disgust of others when breastfeeding in public [ 46 , 47 ], and some reported that women opted out of breastfeeding in public because they did not want to make those around them feel uncomfortable [ 25 , 40 , 48 ].
Finally, return to paid employment was noted in the literature as a significant challenge for continuation of breastfeeding [ 48 ]. Lack of supportive workplace environments [ 39 ] or inability to express milk were cited by women as barriers for continuing breastfeeding in the United States and New Zealand [ 39 , 49 ].
Supports needed to maintain breastfeeding
Due to the central role family members played in women’s experiences of breastfeeding, support from partners as well as female relatives was cited in the literature as key factors shaping women’s breastfeeding decisions [ 1 , 9 , 48 ]. In the articles published in Canada, Australia, and the United Kingdom, supportive family members allowed women to share the responsibility of feeding and other childcare activities, which reduced the pressures associated with being a new mother [ 19 , 20 ]. Similarly, encouragement, breastfeeding advice, and validation from healthcare professionals were identified as positively impacting women’s experiences with breastfeeding [ 1 , 22 , 28 ].
Community resources, such as peer support groups, helplines, and in-home breastfeeding support provided mothers with the opportunity to access help when they need it, and hence were reported to be facilitators for breastfeeding [ 19 , 22 , 33 , 44 ]. An increase in the usage of social media platforms, such as Facebook, among breastfeeding mothers for peer support were reported in some studies [ 47 ]. Public health breastfeeding clinics, lactation specialists, antenatal and prenatal classes, as well as education groups for mothers were identified as central support structures for the initiation and maintenance of breastfeeding [ 23 , 24 , 28 , 33 , 39 , 50 ]. Based on the analysis of the reviewed literature, however, access to these services varied greatly geographically and by socio-economic status [ 33 , 51 ]. It is also important to note that local and cultural context played a significant role in shaping women’s perceptions of breastfeeding. For example, a study that explored women’s breastfeeding experiences in Iceland highlighted the importance of breastfeeding in Icelandic society [ 52 ]. Women are expected to breastfeed and the decision to forgo breastfeeding is met with disproval [ 52 ]. Cultural beliefs regarding breastfeeding were also deemed important in the study of Szafrankska and Gallagher (2016), who noted that Polish women living in Ireland had a much higher rate of initiating breastfeeding compared to Irish women [ 53 ]. They attributed these differences to familial and societal expectations regarding breastfeeding in Poland [ 53 ].
Overall, the reviewed literature suggested that women faced socio-cultural pressure to breastfeed their infants [ 36 , 40 , 54 ]. Women reported initiating breastfeeding due to recognition of the many benefits it brings to the health of the child, even when they were reluctant to do it for personal reasons [ 8 ]. This hints at the success of public health education campaigns on the benefits of breastfeeding, which situates breastfeeding as a new cultural norm [ 24 ].
This scoping review examined the existing empirical literature on women’s perceptions about and experiences of breastfeeding to identify how public health messaging can be tailored to improve breastfeeding rates. The literature suggests that, overall, mothers are aware of the positive impacts of breastfeeding and have strong motivation to breastfeed [ 37 ]. However, women who chose to breastfeed also experience many barriers related to their social interactions with significant others and their unique socio-cultural contexts [ 25 ]. These different factors, summarized in Fig. 5 , should be considered in developing public health activities that promote breastfeeding. Breastfeeding experiences for women were very similar across the United Kingdom, United States, Canada, and Australia based on the studies included in this review. Likewise, barriers and supports to breastfeeding identified by women across the countries situated in the global north were quite similar. However, local policy context also impacted women’s experiences of breastfeeding. For example, maintaining breastfeeding while returning to paid employment has been identified as a challenge for mothers in the United States [ 39 , 45 ], a country with relatively short paid parental leave. Still, challenges with balancing breastfeeding while returning to paid employment were also noticed among women in New Zealand, despite a more generous maternity leave [ 49 ]. This suggests that while local and institutional policies might shape women’s experiences of breastfeeding, interpersonal and personal factors can also play a central role in how long they breastfeed their infants. Evidently, the importance of significant others, such as family members or friends, in providing support to breastfeeding mothers was cited as a key facilitator for breastfeeding across multiple geographic locations [ 29 , 34 , 48 ]. In addition, cultural beliefs and practices were also cited as an important component in either promoting breastfeeding or deterring women’s desire to initiate or maintain breastfeeding [ 15 , 29 , 37 ]. Societal support for breastfeeding and cultural practices can therefore partly explain the variation in breastfeeding rates across different countries [ 15 , 21 ]. Figure 5 summarizes the key barriers identified in the literature that inhibit women’s ability to breastfeed.
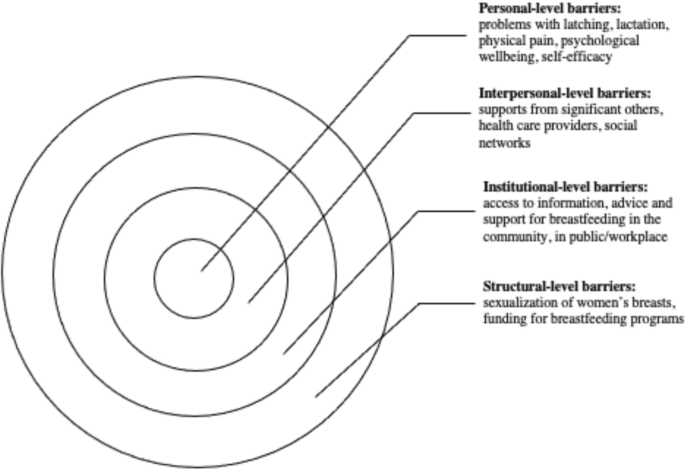
Barriers to Breastfeeding
At the individual level, women might experience challenges with breastfeeding stemming from various physiological and psychological problems, such as issues with latching, perceived or actual lack of breastmilk, and physical pain associated with breastfeeding. The onset of postpartum depression or other psychological problems may also impact women’s ability to breastfeed [ 54 ]. Given that many women assume that breastfeeding will happen “naturally” [ 15 , 40 ] these challenges can deter women from initiating or continuing breastfeeding. In light of these personal challenges, it is important to consider the potential challenges associated with breastfeeding that are conveyed to new mothers through the simplified message “breast is best” [ 21 ]. While breastfeeding may come easy to some women, most papers included in this review pointed to various challenges associated with initiating or maintaining breastfeeding [ 19 , 33 ]. By modifying public health messaging regarding breastfeeding to acknowledge that breastfeeding may pose a challenge and offering supports to new mothers, it might be possible to alleviate some of the guilt mothers experience when they are unable to breastfeed.
Barriers that can be experienced at the interpersonal level concern women’s communication with others regarding their breastfeeding choices and practices. The reviewed literature shows a strong impact of women’s social networks on their decision to breastfeed [ 24 , 33 ]. In particular, significant others – partners, mothers, siblings and close friends – seem to have a considerable influence over mothers’ decision to breastfeed [ 42 , 53 , 55 ]. Hence, public health messaging should target not only mothers, but also their significant others in developing breastfeeding campaigns. Social media may also be a potential medium for sharing supports and information regarding breastfeeding with new mothers and their significant others.
There is also a strong need for breastfeeding supports at the institutional and community levels. Access to lactation consultants, sound and practical advice from health care providers, and availability of physical spaces in the community and (for women who return to paid employment) in the workplace can provide more opportunities for mothers who want to breastfeed [ 18 , 33 , 44 ]. The findings from this review show, however, that access to these supports and resources vary greatly, and often the women who need them the most lack access to them [ 56 ].
While women make decisions about breastfeeding in light of their own personal circumstances, it is important to note that these circumstances are shaped by larger structural, social, and cultural factors. For instance, mothers may feel reluctant to breastfeed in public, which may stem from their familiarity with dominant cultural perspectives that label breasts as objects for sexualized pleasure [ 48 ]. The reviewed literature also showed that, despite the initial support, mothers who continue to breastfeed past the first year may be judged and scrutinized by others [ 47 ]. Tailoring public health care messaging to local communities with their own unique breastfeeding-related beliefs might help to create a larger social change in sociocultural norms regarding breastfeeding practices.
The literature included in this scoping review identified the importance of support from community services and health care providers in facilitating women’s breastfeeding behaviours [ 22 , 24 ]. Unfortunately, some mothers felt that the support and information they received was inadequate, impractical, or infused with conflicting messaging [ 28 , 44 ]. To make breastfeeding support more accessible to women across different social positions and geographic locations, it is important to acknowledge the need for the development of formal infrastructure that promotes breastfeeding. This includes training health care providers to help women struggling with breastfeeding and allocating sufficient funding for such initiatives.
Overall, this scoping review revealed the need for healthcare professionals to provide practical breastfeeding advice and realistic solutions to women encountering difficulties with breastfeeding. Public health messaging surrounding breastfeeding must re-invent breastfeeding as a “family practice” that requires collaboration between the breastfeeding mother, their partner, as well as extended family to ensure that women are supported as they breastfeed [ 8 ]. The literature also highlighted the issue of healthcare professionals easily giving up on women who encounter problems with breastfeeding and automatically recommending the initiation of formula use without further consideration towards solutions for breastfeeding difficulties [ 19 ]. While some challenges associated with breastfeeding are informed by local culture or health care policies, most of the barriers experienced by breastfeeding women are remarkably universal. Women often struggle with initiation of breastfeeding, lack of support from their significant others, and lack of appropriate places and spaces to breastfeed [ 25 , 26 , 33 , 39 ]. A change in public health messaging to a more flexible messaging that recognizes the challenges of breastfeeding is needed to help women overcome negative feelings associated with failure to breastfeed. Offering more personalized advice and support to breastfeeding mothers can improve women’s experiences and increase the rates of breastfeeding while also boosting mothers’ sense of self-efficacy.
Limitations
This scoping review has several limitations. First, the focus on “women’s experiences” rendered broad search criteria but may have resulted in the over or underrepresentation of specific findings in this review. Also, the exclusion of empirical work published in languages other than English rendered this review reliant on the papers published predominantly in English-speaking countries. Finally, consistent with Arksey and O’Malley’s [ 18 ] scoping review methodology, we did not appraise the quality of the reviewed literature. Notwithstanding these limitations, this review provides important insights into women’s experiences of breastfeeding and offers practical strategies for improving dominant public health messaging on the importance of breastfeeding.
Women who breastfeed encounter many difficulties when they initiate breastfeeding, and most women are unsuccessful in adhering to current public health breastfeeding guidelines. This scoping review highlighted the need for reconfiguring public health messaging to acknowledge the challenges many women experience with breastfeeding and include women’s social networks as a target audience for such messaging. This review also shows that breastfeeding supports and counselling are needed by all women, but there is also a need to tailor public health messaging to local social norms and culture. The role social institutions and cultural discourses have on women’s experiences of breastfeeding must also be acknowledged and leveraged by health care professionals promoting breastfeeding.
Availability of data and materials
All data generated or analysed during this study are included in this published article [and its supplementary information files].
Wolf JH. Low breastfeeding rates and public health in the United States. Am J Public Health. 2003;93(12):2000–2010. [cited 2021 Apr 21] Available from: http://ajph.aphapublications.org/doi/ https://doi.org/10.2105/AJPH.93.12.2000
World Health Organization, UNICEF. Global nutrition targets 2015: Breastfeeding policy brief 2014.
United Nations International Children’s Emergency Fund (UNICEF). Breastfeeding in the UK. 2019 [cited 2021 Apr 21]. Available from: https://www.unicef.org.uk/babyfriendly/about/breastfeeding-in-the-uk/
Semenic S, Loiselle C, Gottlieb L. Predictors of the duration of exclusive breastfeeding among first-time mothers. Res Nurs Health. 2008;31(5):428–441. [cited 2021 Apr 21] Available from: http://doi.wiley.com/ https://doi.org/10.1002/nur.20275
Hauck YL, Bradfield Z, Kuliukas L. Women’s experiences with breastfeeding in public: an integrative review. Women Birth. 2020;34:e217–27.
Hendaus MA, Alhammadi AH, Khan S, Osman S, Hamad A. Breastfeeding rates and barriers: a report from the state of Qatar. Int. J Women's Health. 2018;10:467–75 [cited 2021 Apr 20] Available from: /pmc/articles/PMC6110662/.
Google Scholar
Ogbo FA, Ezeh OK, Khanlari S, Naz S, Senanayake P, Ahmed KY, et al. Determinants of exclusive breastfeeding cessation in the early postnatal period among culturally and linguistically diverse (CALD) Australian mothers. Nutrients. 2019;11(7):1611 [cited 2021 Apr 21] Available from: https://www.mdpi.com/2072-6643/11/7/1611 .
Article Google Scholar
Ayton JE, Tesch L, Hansen E. Women’s experiences of ceasing to breastfeed: Australian qualitative study. BMJ Open. 2019;9(5):26234 [cited 2021 Apr 20] Available from: http://bmjopen.bmj.com/ .
Brown CRL, Dodds L, Legge A, Bryanton J, Semenic S. Factors influencing the reasons why mothers stop breastfeeding. Can J Public Heal. 2014;105(3):e179–e185. [cited 2021 Apr 20] Available from: https://link.springer.com/article/ https://doi.org/10.17269/cjph.105.4244
Sharma AJ, Dee DL, Harden SM. Adherence to breastfeeding guidelines and maternal weight 6 years after delivery. Pediatrics. 2014;134(Supplement 1):S42–S49. [cited 2021 Apr 21] Available from: www.pediatrics.org/cgi/doi/ https://doi.org/10.1542/peds.2014-0646H
Walters DD, Phan LTH, Mathisen R. The cost of not breastfeeding: Global results from a new tool. Health Policy Plan. 2019;34(6):407–17 [cited 2021 Apr 21] Available from: https://academic.oup.com/heapol/article/34/6/407/5522499 .
Friedman M. For whom is breast best? Thoughts on breastfeeding, feminism and ambivalence. J Mother Initiat Res Community Involv. 2009;11(1):26–35 [cited 2021 Apr 20] Available from: https://jarm.journals.yorku.ca/index.php/jarm/article/viewFile/22506/20986 .
Blixt I, Johansson M, Hildingsson I, Papoutsi Z, Rubertsson C. Women’s advice to healthcare professionals regarding breastfeeding: “offer sensitive individualized breastfeeding support” - an interview study. Int Breastfeed J 2019;14(1):51. [cited 2021 Apr 20] Available from: https://internationalbreastfeedingjournal.biomedcentral.com/articles/10.1186/s13006-019-0247-4
Obeng C, Dickinson S, Golzarri-Arroyo L. Women’s perceptions about breastfeeding: a preliminary study. Children. 2020;7(6):61 [cited 2021 Apr 21] Available from: https://www.mdpi.com/2227-9067/7/6/61 .
Choudhry K, Wallace LM. ‘Breast is not always best’: South Asian women’s experiences of infant feeding in the UK within an acculturation framework. Matern Child Nutr. 2012;8(1):72–87. [cited 2021 Apr 20] Available from: http://doi.wiley.com/ https://doi.org/10.1111/j.1740-8709.2010.00253.x
Da Silva TD, Bick D, Chang YS. Breastfeeding experiences and perspectives among women with postnatal depression: a qualitative evidence synthesis. Women Birth. 2020;33(3):231–9.
Kilanowski JF. Breadth of the socio-ecological model. J Agromedicine. 2017;22(4):295–7 [cited 2021 Apr 20] Available from: https://www.tandfonline.com/action/journalInformation?journalCode=wagr20 .
Arksey H, O’Malley L. Scoping studies: Towards a methodological framework. Int J Soc Res Methodol Theory Pract. 2005;8(1):19–32 [cited 2021 Apr 20] Available from: https://www.tandfonline.com/action/journalInformation?journalCode=tsrm20 .
Brown A, Lee M. An exploration of the attitudes and experiences of mothers in the United Kingdom who chose to breastfeed exclusively for 6 months postpartum. Breastfeed Med. 2011;6(4):197–204. [cited 2021 Apr 20] Available from: http://www.liebertpub.com/doi/ https://doi.org/10.1089/bfm.2010.0097
Morns MA, Steel AE, Burns E, McIntyre E. Women who experience feelings of aversion while breastfeeding: a meta-ethnographic review. Women Birth. 2021;34:128–35.
Jackson KT, Mantler T, O’Keefe-McCarthy S. Women’s experiences of breastfeeding-related pain. MCN Am J Matern Nurs. 2019;44(2):66–72 [cited 2021 Apr 20] Available from: https://journals.lww.com/00005721-201903000-00002 .
Burns E, Schmied V, Sheehan A, Fenwick J. A meta-ethnographic synthesis of women’s experience of breastfeeding. Matern Child Nutr. 2009;6(3):201–219. [cited 2021 Apr 20] Available from: http://doi.wiley.com/ https://doi.org/10.1111/j.1740-8709.2009.00209.x
Claesson IM, Larsson L, Steen L, Alehagen S. “You just need to leave the room when you breastfeed” Breastfeeding experiences among obese women in Sweden - A qualitative study. BMC Pregnancy Childbirth. 2018;18(1):1–10. [cited 2021 Apr 20] Available from: https://link.springer.com/articles/ https://doi.org/10.1186/s12884-017-1656-2
Asiodu IV, Waters CM, Dailey DE, Lyndon • Audrey. Infant feeding decision-making and the influences of social support persons among first-time African American mothers. Matern Child Health J. 2017;21:863–72.
Forster DA, McLachlan HL. Women’s views and experiences of breast feeding: positive, negative or just good for the baby? Midwifery. 2010;26(1):116–25.
Demirci J, Caplan E, Murray N, Cohen S. “I just want to do everything right:” Primiparous Women’s accounts of early breastfeeding via an app-based diary. J Pediatr Heal Care. 2018;32(2):163–72.
Furman LM, Banks EC, North AB. Breastfeeding among high-risk Inner-City African-American mothers: a risky choice? Breastfeed Med. 2013;8(1):58–67. [cited 2021 Apr 20]Available from: http://www.liebertpub.com/doi/ https://doi.org/10.1089/bfm.2012.0012
Cottrell BH, Detman LA. Breastfeeding concerns and experiences of african american mothers. MCN Am J Matern Nurs. 2013;38(5):297–304 [cited 2021 Apr 20] Available from: https://journals.lww.com/00005721-201309000-00009 .
Wambach K, Domian EW, Page-Goertz S, Wurtz H, Hoffman K. Exclusive breastfeeding experiences among mexican american women. J Hum Lact. 2016;32(1):103–111. [cited 2021 Apr 21] Available from: http://journals.sagepub.com/doi/ https://doi.org/10.1177/0890334415599400
Regan P, Ball E. Breastfeeding mothers’ experiences: The ghost in the machine. Qual Health Res. 2013;23(5):679–688. [cited 2021 Apr 21] Available from: http://journals.sagepub.com/doi/ https://doi.org/10.1177/1049732313481641
Hinsliff-Smith K, Spencer R, Walsh D. Realities, difficulties, and outcomes for mothers choosing to breastfeed: Primigravid mothers experiences in the early postpartum period (6-8 weeks). Midwifery. 2014;30(1):e14–9.
Palmér L. Previous breastfeeding difficulties: an existential breastfeeding trauma with two intertwined pathways for future breastfeeding—fear and longing. Int J Qual Stud Health Well-being. 2019;14(1) [cited 2021 Apr 21] Available from: https://www.tandfonline.com/action/journalInformation?journalCode=zqhw20 .
Francis J, Mildon A, Stewart S, Underhill B, Tarasuk V, Di Ruggiero E, et al. Vulnerable mothers’ experiences breastfeeding with an enhanced community lactation support program. Matern Child Nutr 2020;16(3):16. [cited 2021 Apr 20] Available from: https://onlinelibrary.wiley.com/doi/abs/ https://doi.org/10.1111/mcn.12957
Palmér L, Carlsson G, Mollberg M, Nyström M. Breastfeeding: An existential challenge - Women’s lived experiences of initiating breastfeeding within the context of early home discharge in Sweden. Int J Qual Stud Health Well-being 2010;5(3). [cited 2021 Apr 21] Available from: https://www.tandfonline.com/action/journalInformation?journalCode=zqhw20https://doi.org/ https://doi.org/10.3402/qhw.v5i3.5397
Grant A, Mannay D, Marzella R. ‘People try and police your behaviour’: the impact of surveillance on mothers and grandmothers’ perceptions and experiences of infant feeding. Fam Relationships Soc. 2018;7(3):431–47.
Thomson G, Ebisch-Burton K, Flacking R. Shame if you do - shame if you don’t: women’s experiences of infant feeding. Matern Child Nutr. 2015;11(1):33–46. [cited 2021 Apr 21] Available from: http://doi.wiley.com/ https://doi.org/10.1111/mcn.12148
Dietrich Leurer M, Misskey E. The psychosocial and emotional experience of breastfeeding: reflections of mothers. Glob Qual. Nurs Res. 2015;2:2333393615611654 [cited 2021 Apr 20] Available from: http://www.ncbi.nlm.nih.gov/pubmed/28462320 .
Fahlquist JN. Experience of non-breastfeeding mothers: Norms and ethically responsible risk communication. Nurs Ethics. 2016;23(2):231–241. [cited 2021 Apr 20] Available from: http://journals.sagepub.com/doi/ https://doi.org/10.1177/0969733014561913
Gross TT, Davis M, Anderson AK, Hall J, Hilyard K. Long-term breastfeeding in African American mothers: a positive deviance inquiry of WIC participants. J Hum Lact. 2017;33(1):128–139. [cited 2021 Apr 20] Available from: http://journals.sagepub.com/doi/ https://doi.org/10.1177/0890334416680180
Spencer RL, Greatrex-White S, Fraser DM. ‘I thought it would keep them all quiet’. Women’s experiences of breastfeeding as illusions of compliance: an interpretive phenomenological study. J Adv Nurs. 2015;71(5):1076–1086. [cited 2021 Apr 21] Available from: http://doi.wiley.com/ https://doi.org/10.1111/jan.12592
Twamley K, Puthussery S, Harding S, Baron M, Macfarlane A. UK-born ethnic minority women and their experiences of feeding their newborn infant. Midwifery. 2011;27(5):595–602.
PubMed Google Scholar
Lutenbacher M, Karp SM, Moore ER. Reflections of Black women who choose to breastfeed: influences, challenges, and supports. Matern Child Health J. 2016;20(2):231–9.
Dowling S, Brown A. An exploration of the experiences of mothers who breastfeed long-term: what are the issues and why does it matter? Breastfeed Med. 2013;8(1):45–52. [cited 2021 Apr 20] Available from: http://www.liebertpub.com/doi/ https://doi.org/10.1089/bfm.2012.0057
Fox R, McMullen S, Newburn M. UK women’s experiences of breastfeeding and additional breastfeeding support: a qualitative study of baby Café services. BMC Pregnancy Childbirth 2015;15(1):147. [cited 2021 Apr 20] Available from: http://bmcpregnancychildbirth.biomedcentral.com/articles/ https://doi.org/10.1186/s12884-015-0581-5
Spencer B, Wambach K, Domain EW. African American women’s breastfeeding experiences: cultural, personal, and political voices. Qual Health Res. 2015;25(7):974–987. [cited 2021 Apr 21] Available from: http://journals.sagepub.com/doi/ https://doi.org/10.1177/1049732314554097
McBride-Henry K. The influence of the They: An interpretation of breastfeeding culture in New Zealand. Qual Health Res. 2010;20(6):768–777. [cited 2021 Apr 21] Available from: http://journals.sagepub.com/doi/ https://doi.org/10.1177/1049732310364220
Newman KL, Williamson IR. Why aren’t you stopping now?!’ Exploring accounts of white women breastfeeding beyond six months in the east of England. Appetite. 2018 Oct;1(129):228–35.
Dowling S, Pontin D. Using liminality to understand mothers’ experiences of long-term breastfeeding: ‘Betwixt and between’, and ‘matter out of place.’ Heal (United Kingdom). 2017;21(1):57–75. [cited 2021 Apr 20] Available from: http://journals.sagepub.com/doi/ https://doi.org/10.1177/1363459315595846
Payne D, Nicholls DA. Managing breastfeeding and work: a Foucauldian secondary analysis. J Adv Nurs. 2010;66(8):1810–1818. [cited 2021 Apr 21] Available from: http://doi.wiley.com/ https://doi.org/10.1111/j.1365-2648.2009.05156.x
Keely A, Lawton J, Swanson V, Denison FC. Barriers to breast-feeding in obese women: a qualitative exploration. Midwifery. 2015;31(5):532–9.
Afoakwah G, Smyth R, Lavender DT. Women’s experiences of breastfeeding: A narrative review of qualitative studies. Afr J Midwifery Womens Health. 2013 ;7(2):71–77. [cited 2021 Apr 21] Available from: https://www.magonlinelibrary.com/doi/abs/ https://doi.org/10.12968/ajmw.2013.7.2.71
Símonardóttir S. Getting the green light: experiences of Icelandic mothers struggling with breastfeeding. Sociol Res Online. 2016;21(4):1.
Szafranska M, Gallagher DL. Polish women’s experiences of breastfeeding in Ireland. Pract Midwife. 2016;19(1):30–2 [cited 2021 Apr 21] Available from: https://europepmc.org/article/med/26975131 .
Pratt BA, Longo J, Gordon SC, Jones NA. Perceptions of breastfeeding for women with perinatal depression: a descriptive phenomenological study. Issues Ment Health Nurs. 2020;41(7):637–644. [cited 2021 Apr 21] Available from: https://www.tandfonline.com/doi/abs/ https://doi.org/10.1080/01612840.2019.1691690
Durmazoğlu G, Yenal K, Okumuş H. Maternal emotions and experiences of mothers who had breastfeeding problems: a qualitative study. Res Theory Nurs Pract. 2020;34(1):3–20. [cited 2021 Apr 20] Available from: http://connect.springerpub.com/lookup/doi/ https://doi.org/10.1891/1541-6577.34.1.3
Burns E, Triandafilidis Z. Taking the path of least resistance: a qualitative analysis of return to work or study while breastfeeding. Int Breastfeed J. 2019;14(1):1–13.
Download references
Acknowledgements
The authors would like to acknowledge the assistance of Jackie Stapleton, the University of Waterloo librarian, for her assistance with developing the search strategy used in this review.
Not applicable.
Author information
Authors and affiliations.
School of Public Health Sciences, University of Waterloo, 200 University Ave West, Waterloo, ON, N2L 3G1, Canada
Bridget Beggs, Liza Koshy & Elena Neiterman
You can also search for this author in PubMed Google Scholar
Contributions
BB was responsible for the formal analysis and organization of the review. LK was responsible for data curation, visualization and writing the original draft. EN was responsible for initial conceptualization and writing the original draft. BB and LK were responsible for reviewing and editing the manuscript. All authors read and approved the final manuscript.
Authors’ information
BB is completing her Bachelor of Science (BSc) degree at the School of Public Health Sciences at the University of Waterloo.
LK is completing her Bachelor of Public Health (BPH) degree at the School of Public Health Sciences at the University of Waterloo.
EN (PhD), is a continuing lecturer at the School of Public Health Sciences at the University of Waterloo. Her areas of expertise are in women’s reproductive health and sociology of health, illness, and healthcare.
Corresponding author
Correspondence to Bridget Beggs .
Ethics declarations
Ethics approval and consent to participate, consent for publication, competing interests.
The authors declare that they have no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Beggs, B., Koshy, L. & Neiterman, E. Women’s Perceptions and Experiences of Breastfeeding: a scoping review of the literature. BMC Public Health 21 , 2169 (2021). https://doi.org/10.1186/s12889-021-12216-3
Download citation
Received : 23 June 2021
Accepted : 10 November 2021
Published : 26 November 2021
DOI : https://doi.org/10.1186/s12889-021-12216-3
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Breastfeeding
- Experiences
- Public health
BMC Public Health
ISSN: 1471-2458
- General enquiries: [email protected]
An official website of the United States government
Official websites use .gov A .gov website belongs to an official government organization in the United States.
Secure .gov websites use HTTPS A lock ( Lock Locked padlock icon ) or https:// means you've safely connected to the .gov website. Share sensitive information only on official, secure websites.
- Publications
- Account settings
- Advanced Search
- Journal List

Breastfeeding and maternal health outcomes: a systematic review and meta-analysis
Ranadip chowdhury, bireshwar sinha, mari jeeva sankar, sunita taneja, nita bhandari, nigel rollins, jose martines.
- Author information
- Article notes
- Copyright and License information
Dr Ranadip Chowdhury, Scientist, Centre for Health Research and Development, Society for Applied Studies, 45, Kalu Sarai, New Delhi-110016, India. Tel: +91 011 46043751- 55 | Fax: +91 011 46043756 | Email: [email protected]
Received 2015 May 18; Revised 2015 Jun 16; Accepted 2015 Jun 18; Issue date 2015 Dec.
This is an open access article under the terms of the Creative Commons Attribution License, which permits use, distribution and reproduction in any medium, provided the original work is properly cited.
To evaluate the effect of breastfeeding on long-term (breast carcinoma, ovarian carcinoma, osteoporosis and type 2 diabetes mellitus) and short-term (lactational amenorrhoea, postpartum depression, postpartum weight change) maternal health outcomes.
A systematic literature search was conducted in PubMed, Cochrane Library and CABI databases. Outcome estimates of odds ratios or relative risks or standardised mean differences were pooled. In cases of heterogeneity, subgroup analysis and meta-regression were explored.
Breastfeeding >12 months was associated with reduced risk of breast and ovarian carcinoma by 26% and 37%, respectively. No conclusive evidence of an association between breastfeeding and bone mineral density was found. Breastfeeding was associated with 32% lower risk of type 2 diabetes. Exclusive breastfeeding and predominant breastfeeding were associated with longer duration of amenorrhoea. Shorter duration of breastfeeding was associated with higher risk of postpartum depression. Evidence suggesting an association of breastfeeding with postpartum weight change was lacking.
This review supports the hypothesis that breastfeeding is protective against breast and ovarian carcinoma, and exclusive breastfeeding and predominant breastfeeding increase the duration of lactational amenorrhoea. There is evidence that breastfeeding reduces the risk of type 2 diabetes. However, an association between breastfeeding and bone mineral density or maternal depression or postpartum weight change was not evident.
Keywords: Breastfeeding, Long and Short Term, Maternal health, Meta-analysis
Introduction
Breast milk is the natural first food for newborns. It provides all the energy and nutrients that an infant needs for the first six months of life, up to half or more during the second half of infancy and up to one-third during the second year of life ( 1 , 2 ). For mothers, breastfeeding has been reported to confer lower risk of breast and ovarian carcinoma ( 3 , 4 ), greater postpartum weight loss ( 5 ) and decreased blood pressure ( 6 ) compared with no breastfeeding. The World Health Organization (WHO) recommends exclusive breastfeeding in the first six months and continuation of breastfeeding for 2 years and beyond ( 1 ).
The association between breastfeeding and breast carcinoma in mothers has received increased scrutiny in recent years. A number of studies have suggested that breastfeeding, particularly for an extended period of time, may be associated with a decreased risk of breast carcinoma, even after adjustment for potential confounders ( 7 ). It is difficult, however, to estimate the magnitude of association between breastfeeding duration and breast carcinoma if any, because of the different methodologies used in breastfeeding histories. Parity is also a protective factor against breast carcinoma ( 8 ), and there may be an interaction between parity and breastfeeding duration interplay in protecting women from breast carcinoma.
Longer duration of breastfeeding protects against breast and ovarian carcinoma.
Exclusive breastfeeding and predominant breastfeeding increase the duration of lactational amenorrhoea.
Evidence on the association between breastfeeding and maternal bone mineral density, maternal depression or postpartum weight change was lacking.
Ovarian cancer is one of the most common cancers in female ( 9 , 10 ). Reproductive factors have been identified as markers of risk for ovarian cancer. These reproductive factors mainly include total number of pregnancies, parity, age at menarche and menopause, as well as breastfeeding ( 11 ). Evidence from previous analyses indicates an inverse association between breastfeeding and the risk of ovarian carcinoma ( 4 , 12 ).
Calcium metabolism and bone metabolism are substantially altered with increased calcium demands during pregnancy and lactation. Bone densities can decrease by between 3 and 10 per cent in the span of a few months in a healthy mother ( 13 ). Confounders commonly considered in the studies of the relationship between fracture risk and breastfeeding are age, hormone replacement therapy, parity and BMI ( 4 ).
Available literature suggests that breastfeeding reduces the risk of maternal type 2 diabetes in some cohort studies, but the evidence from published studies has differed with regard to the strength of the association ( 14 , 15 ).
The literature suggests that exclusive breastfeeding protects against pregnancy ( 16 , 17 ). Some studies, however, show that exclusive breastfeeding is not always associated with inhibition of ovulation ( 18 , 19 ).
The incidence of postpartum depression (PPD) is high (10–15%) ( 20 ), and depression during pregnancy usually continues into the postpartum period ( 21 ). Postpartum depression has an immediate impact on mothers. It carries long-term risks for their mental health ( 22 ) and may also have significant negative effects on the cognitive, social and physical development of their children ( 23 ). The evidence for an association between breastfeeding and PPD is, however, unclear ( 23 , 24 ).
Postpartum weight retention is a predictor for future overweight and obesity ( 25 ) and is associated with obesity-related illnesses, such as type 2 diabetes mellitus and cardiovascular disease ( 26 ). Breastfeeding may promote weight loss due to lactation ( 27 ), but there is a lack of strong evidence to support this hypothesis ( 28 ).
We conducted this review to summarise the literature and explore the relationship of breastfeeding and its duration with long-term (breast carcinoma, ovarian carcinoma, osteoporosis and type 2 diabetes mellitus) and short-term (lactational amenorrhoea, postpartum depression, postpartum weight change) maternal health outcomes. Outcomes for review were selected during an expert meeting at the World Health Organization (October 2014) that was reviewing the impact of breastfeeding on maternal and child health.
A search strategy (Box 1 ) was developed and reviewed by all authors. Medical Subject Heading ( 29 ) terms and keywords were used in various combinations. We searched published literature from PubMed, Cochrane Library and CABI databases to identify studies examining the effect of type and duration of breastfeeding on maternal health outcomes. We conducted the search in February 2015. No language or date restrictions were employed in the electronic search.
Box 1. Search strategy for breastfeeding & maternal health
Breastfeeding OR Breast Feeding OR Lactation OR Human Milk OR Breast Milk
Women OR Maternal OR Postpartum OR puerperal OR postnatal OR Birth OR gestation
Diabetes OR (Breast AND (Carcinoma OR carcinoma OR tumor OR malignancy)) OR (Ovarian OR Ovary AND (Carcinoma OR carcinoma OR tumor OR malignancy)) OR (depression OR Blues OR psychosis) OR (Amenorrhea OR Contraception) OR (Osteoporosis OR Bone mineral density) OR Weight OR BMI OR body mass index
(Addresses[ptyp] OR Autobiography[ptyp] OR Bibliography[ptyp] OR Biography[ptyp] OR pubmed books[filter] OR Case Reports[ptyp] OR Congresses[ptyp] OR Consensus Development Conference[ptyp] OR Directory[ptyp] OR Duplicate Publication[ptyp] OR Editorial[ptyp] OR Festschrift[ptyp] OR Guideline[ptyp] OR In Vitro [ptyp] OR Interview[ptyp] OR Lectures[ptyp] OR Legal Cases[ptyp] OR News[ptyp] OR Newspaper Article[ptyp] OR Personal Narratives[ptyp] OR Portraits[ptyp] OR Retracted Publication[ptyp] OR Twin Study[ptyp] OR Video-Audio Media[ptyp])
#1 AND #2 AND #3
Two review authors (RC and BS) screened the titles and abstracts independently to identify potentially relevant citations. These review authors retrieved the full texts of all potentially relevant articles and independently assessed the eligibility of the studies using predefined inclusion criteria. We extracted data from all articles found to be relevant by both authors. Any disagreements or discrepancies between reviewers were resolved by discussion and if necessary by consulting a third author (JSM). In addition to the electronic search, we searched reference lists of the articles identified. We used Web-based citation index for citing manuscripts of these identified articles.
We identified four recent systematic reviews addressing the following outcomes: ovarian carcinoma ( 30 ), type 2 diabetes mellitus ( 31 ), postpartum depression ( 32 ) and postpartum weight change ( 33 ). We planned to update these reviews and provide new quantitative estimates of breastfeeding on these health outcomes. For other maternal health outcomes, that is breast carcinoma, osteoporosis and lactational amenorrhoea, we planned for new reviews.
Inclusion criteria
We selected all observational studies (prospective/retrospective cohort and case–control), randomised controlled trials (RCTs), including cluster randomised trials, and quasi-experimental trials which examined the impact of duration and type of breastfeeding on maternal health outcomes. For articles not written in English, we attempted to get an English abstract. If it was not available, the article was excluded.
Abstraction, summary measure, breastfeeding categories and analysis
We abstracted data using a modified Cochrane data abstraction form. If a study provided separate estimates for hospital- and community-based populations, then the outcome estimates were pooled separately. We used odds ratios (ORs), both adjusted and unadjusted, as our outcome estimate for breast and ovarian carcinoma. Relative risk (RR) was used as the outcome estimate for lactational amenorrhoea. To examine the effect on breast and ovarian carcinoma, breastfeeding was categorised into ever breastfed vs. never breastfed and also by breastfeeding duration, that is breastfed less than six months vs. not breastfed; breastfed 6 to 12 months vs. not breastfed; and breastfed >12 months vs. not breastfed. For lactational amenorrhoea, we used exclusive, predominant, partial, any and no breastfeeding as the categories (Table A1 ). Standardised mean differences in bone mineral density between highest and lowest breastfeeding duration categories were used for osteoporosis outcome. A narrative approach was used to summarise the studies for postpartum weight change as the studies were very heterogeneous.
We performed meta-analysis with Stata 11.2 software (StataCorp, College Station, TX, USA). We calculated the pooled estimates of the outcome measures from the odds ratios (ORs), relative risks (RRs), standardised mean differences (SMDs) and 95% confidence intervals (CIs) of the individual studies by inverse variance or DerSimonian and Laird method in Stata ( 34 ). High heterogeneity was defined by either a low p-value (<0.10) or I 2 value greater than 60%. In cases of high heterogeneity, the random-effects model was used and causes were explored by conducting subgroup analysis and meta-regression. Subgroup analyses were carried out based on breastfeeding categories (ever vs never, less than six months vs never, 6–12 months vs never, >12 months vs never). Among the ever vs never breastfeeding category, subgroup analyses were carried out based on sample size (<500, 500–1499, ≥1500), individual study setting (i.e. high-income country (HIC) or low- and middle-income country (LMIC) ( 35 )), study design (cohort, case–control), mean age of diagnosis (≤49 years, >49 years), adjustment for parity (fine adjustment, i.e. adjustment according to each parity number measured as 0, 1, 2, 3, 4+; crude adjustment, i.e. groupwise adjustment measured as 0, 1–3, 4+ children; and no adjustment), control for confounding (thorough, i.e. controlled for all potential socio-demographic and reproductive factors such as age, income, ethnicity, parity, contraceptive use, family history of carcinoma, menopausal status and smoking; partial, i.e. only partially controlled for potential socio-demographic and reproductive factors; and none) and quality of study (adequate, i.e. study had none or one among selection bias, measurement bias, attrition (20%) and confounding bias; inadequate) ( 36 ). We also evaluated the presence of publication bias in the extracted data for the primary outcome using Begg's test or Egger's test or funnel plots ( 37 ).
We screened the 12 071 titles identified. Of these, after reviewing abstracts of 1501 articles, we selected 341 for full-text review. We identified 163 articles for inclusion in our final database (Fig. 1 ). Among these, 100 studies examined the impact of breastfeeding on breast carcinoma, 40 studies on ovarian carcinoma, 12 studies on lactational amenorrhoea, five studies on postpartum weight change and six studies on osteoporosis. We did fresh meta-analysis for breast carcinoma, ovarian carcinoma, osteoporosis and lactational amenorrhoea and updated the review on postpartum weight change. No new studies subsequent to the existing reviews on type 2 diabetes mellitus and postpartum depression ( 31 , 32 ) were found to be eligible for inclusion.
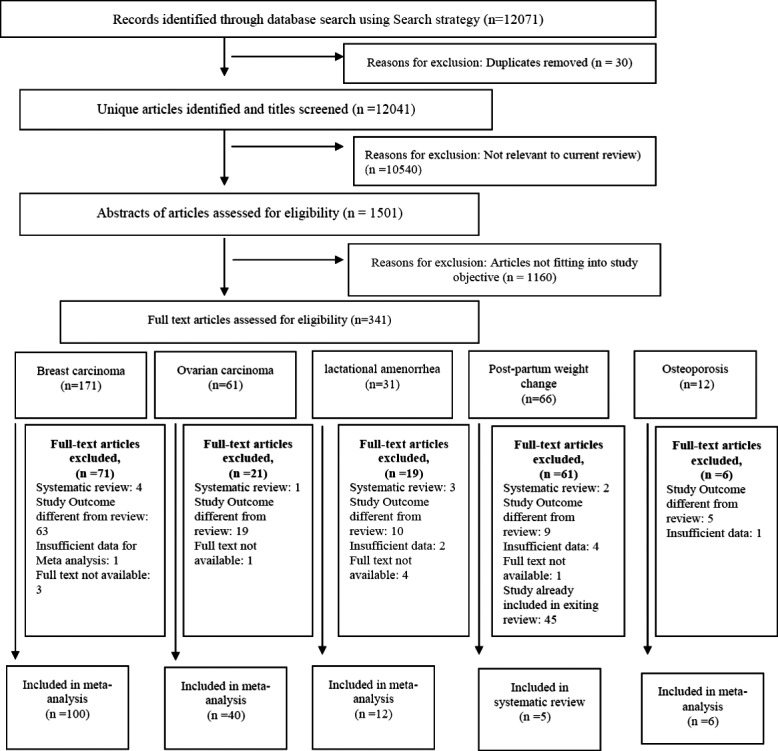
: Prisma Flow chart.
Effects of breastfeeding on long-term maternal health outcomes
Breast carcinoma.
We identified 98 estimates ( 38 – 135 ) of the association between ever breastfeeding and breast carcinoma risk (Tables 1 and A2 ). Ever breastfeeding was associated with 22% (OR 0.78, 95% CI 0.74–0.82) (Fig. 2 ) reduction of breast carcinoma risk compared with never breastfeeding. Compared with no breastfeeding, breastfeeding for less than six months (39 estimates) and breastfeeding for 6–12 months (36 estimates) were associated with 7% (OR 0.93, 95% CI 0.88–0.99) and 9% (OR 0.91, 95% CI 0.87–0.96) risk reduction of breast carcinoma, respectively. We found that mothers who breastfed for >12 months compared with those who did not breastfeed had a 26% lower risk of developing breast carcinoma (50 studies; OR 0.74, 95% CI 0.69–0.79), and when restricted to high-quality studies, only (41 studies) breastfeeding >12 months was associated with 23% lower risk of developing breast carcinoma (OR 0.77, 95% CI 0.72–0.83) (not shown in Table 1 ). There was, however, an indication of publication bias. Asymmetry was observed in funnel plot when inspected visually. Both Egger's test (p bias <0.001) and Begg's test (p bias <0.001) showed statistically significant findings.
Risk of breast carcinoma by breastfeeding duration and by subgroup
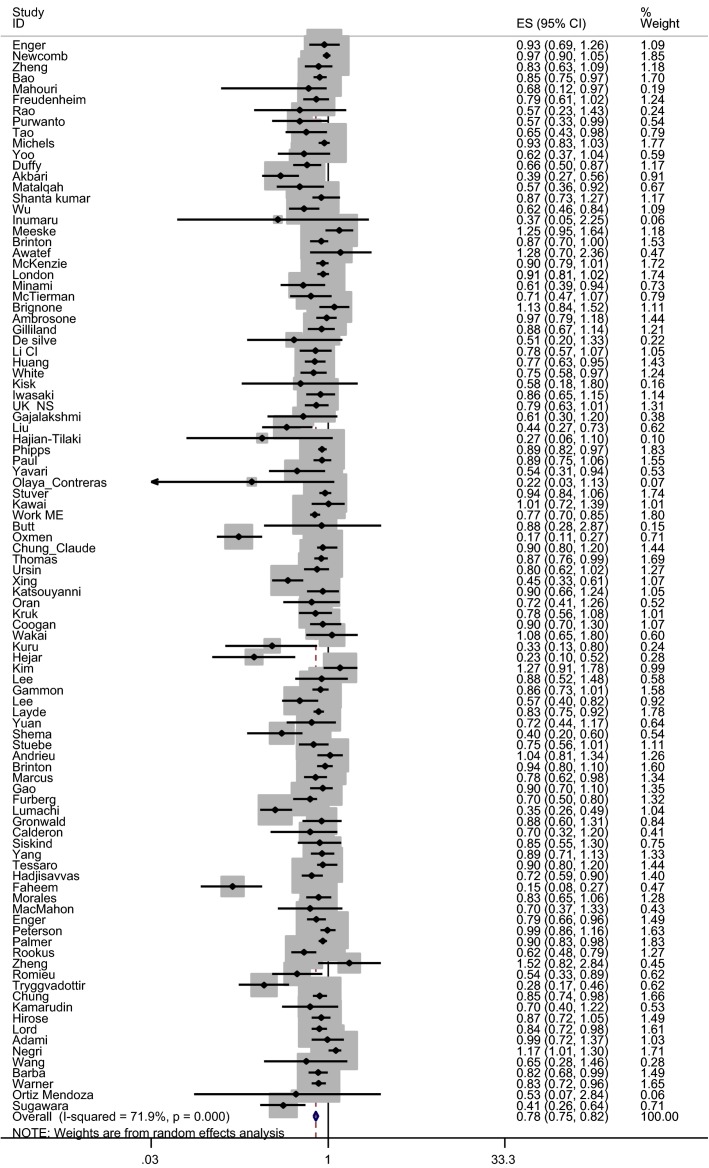
Effect of ever breastfeeding vs. no breastfeeding on risk of breast carcinoma.
Subgroup analysis of the effects of ever breastfeeding on risk of breast carcinoma among studies conducted in high-income countries, with large sample sizes (>1500), of cohort design, with thorough control of confounding factors and adequate quality showed a smaller breast carcinoma risk reduction. Studies where fine adjustment for parity was made showed a smaller effect of breastfeeding on breast carcinoma risk reduction (OR 0.92, 95% CI 0.88–0.96) compared with studies where crude adjustment or no adjustment was made. A restricted analysis including parous women in the fine adjustment subgroup showed a risk reduction of 7% for breast carcinoma (OR 0.93, 95% CI 0.89–0.97; 14 estimates) (not shown in Table 1 ).
Ovarian carcinoma
Pooled results from 41 estimates ( 65 , 69 , 136 – 173 ) showed that mothers who ever breastfed their children had a 30% reduction in the risk of ovarian carcinoma, when compared with those who never breastfed (OR 0.70, 95% CI 0.64–0.77) (Tables 2 and A3 ; Fig. 3 ). The risk of ovarian carcinoma was 17% lower among women who had breastfed for less than six months when compared with those who did not breastfeed (OR 0.83, 95% CI 0.78–0.89). The risk of ovarian carcinoma among mothers who breastfed for 6–12 months was 28% lower (OR 0.72, 95% CI 0.66–0.78; 19 estimates) when compared with women who had not breastfed. The highest risk reduction was observed among women who breastfed for more than 12 months, in whom the risk of ovarian carcinoma was 37% lower than among women who had not breastfed (OR 0.63; 95% CI 0.56–0.71; 29 estimates). The effect size was slightly less (OR 0.65, 95% CI 0.57–0.73), when the analyses were restricted to high-quality studies (29 estimates). There was no evidence of publication bias in Egger's test or Begg's test (p bias >0.1) in either of the analyses.
Risk of ovarian carcinoma by breastfeeding duration and by subgroup
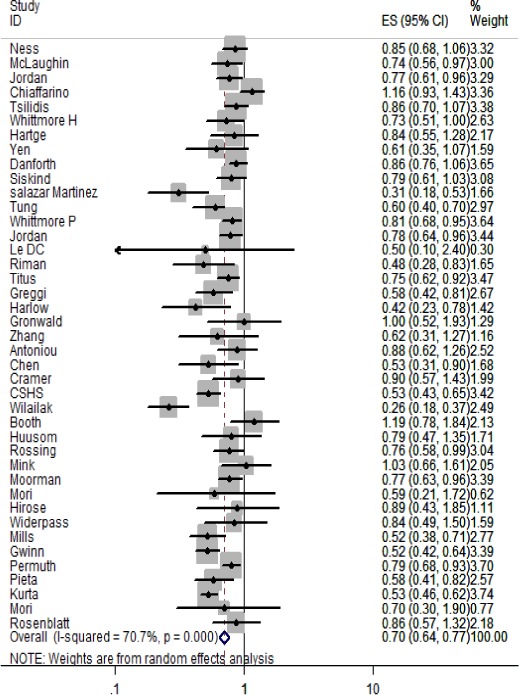
Effect on ever vs. never breastfeeding on risk of ovarian carcinoma.
In subgroup analysis, studies with sample sizes of more than 1500 showed a significant protection of 24% from ovarian carcinoma (OR 0.76, 95% CI 0.69–0.84). This effect size was reduced compared to studies with smaller samples (OR 0.67, 95% CI 0.53–0.84). Studies in HICs also showed a significant but reduced effect (OR 0.74, 95% CI 0.68–0.80) compared with studies in LMICs (OR 0.48 95% CI 0.29–0.77). Lower quality studies showed a higher risk reduction for ovarian carcinoma (OR 0.63, 95% CI 0.58–0.68) than higher quality studies (OR 0.72, 95% CI 0.65–0.80). Studies where fine adjustment for parity was made showed a modest but still significant (OR 0.80, 95% CI 0.75–0.86) reduction in risk of ovarian carcinoma compared with studies where no or crude adjustment for parity was made. In an analysis restricted to parous women in the fine adjustment subgroup, the effect was further attenuated (OR 0.82, 95% CI 0.75–0.89) (not shown in Table 2 ).
Osteoporosis
A total of six studies ( 174 – 179 ) were identified (Table 3 ). Two studies were from LMICs ( 174 , 178 ) and four studies from HICs ( 175 – 177 , 179 ). Bone mineral density (BMD) was generally measured at two sites, that is femoral neck and distal radius. For femoral neck, four studies ( 175 , 177 – 179 ) were identified with small sample size (total 489 women). The pooled effect suggests that breastfeeding had a nonsignificant effect on femoral neck bone mass. With respect to distal radius, four studies ( 174 – 177 ) were identified and the results were heterogeneous. The largest (n = 963) study ( 176 ) did not observe any association, whereas Chowdhury et al. ( 174 ) (n = 400) reported a negative effect of breastfeeding on bone mineral density. Overall, there was no clear evidence of an effect of breastfeeding on osteoporosis.
Association between breastfeeding and bone mineral density
BMD, bone mineral density; SD, standard deviation; SMD, standardised mean difference.
A recent systematic review by Aune reported a reduced risk of type 2 diabetes (RR 0.68 95% CI: 0.57–0.82) with longer duration of lifetime breastfeeding compared with shorter durations. A one-year increase in the total lifetime duration of breastfeeding was associated with 9% protection (RR 0.91, 95% CI: 0.86–0.96) against the presence of type 2 diabetes in the mothers. No new studies were found subsequent to the systemic review by Aune et al. in 2013.
Effects of breastfeeding on short-term maternal health outcomes
Lactational amenorrhoea.
We identified 12 studies ( 173 , 180 – 190 ) that examined the association between breastfeeding and lactational amenorrhoea (Table 4 ). Four studies ( 180 , 182 , 188 , 185 ) did not provide either RR or OR. They reported that exclusive compared to mixed feeding, or longer duration of any breastfeeding, was associated with an increased mean or median duration of lactational amenorrhoea. The remaining studies provided data from which the following estimates were derived: the probability of continued lactational amenorrhoea at six months postpartum was 23% higher (RR 1.23, 95% CI 1.07–1.41; three studies) for exclusive or predominant breastfeeding compared to no breastfeeding, and 21% higher (RR 1.21, 95% CI 1.01–1.25; five studies) (Table 4 ) when compared to partial breastfeeding. We found no evidence of publication bias.
Effect of breastfeeding on probability of lactational amenorrhoea
Postpartum depression
A recent systematic review conducted by Dias et al. reported that pregnancy depression predicts a shorter breastfeeding duration, but evidence is unclear on whether breastfeeding mediates the association between pregnancy and postpartum depression. No new studies were found subsequent to the systemic review conducted by Dias and Figueiredo in ( 32 ).
Postpartum weight change
We updated the systematic review by Neville et al. ( 33 ) by including 5 additional studies (Table 5 ) ( 191 – 195 ). In the review by Neville et al., the majority of identified studies reported little or no association between breastfeeding and weight change. Of those five studies, three studies were performed in low- and middle-income countries, one was performed in high-income country, and one was multicentre study (Brazil, Ghana, India, Norway, Oman, USA). In studies performed in low- and middle-income countries, we have not found any potential differential effect for breastfeeding and postpartum weight loss response as a function of countries being low to middle and high income. Two of the five additionally identified studies ( 194 , 195 ) reported a significant reduction in postpartum weight with breastfeeding. Sarkar and Taylor ( 191 ) in a cross-sectional study in Bangladesh revealed that body weight of mothers was negatively correlated with 1–12 and 13–24 months of lactation after controlling for height, education and food consumption. Stuebe et al. ( 192 ) showed that women who exclusively breastfed for greater than six months had the lowest BMI at 3 years postpartum as well as the lowest postpartum weight retention at 3 years compared with women who never exclusively breastfed. A multicentre study showed that lactation intensity and duration explained little variation in weight change patterns ( 193 – 195 ). Overall, the role of breastfeeding on postpartum weight change remains unclear.
Overview of studies which examined the association between breastfeeding and postpartum weight change
The aim of this review was to systematically examine the effect of breastfeeding on important maternal health outcomes.
The risk of developing breast carcinoma was reduced by 26% among women who cumulatively breastfed for more than 12 months, compared with women who did not breast feed.
Previous reviews suggested that breastfeeding was not strongly related to risk of breast carcinoma ( 196 , 197 ) or found a small but statistically significant protective association ( 198 – 200 ). Our meta-analysis findings are comparable with but suggest a higher level of protection than that found by the Collaborative Group on Hormonal Factors in Breast Carcinoma ( 201 ). In this pooled analysis of approximately 50 000 carcinoma cases from 47 studies in 30 countries around the world and after adjustment for confounders including parity and exclusion of nulliparous women, the authors estimated that the risk of invasive breast carcinoma decreased by 4.3% for every 12 months of breastfeeding ( 201 ). However, one of the challenges of comparing studies on cumulative breastfeeding duration and determining the effect on breast carcinoma risk is the lack of a standard protocol for grouping the lifetime number of months of breastfeeding for analysis and the adjustment of parity. Lifetime duration of breastfeeding is related to the number of children breastfed, that is parity and the duration of breastfeeding for each child. Our results showed that when controlled for parity, breastfeeding independently contributed to a modest but significant risk reduction for breast carcinoma. The risk reduction for breast carcinoma was 8% among ever breastfed mothers when finely adjusted for parity, while it was 22% when all studies were pooled together. Even when our analysis was restricted to only parous women, finely adjusted for parity, ever breastfeeding was associated with a 7% reduction in risk of breast carcinoma compared with never breastfeeding. Longer duration of breastfeeding (>12 months) was associated with more protection of breast carcinoma than shorter duration of breastfeeding (breastfeeding <6 and 6–12 months) when compared to never breastfeeding. Even when our analysis was restricted to studies with adequate quality, breastfeeding >12 months showed more protection against breast carcinoma. Possible biological mechanisms include that protection may occur through parity-specific changes in levels of circulating hormones such as estradiol, prolactin and growth hormone, as each of these has been associated with breast cancer risk ( 202 ), or that the parous mammary gland may contain epithelial cells with a more differentiated and less proliferative character which are less susceptible to transformation ( 203 ).
Breastfeeding by women for more than 12 months was also associated with a 35% reduction in ovarian cancer, compared with women who had not breastfed. The protective effect was less in women who had only ever breastfed (for any duration) ranging from 30% in an unadjusted analysis to 18% when the analysis was restricted to ever breastfeeding parous women (finely adjusted for parity). A number of physiological mechanisms may account for the protective effect of breastfeeding against ovarian cancer through modulating ovarian cycle length ( 204 ), and therefore, parity is an important confounder. Longer duration of breastfeeding suppresses ovulation longer and causes suppression of gonadotropins, resulting in depressed production of plasma estradiol, considered to be a potential causal mechanism of ovarian cancer when present at high levels ( 205 ). However, breastfeeding must also have an independent effect to explain the estimated reduction in ovarian cancer when parity is adjusted for.
There did not appear to be a significant effect of breastfeeding on the risk of osteoporosis. Calcium metabolism and bone metabolism are substantially altered during pregnancy and lactation, and high calcium demand during lactation makes women more prone to bone resorption and subsequent osteoporosis. There was no evidence of such risk, and it has been suggested that during lactation, oestrogen imposes minor inhibitory effect on periosteal bone formation and permits periosteal expansion which increases bone size after weaning ( 206 ).
Available review suggests that longer duration of breastfeeding reduces risk of development of type 2 diabetes mellitus by 32%, and in linear dose–response analyses, there was a 9% reduction in relative risk for each 12-month increase in lifetime duration of breastfeeding. Our review shows that exclusive or predominant breastfeeding during the first six months postpartum was associated with longer periods of amenorrhoea. Less intensive breastfeeding, captured under ‘any or partial breastfeeding’, offers less clear benefit. This finding is biologically plausible. Breastfeeding suppresses the resumption of ovarian activity after childbirth and is thus associated with a period of infertility. Exclusive breastfeeding and predominant breastfeeding are associated with a higher frequency of suckling than other patterns of breastfeeding. Frequent suckling inhibits gonadotropin-releasing hormone and decreases the release of luteinising hormone and follicle-stimulating hormone ( 207 ), thus preventing early return of menses.
The association between breastfeeding and postpartum weight change remains uncertain. Factors such as age, gestational weight gain and prepregnancy weight confound such analyses ( 208 , 209 ). As prepregnancy weight and gestational weight gain were found to be strong determinant factors of postpartum weight change, future research should include the preconception period with continued monitoring into the postpartum period to capture the true trajectory of weight change. Even though BF may not lead to postpartum weight loss under ‘natural’ conditions, it remains unknown whether women who wish to lose weight intentionally in the postpartum period are more likely to be successful at doing so if they are vs. if they are not breastfeeding.
Although our original review plans included exploring the associations between breastfeeding and the risk of maternal postpartum depression and type 2 diabetes, we were unable to identify new studies following the reviews published in 2015 ( 31 ) and 2013 ( 32 ). The evidence suggests that the relationship between breastfeeding and postpartum depression is lacking.
The range of the maternal outcomes examined and the various categories of breastfeeding exposures that we considered are important strengths of this review. Despite the expanded scope of review, other important maternal health outcomes such as maternal hypertension and cardiovascular disease were not addressed and should be considered in future research and reviews. Also important was the attempt to look for dose–response relationships and the evaluation of heterogeneity and publication biases. However, some limitations should be acknowledged. We have pooled data from many observational studies that are prone to be affected by biases such as in recall or due to selection. Some studies did not control for or collect information on potential confounders that could have affected the association between breastfeeding and the outcome of interest. For postpartum weight change, we were constrained to take a narrative approach to present the outcomes because of the heterogeneous nature of the studies. In cases of significant heterogeneity in study results, we have performed post hoc subgroup analysis and meta-regression and have used the random-effects model. But in some cases even within subgroups, there was significant heterogeneity which suggests some other unidentified factors causing such heterogeneity. Although the meta-regression seemed to explain around 80% of the heterogeneity for breast and ovarian carcinoma, we need to acknowledge the limitation of post hoc subgroup analysis.
Our meta-analysis shows that women who had ever breastfed and who breastfed for longer duration have a lower risk of breast and ovarian carcinoma and also type 2 diabetes mellitus. Exclusive or predominant breastfeeding during the first six months postpartum prolongs lactational amenorrhoea. We found no evidence of a clear association between breastfeeding and bone mineral density, maternal depression or postpartum weight change.
Acknowledgments
We are thankful to Dr. Cesar Victora, Universidade Federal de Pelotas, Pelotas, Brazil, for his guidance and feedback at different stages of this work. Centre for Health Research and Development, Society for Applied Studies (CHRD-SAS) is grateful for the core support from The Department of Child and Adolescent Health and Development, World Health Organization (Geneva), and The Centre for Intervention Science in Maternal and Child Health (RCN Project No. 223269), Centre for International Health, University of Bergen (Norway). We acknowledge the administrative and secretarial support extended by Ms. Nicola Mendes during manuscript preparation.
Confidence interval
High-income country
Low- and middle-income country
Medical Subject Heading
Randomised controlled trials
Relative risk
Standardised mean difference
United Nations Children's Fund
World Health Organization
Breastfeeding exposures (WHO definitions) ( 210 )
Summary of studies included in breast carcinoma
HIC, high-income country; LIC, low-income country; AQ, adequate quality; IQ, inadequate quality.
Summary of studies included in ovarian carcinoma
LIC, low-income country; AQ, adequate quality; IQ, inadequate quality.
Conflict of Interest
The authors have no financial relationships or other conflict of interests to disclose.
The authors alone are responsible for the views expressed in this article and they do not necessarily represent the views, decisions or policies of the institutions with which they are affiliated.
- 1. WHO. Infant and Young Child feeding. Model Chapter for textbooks for medical students and allied health professionals. Geneva: World Health Organization; 2009. [ PubMed ] [ Google Scholar ]
- 2. Brion MJ, Lawlor DA, Matijasevich A, Horta B, Anselmi L, Araujo CL, et al. What are the causal effects of breastfeeding on IQ, obesity and blood pressure? Evidence from comparing high-income with middle-income cohorts. Int J Epidemiol. 2011;40:670–80. doi: 10.1093/ije/dyr020. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 3. Gonzalez-Jimenez E, Garcia PA, Aguilar MJ, Padilla CA, Alvarez J. Breastfeeding and the prevention of breast cancer: a retrospective review of clinical histories. J Clin Nurs. 2014;23:2397–403. doi: 10.1111/jocn.12368. [ DOI ] [ PubMed ] [ Google Scholar ]
- 4. Ip S, Chung M, Raman G, Trikalinos TA, Lau J. A summary of the Agency for Healthcare Research and Quality's evidence report on breastfeeding in developed countries. Breastfeed Med. 2009;4(Suppl 1):S17–30. doi: 10.1089/bfm.2009.0050. [ DOI ] [ PubMed ] [ Google Scholar ]
- 5. Haiek LN, Kramer MS, Ciampi A, Tirado R. Postpartum weight loss and infant feeding. J Am Board Fam Pract. 2001;14:85–94. [ PubMed ] [ Google Scholar ]
- 6. Ebina S, Kashiwakura I. Influence of breastfeeding on maternal blood pressure at one month postpartum Int. J Womens Health. 2012;4:333–9. doi: 10.2147/IJWH.S33379. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 7. Lipworth L, Bailey LR, Trichopoulos D. History of breast-feeding in relation to breast cancer risk: a review of the epidemiologic literature. J Natl Cancer Inst. 2000;92:302–12. doi: 10.1093/jnci/92.4.302. [ DOI ] [ PubMed ] [ Google Scholar ]
- 8. Britt K, Ashworth A, Smalley M. Pregnancy and the risk of breast cancer. Endocr Relat Cancer. 2007;14:907–33. doi: 10.1677/ERC-07-0137. [ DOI ] [ PubMed ] [ Google Scholar ]
- 9. Siegel R, Naishadham D, Jemal A. Cancer statistics, 2012. CA Cancer J Clin. 2012;62:10–29. doi: 10.3322/caac.20138. [ DOI ] [ PubMed ] [ Google Scholar ]
- 10. Bray F, Loos AH, Tognazzo S, La Vecchia C. Ovarian cancer in Europe: cross-sectional trends in incidence and mortality in 28 countries, 1953-2000. Int J Cancer. 2005;113:977–90. doi: 10.1002/ijc.20649. [ DOI ] [ PubMed ] [ Google Scholar ]
- 11. Sueblinvong T, Carney ME. Current understanding of risk factors for ovarian cancer. Curr Treat Options Oncol. 2009;10:67–81. doi: 10.1007/s11864-009-0108-2. [ DOI ] [ PubMed ] [ Google Scholar ]
- 12. Whittemore AS, Harris R, Itnyre J. Characteristics relating to ovarian cancer risk: collaborative analysis of 12 US case-control studies. IV. The pathogenesis of epithelial ovarian cancer. Collaborative Ovarian Cancer Group. Am J Epidemiol. 1992;136:1212–20. doi: 10.1093/oxfordjournals.aje.a116429. [ DOI ] [ PubMed ] [ Google Scholar ]
- 13. Kovacs CS, Kronenberg HM. Maternal-fetal calcium and bone metabolism during pregnancy, puerperium, and lactation. Endocr Rev. 1997;18:832–72. doi: 10.1210/edrv.18.6.0319. [ DOI ] [ PubMed ] [ Google Scholar ]
- 14. Stuebe AM, Rich-Edwards JW, Willett WC, Manson JE, Michels KB. Duration of lactation and incidence of type 2 diabetes. JAMA. 2005;294:2601–10. doi: 10.1001/jama.294.20.2601. [ DOI ] [ PubMed ] [ Google Scholar ]
- 15. Schwarz EB, Brown JS, Creasman JM, Stuebe A, McClure CK, Van Den Eeden SK, et al. Lactation and maternal risk of type 2 diabetes: a population-based study. Am J Med. 2010;123:863. doi: 10.1016/j.amjmed.2010.03.016. e1–6. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 16. Gray RH, Campbell OM, Apelo R, Eslami SS, Zacur H, Ramos RM, et al. Risk of ovulation during lactation. Lancet. 1990;335:25–9. doi: 10.1016/0140-6736(90)90147-w. [ DOI ] [ PubMed ] [ Google Scholar ]
- 17. Andersen AN, Schioler V. Influence of breast-feeding pattern on pituitary-ovarian axis of women in an industrialized community. Am J Obstet Gynecol. 1982;143:673–7. doi: 10.1016/0002-9378(82)90113-2. [ DOI ] [ PubMed ] [ Google Scholar ]
- 18. Rivera R, Kennedy KI, Ortiz E, Barrera M, Bhiwandiwala PP. Breast-feeding and the return to ovulation in Durango, Mexico. Fertil Steril. 1988;49:780–7. [ PubMed ] [ Google Scholar ]
- 19. Diaz S, Rodriguez G, Peralta O, Miranda P, Casado ME, Salvatierra AM, et al. Lactational amenorrhea and the recovery of ovulation and fertility in fully nursing Chilean women. Contraception. 1988;38:53–67. doi: 10.1016/0010-7824(88)90095-9. [ DOI ] [ PubMed ] [ Google Scholar ]
- 20. Halbreich U, Karkun S. Cross-cultural and social diversity of prevalence of postpartum depression and depressive symptoms. J Affect Disord. 2006;91:97–111. doi: 10.1016/j.jad.2005.12.051. [ DOI ] [ PubMed ] [ Google Scholar ]
- 21. Josefsson A, Sydsjo G. A follow-up study of postpartum depressed women: recurrent maternal depressive symptoms and child behavior after four years. Arch Womens Ment Health. 2007;10:141–5. doi: 10.1007/s00737-007-0185-9. [ DOI ] [ PubMed ] [ Google Scholar ]
- 22. Pincus HA, Pettit AR. The societal costs of chronic major depression. J Clin Psychiatry. 2001;62(Suppl 6):5–9. [ PubMed ] [ Google Scholar ]
- 23. Ystrom E. Breastfeeding cessation and symptoms of anxiety and depression: a longitudinal cohort study. BMC Pregnancy Childbirth. 2012;12:36. doi: 10.1186/1471-2393-12-36. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 24. Chung EK, McCollum KF, Elo IT, Lee HJ, Culhane JF. Maternal depressive symptoms and infant health practices among low-income women. Pediatrics. 2004;113:e523–9. doi: 10.1542/peds.113.6.e523. [ DOI ] [ PubMed ] [ Google Scholar ]
- 25. Linne Y, Barkeling B, Rossner S. Long-term weight development after pregnancy. Obes Rev. 2002;3:75–83. doi: 10.1046/j.1467-789x.2002.00061.x. [ DOI ] [ PubMed ] [ Google Scholar ]
- 26. Rooney BL, Schauberger CW, Mathiason MA. Impact of perinatal weight change on long-term obesity and obesity-related illnesses. Obstet Gynecol. 2005;106:1349–56. doi: 10.1097/01.AOG.0000185480.09068.4a. [ DOI ] [ PubMed ] [ Google Scholar ]
- 27. Stuebe AM, Rich-Edwards JW. The reset hypothesis: lactation and maternal metabolism. Am J Perinatol. 2009;26:81–8. doi: 10.1055/s-0028-1103034. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 28. Excellence NIoHaC. Donor milk banks: the operation of donor milk bank services. NICE 2010. Available at https://www.nice.org.uk/guidance/cg93 (Last accessed on: 10 March 2015) [ PubMed ] [ Google Scholar ]
- 29. Lefebvre C, Manheimer E, Glanville J. Searching for studies. In: Higgins JPT, Greene S, editors. Cochrane Handbook for Systematic Reviews of Interventions, Version 5.0. The Cochrane Collaboration; 2008. Available at: http://www.cochrane-handbook.org.2008 (accessed on March 10, 2015) [ Google Scholar ]
- 30. Luan NN, Wu QJ, Gong TT, Vogtmann E, Wang YL, Lin B. Breastfeeding and ovarian cancer risk: a meta-analysis of epidemiologic studies. Am J Clin Nutr. 2013;98:1020–31. doi: 10.3945/ajcn.113.062794. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 31. Aune D, Norat T, Romundstad P, Vatten LJ. Breastfeeding and the maternal risk of type 2 diabetes: a systematic review and dose-response meta-analysis of cohort studies. Nutr Metab Cardiovasc Dis. 2014;24:107–15. doi: 10.1016/j.numecd.2013.10.028. [ DOI ] [ PubMed ] [ Google Scholar ]
- 32. Dias CC, Figueiredo B. Breastfeeding and depression: a systematic review of the literature. J Affect Disord. 2015;171:142–54. doi: 10.1016/j.jad.2014.09.022. [ DOI ] [ PubMed ] [ Google Scholar ]
- 33. Neville CE, McKinley MC, Holmes VA, Spence D, Woodside JV. The relationship between breastfeeding and postpartum weight change–a systematic review and critical evaluation. Int J Obes (Lond) 2014;38:577–90. doi: 10.1038/ijo.2013.132. [ DOI ] [ PubMed ] [ Google Scholar ]
- 34. Harris R, Bradburn M, Deeks J, Harbord R, Altman D, Sterne J. metan: fixed- and random-effects meta-analysis. Stata J. 2008;8:3–28. [ Google Scholar ]
- 35. World Bank. Low and middle income country data. World Bank 2014; 2014. [ Google Scholar ]
- 36. Sterne JAC, Higgins JPT Reeves BC on behalf of the Development Group for ACROBAT-NRSI. A Cochrane Risk of Bias Assessment Tool: for Non-Randomized Studies of Interventions (ACROBAT-NRSI), Version 1.0.0, 24.
- 37. Sterne JAC, Egger M, Smith GD. Investigating and Dealing with Publication and Other Biases, in Systematic Reviews in Health Care: Meta-Analysis in Context. 2nd ed. London: BMJ Publishing Group; 2001. pp. 189–208. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 38. United Kingdom National Case-Control Study Group. Breast feeding and risk of breast cancer in young women. United Kingdom National Case-Control Study Group. BMJ. 1993;307:17–20. doi: 10.1136/bmj.307.6895.17. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 39. Adami HO, Bergstrom R, Lund E, Meirik O. Absence of association between reproductive variables and the risk of breast cancer in young women in Sweden and Norway. Br J Cancer. 1990;62:122–6. doi: 10.1038/bjc.1990.242. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 40. Akbari A, Razzaghi Z, Homaee F, Khayamzadeh M, Movahedi M, Akbari ME. Parity and breastfeeding are preventive measures against breast cancer in Iranian women. Breast Cancer. 2011;18:51–5. doi: 10.1007/s12282-010-0203-z. [ DOI ] [ PubMed ] [ Google Scholar ]
- 41. Ambrosone CB, Zirpoli G, Ruszczyk M, Shankar J, Hong CC, McIlwain D, et al. Parity and breastfeeding among African-American women: differential effects on breast cancer risk by estrogen receptor status in the Women's Circle of Health Study. Cancer Causes Control. 2014;25:259–65. doi: 10.1007/s10552-013-0323-9. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 42. Andrieu N, Goldgar DE, Easton DF, Rookus M, Brohet R, Antoniou AC, et al. Pregnancies, breast-feeding, and breast cancer risk in the International BRCA1/2 Carrier Cohort Study (IBCCS) J Natl Cancer Inst. 2006;98:535–44. doi: 10.1093/jnci/djj132. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 43. Awatef M, Olfa G, Imed H, Kacem M, Imen C, Rim C, et al. Breastfeeding reduces breast cancer risk: a case-control study in Tunisia. Cancer Causes Control. 2010;21:393–7. doi: 10.1007/s10552-009-9471-3. [ DOI ] [ PubMed ] [ Google Scholar ]
- 44. Bao PP, Shu XO, Gao YT, Zheng Y, Cai H, Deming SL, et al. Association of hormone-related characteristics and breast cancer risk by estrogen receptor/progesterone receptor status in the shanghai breast cancer study. Am J Epidemiol. 2011;174:661–71. doi: 10.1093/aje/kwr145. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 45. Barba M, McCann SE, Nie J, Vito D, Stranges S, Fuhrman B, et al. Perinatal exposures and breast cancer risk in the Western New York Exposures and Breast Cancer (WEB) Study. Cancer Causes Control. 2006;17:395–401. doi: 10.1007/s10552-005-0481-5. [ DOI ] [ PubMed ] [ Google Scholar ]
- 46. Brignone G, Cusimano R, Dardanoni G, Gugliuzza M, Lanzarone F, Scibilia V, et al. A case-control study on breast cancer risk factors in a southern European population. Int J Epidemiol. 1987;16:356–61. doi: 10.1093/ije/16.3.356. [ DOI ] [ PubMed ] [ Google Scholar ]
- 47. Brinton LA, Hoover R, Fraumeni JF., Jr Reproductive factors in the aetiology of breast cancer. Br J Cancer. 1983;47:757–62. doi: 10.1038/bjc.1983.128. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 48. Brinton LA, Potischman NA, Swanson CA, Schoenberg JB, Coates RJ, Gammon MD, et al. Breastfeeding and breast cancer risk. Cancer Causes Control. 1995;6:199–208. doi: 10.1007/BF00051791. [ DOI ] [ PubMed ] [ Google Scholar ]
- 49. Butt Z, Haider SF, Arif S, Khan MR, Ashfaq U, Shahbaz U, et al. Breast cancer risk factors: a comparison between pre-menopausal and post-menopausal women. J Pak Med Assoc. 2012;62:120–4. [ PubMed ] [ Google Scholar ]
- 50. Calderon-Garciduenas AL, Paras-Barrientos FU, Cardenas-Ibarra L, Gonzalez-Guerrero JF, Villarreal-Rios E, Staines-Boone T, et al. Risk factors of breast cancer in Mexican women. Salud Publica Mex. 2000;42:26–33. doi: 10.1590/s0036-36342000000100006. [ DOI ] [ PubMed ] [ Google Scholar ]
- 51. Chang-Claude J, Eby N, Kiechle M, Bastert G, Becher H. Breastfeeding and breast cancer risk by age 50 among women in Germany. Cancer Causes Control. 2000;11:687–95. doi: 10.1023/a:1008907901087. [ DOI ] [ PubMed ] [ Google Scholar ]
- 52. Chung S, Park SK, Sung H, Song N, Han W, Noh DY, et al. Association between chronological change of reproductive factors and breast cancer risk defined by hormone receptor status: results from the Seoul Breast Cancer Study. Breast Cancer Res Treat. 2013;140:557–65. doi: 10.1007/s10549-013-2645-4. [ DOI ] [ PubMed ] [ Google Scholar ]
- 53. Coogan PF, Rosenberg L, Shapiro S, Hoffman M. Lactation and breast carcinoma risk in a South African population. Cancer. 1999;86:982–9. doi: 10.1002/(sici)1097-0142(19990915)86:6<982::aid-cncr13>3.0.co;2-b. [ DOI ] [ PubMed ] [ Google Scholar ]
- 54. De Silva M, Senarath U, Gunatilake M, Lokuhetty D. Prolonged breastfeeding reduces risk of breast cancer in Sri Lankan women: a case-control study. Cancer Epidemiol. 2010;34:267–73. doi: 10.1016/j.canep.2010.02.012. [ DOI ] [ PubMed ] [ Google Scholar ]
- 55. Duffy SW, Roberts MM, Elton RA. Risk factors for breast cancer: relevance to screening. J Epidemiol Community Health. 1983;37:127–31. doi: 10.1136/jech.37.2.127. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 56. Enger SM, Ross RK, Henderson B, Bernstein L. Breastfeeding history, pregnancy experience and risk of breast cancer. Br J Cancer. 1997;76:118–23. doi: 10.1038/bjc.1997.346. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 57. Enger SM, Ross RK, Paganini-Hill A, Bernstein L. Breastfeeding experience and breast cancer risk among postmenopausal women. Cancer Epidemiol Biomarkers Prev. 1998;7:365–9. [ PubMed ] [ Google Scholar ]
- 58. Faheem M, Khurram M, Jafri IA, Mehmood H, Hasan Z, Iqbal GS, et al. Risk factors for breast cancer in patients treated at NORI Hospital, Islamabad. J Pak Med Assoc. 2007;57:242–5. [ PubMed ] [ Google Scholar ]
- 59. Freudenheim JL, Marshall JR, Vena JE, Moysich KB, Muti P, Laughlin R, et al. Lactation history and breast cancer risk. Am J Epidemiol. 1997;146:932–8. doi: 10.1093/oxfordjournals.aje.a009219. [ DOI ] [ PubMed ] [ Google Scholar ]
- 60. Furberg H, Newman B, Moorman P, Millikan R. Lactation and breast cancer risk. Int J Epidemiol. 1999;28:396–402. doi: 10.1093/ije/28.3.396. [ DOI ] [ PubMed ] [ Google Scholar ]
- 61. Gajalakshmi V, Mathew A, Brennan P, Rajan B, Kanimozhi VC, Mathews A, et al. Breastfeeding and breast cancer risk in India: a multicenter case-control study. Int J Cancer. 2009;125:662–5. doi: 10.1002/ijc.24429. [ DOI ] [ PubMed ] [ Google Scholar ]
- 62. Gammon MD, Neugut AI, Santella RM, Teitelbaum SL, Britton JA, Terry MB, et al. The Long Island Breast Cancer Study Project: description of a multi-institutional collaboration to identify environmental risk factors for breast cancer. Breast Cancer Res Treat. 2002;74:235–54. doi: 10.1023/a:1016387020854. [ DOI ] [ PubMed ] [ Google Scholar ]
- 63. Gao YT, Shu XO, Dai Q, Potter JD, Brinton LA, Wen W, et al. Association of menstrual and reproductive factors with breast cancer risk: results from the Shanghai Breast Cancer Study. Int J Cancer. 2000;87:295–300. doi: 10.1002/1097-0215(20000715)87:2<295::aid-ijc23>3.0.co;2-7. [ DOI ] [ PubMed ] [ Google Scholar ]
- 64. Gilliland FD, Hunt WC, Baumgartner KB, Crumley D, Nicholson CS, Fetherolf J, et al. Reproductive risk factors for breast cancer in Hispanic and non-Hispanic white women: the New Mexico Women's Health Study. Am J Epidemiol. 1998;148:683–92. doi: 10.1093/aje/148.7.683. [ DOI ] [ PubMed ] [ Google Scholar ]
- 65. Gronwald J, Byrski T, Huzarski T, Cybulski C, Sun P, Tulman A, et al. Influence of selected lifestyle factors on breast and ovarian cancer risk in BRCA1 mutation carriers from Poland. Breast Cancer Res Treat. 2006;95:105–9. doi: 10.1007/s10549-005-9051-5. [ DOI ] [ PubMed ] [ Google Scholar ]
- 66. Hadjisavvas A, Loizidou MA, Middleton N, Michael T, Papachristoforou R, Kakouri E, et al. An investigation of breast cancer risk factors in Cyprus: a case control study. BMC Cancer. 2010;10:447. doi: 10.1186/1471-2407-10-447. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 67. Hajian-Tilaki KO, Kaveh-Ahangar T. Reproductive factors associated with breast cancer risk in northern Iran. Med Oncol. 2011;28:441–6. doi: 10.1007/s12032-010-9498-z. [ DOI ] [ PubMed ] [ Google Scholar ]
- 68. Hejar AR, Chong FB, Rosnan H, Zailina H. Breast cancer and lifestyle risks among Chinese women in the Klang Valley in 2001. Med J Malaysia. 2004;59:226–32. [ PubMed ] [ Google Scholar ]
- 69. Hirose K, Tajima K, Hamajima N, Kuroishi T, Kuzuya K, Miura S, et al. Comparative case-referent study of risk factors among hormone-related female cancers in Japan. Jpn J Cancer Res. 1999;90:255–61. doi: 10.1111/j.1349-7006.1999.tb00741.x. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 70. Huang WY, Newman B, Millikan RC, Conway K, Hulka BS, Schell MJ, et al. Risk of breast cancer according to the status of HER-2/neu oncogene amplification. Cancer Epidemiol Biomarkers Prev. 2000;9:65–71. [ PubMed ] [ Google Scholar ]
- 71. Inumaru LE, Irineu Gomes Duarte Quintanilha M, Aparecida da Silveira E, Veloso Naves MM. Risk and protective factors for breast cancer in Midwest of Brazil. J Environ Public Health. 2012;2012:356851. doi: 10.1155/2012/356851. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 72. Iwasaki M, Otani T, Inoue M, Sasazuki S, Tsugane S. Role and impact of menstrual and reproductive factors on breast cancer risk in Japan. Eur J Cancer Prev. 2007;16:116–23. doi: 10.1097/01.cej.0000228410.14095.2d. [ DOI ] [ PubMed ] [ Google Scholar ]
- 73. Kamarudin R, Shah SA, Hidayah N. Lifestyle factors and breast cancer: a case-control study in Kuala Lumpur, Malaysia. Asian Pac J Cancer Prev. 2006;7:51–4. [ PubMed ] [ Google Scholar ]
- 74. Katsouyanni K, Lipworth L, Trichopoulou A, Samoli E, Stuver S, Trichopoulos D. A case-control study of lactation and cancer of the breast. Br J Cancer. 1996;73:814–8. doi: 10.1038/bjc.1996.143. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 75. Kawai M, Minami Y, Kuriyama S, Kakizaki M, Kakugawa Y, Nishino Y, et al. Reproductive factors, exogenous female hormone use and breast cancer risk in Japanese: the Miyagi Cohort Study. Cancer Causes Control. 2010;21:135–45. doi: 10.1007/s10552-009-9443-7. [ DOI ] [ PubMed ] [ Google Scholar ]
- 76. Kim Y, Choi JY, Lee KM, Park SK, Ahn SH, Noh DY, et al. Dose-dependent protective effect of breast-feeding against breast cancer among ever-lactated women in Korea. Eur J Cancer Prev. 2007;16:124–9. doi: 10.1097/01.cej.0000228400.07364.52. [ DOI ] [ PubMed ] [ Google Scholar ]
- 77. Kishk NA. Breast cancer in relation to some reproductive factors. J Egypt Public Health Assoc. 1999;74:547–66. [ PubMed ] [ Google Scholar ]
- 78. Kruk J. Association of lifestyle and other risk factors with breast cancer according to menopausal status: a case-control study in the Region of Western Pomerania (Poland) Asian Pac J Cancer Prev. 2007;8:513–24. [ PubMed ] [ Google Scholar ]
- 79. Kuru B, Ozaslan C, Ozdemir P, Dinc S, Camlibel M, Alagol H. Risk factors for breast cancer in Turkish women with early pregnancies and long-lasting lactation–a case-control study. Acta Oncol. 2002;41:556–61. doi: 10.1080/02841860214964. [ DOI ] [ PubMed ] [ Google Scholar ]
- 80. Layde PM, Webster LA, Baughman AL, Wingo PA, Rubin GL, Ory HW. The independent associations of parity, age at first full term pregnancy, and duration of breastfeeding with the risk of breast cancer. Cancer and Steroid Hormone Study Group. J Clin Epidemiol. 1989;42:963–73. doi: 10.1016/0895-4356(89)90161-3. [ DOI ] [ PubMed ] [ Google Scholar ]
- 81. Lee HP, Gourley L, Duffy SW, Esteve J, Lee J, Day NE. Risk factors for breast cancer by age and menopausal status: a case-control study in Singapore. Cancer Causes Control. 1992;3:313–22. doi: 10.1007/BF00146884. [ DOI ] [ PubMed ] [ Google Scholar ]
- 82. Lee SY, Kim MT, Kim SW, Song MS, Yoon SJ. Effect of lifetime lactation on breast cancer risk: a Korean women's cohort study. Int J Cancer. 2003;105:390–3. doi: 10.1002/ijc.11078. [ DOI ] [ PubMed ] [ Google Scholar ]
- 83. Li CI, Beaber EF, Tang MT, Porter PL, Daling JR, Malone KE. Reproductive factors and risk of estrogen receptor positive, triple-negative, and HER2-neu overexpressing breast cancer among women 20-44 years of age. Breast Cancer Res Treat. 2013;137:579–87. doi: 10.1007/s10549-012-2365-1. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 84. Liu YT, Gao CM, Ding JH, Li SP, Cao HX, Wu JZ, et al. Physiological, reproductive factors and breast cancer risk in Jiangsu province of China. Asian Pac J Cancer Prev. 2011;12:787–90. [ PubMed ] [ Google Scholar ]
- 85. London SJ, Colditz GA, Stampfer MJ, Willett WC, Rosner BA, Corsano K, et al. Lactation and risk of breast cancer in a cohort of US women. Am J Epidemiol. 1990;132:17–26. doi: 10.1093/oxfordjournals.aje.a115629. [ DOI ] [ PubMed ] [ Google Scholar ]
- 86. Lord SJ, Bernstein L, Johnson KA, Malone KE, McDonald JA, Marchbanks PA, et al. Breast cancer risk and hormone receptor status in older women by parity, age of first birth, and breastfeeding: a case-control study. Cancer Epidemiol Biomarkers Prev. 2008;17:1723–30. doi: 10.1158/1055-9965.EPI-07-2824. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 87. Lumachi F, Ermani M, Brandes AA, Basso U, Paris M, Basso SM, et al. Breast cancer risk in healthy and symptomatic women: results of a multivariate analysis. A case-control study. Biomed Pharmacother. 2002;56:416–20. doi: 10.1016/s0753-3322(02)00252-4. [ DOI ] [ PubMed ] [ Google Scholar ]
- 88. MacMahon B, Purde M, Cramer D, Hint E. Association of breast cancer risk with age at first and subsequent births: a study in the population of the Estonian Republic. J Natl Cancer Inst. 1982;69:1035–8. [ PubMed ] [ Google Scholar ]
- 89. Mahouri K, Dehghani Zahedani M, Zare S. Breast cancer risk factors in south of Islamic Republic of Iran: a case-control study. East Mediterr Health J. 2007;13:1265–73. doi: 10.26719/2007.13.6.1265. [ DOI ] [ PubMed ] [ Google Scholar ]
- 90. Marcus PM, Baird DD, Millikan RC, Moorman PG, Qaqish B, Newman B. Adolescent reproductive events and subsequent breast cancer risk. Am J Public Health. 1999;89:1244–7. doi: 10.2105/ajph.89.8.1244. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 91. Matalqah L, Radaideh K, Yusoff ZM, Awaisu A. Predictors of breast cancer among women in a northern state of Malaysia: a matched case-control study. Asian Pac J Cancer Prev. 2011;12:1549–53. [ PubMed ] [ Google Scholar ]
- 92. McKenzie F, Ellison-Loschmann L, Jeffreys M, Firestone R, Pearce N, Romieu I. Healthy lifestyle and risk of breast cancer for indigenous and non-indigenous women in New Zealand: a case control study. BMC Cancer. 2014;14:12. doi: 10.1186/1471-2407-14-12. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 93. McTiernan A, Thomas DB, Johnson LK, Roseman D. Risk factors for estrogen receptor-rich and estrogen receptor-poor breast cancers. J Natl Cancer Inst. 1986;77:849–54. [ PubMed ] [ Google Scholar ]
- 94. Meeske K, Press M, Patel A, Bernstein L. Impact of reproductive factors and lactation on breast carcinoma in situ risk. Int J Cancer. 2004;110:102–9. doi: 10.1002/ijc.20072. [ DOI ] [ PubMed ] [ Google Scholar ]
- 95. Michels KB, Willett WC, Rosner BA, Manson JE, Hunter DJ, Colditz GA, et al. Prospective assessment of breastfeeding and breast cancer incidence among 89,887 women. Lancet. 1996;347:431–6. doi: 10.1016/s0140-6736(96)90010-0. [ DOI ] [ PubMed ] [ Google Scholar ]
- 96. Minami Y, Ohuchi N, Fukao A, Hisamichi S. Risk factors for breast cancer: a case-control study of screen-detected breast cancer in Miyagi Prefecture, Japan. Breast Cancer Res Treat. 1997;44:225–33. doi: 10.1023/a:1005883221114. [ DOI ] [ PubMed ] [ Google Scholar ]
- 97. Morales L, Alvarez-Garriga C, Matta J, Ortiz C, Vergne Y, Vargas W, et al. Factors associated with breast cancer in Puerto Rican women. J Epidemiol Glob Health. 2013;3:205–15. doi: 10.1016/j.jegh.2013.08.003. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 98. Negri E, Braga C, La Vecchia C, Levi F, Talamini R, Franceschi S. Lactation and the risk of breast cancer in an Italian population. Int J Cancer. 1996;67:161–4. doi: 10.1002/(SICI)1097-0215(19960717)67:2<161::AID-IJC1>3.0.CO;2-R. [ DOI ] [ PubMed ] [ Google Scholar ]
- 99. Newcomb PA, Storer BE, Longnecker MP, Mittendorf R, Greenberg ER, Clapp RW, et al. Lactation and a reduced risk of premenopausal breast cancer. N Engl J Med. 1994;330:81–7. doi: 10.1056/NEJM199401133300201. [ DOI ] [ PubMed ] [ Google Scholar ]
- 100. Olaya-Contreras P, Pierre B, Lazcano-Ponce E, Villamil-Rodriguez J, Posso-Valencia HJ. [Reproductive risk factors associated with breast cancer in Colombian women] Rev Saude Publica. 1999;33:237–45. doi: 10.1590/s0034-89101999000300004. [ DOI ] [ PubMed ] [ Google Scholar ]
- 101. Oran B, Celik I, Erman M, Baltali E, Zengin N, Demirkazik F, et al. Analysis of menstrual, reproductive, and life-style factors for breast cancer risk in Turkish women: a case-control study. Med Oncol. 2004;21:31–40. doi: 10.1385/MO:21:1:31. [ DOI ] [ PubMed ] [ Google Scholar ]
- 102. Ortiz Mendoza CM, Galvan Martinez EA. [Reproductive risk factors of breast cancer in patients attended at a second level urban hospital] Ginecol Obstet Mex. 2007;75:11–6. [ PubMed ] [ Google Scholar ]
- 103. Ozmen V, Ozcinar B, Karanlik H, Cabioglu N, Tukenmez M, Disci R, et al. Breast cancer risk factors in Turkish women–a University Hospital based nested case control study. World J Surg Oncol. 2009;7:37. doi: 10.1186/1477-7819-7-37. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 104. Palmer JR, Viscidi E, Troester MA, Hong CC, Schedin P, Bethea TN, et al. Parity, lactation, and breast cancer subtypes in African American women: results from the AMBER Consortium. J Natl Cancer Inst. 2014;106:1–8. doi: 10.1093/jnci/dju237. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 105. Paul C, Skegg DC, Spears GF. Oral contraceptives and risk of breast cancer. Int J Cancer. 1990;46:366–73. doi: 10.1002/ijc.2910460305. [ DOI ] [ PubMed ] [ Google Scholar ]
- 106. Peterson NB, Huang Y, Newcomb PA, Titus-Ernstoff L, Trentham-Dietz A, Anic G, et al. Childbearing recency and modifiers of premenopausal breast cancer risk. Cancer Epidemiol Biomarkers Prev. 2008;17:3284–7. doi: 10.1158/1055-9965.EPI-08-0577. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 107. Phipps AI, Chlebowski RT, Prentice R, McTiernan A, Wactawski-Wende J, Kuller LH, et al. Reproductive history and oral contraceptive use in relation to risk of triple-negative breast cancer. J Natl Cancer Inst. 2011;103:470–7. doi: 10.1093/jnci/djr030. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 108. Purwanto H, Sadjimin T, Dwiprahasto I. Lactation and the risk of breast cancer. Gan To Kagaku Ryoho. 2000;27(Suppl 2):474–81. [ PubMed ] [ Google Scholar ]
- 109. Rao DN, Ganesh B, Desai PB. Role of reproductive factors in breast cancer in a low-risk area: a case-control study. Br J Cancer. 1994;70:129–32. doi: 10.1038/bjc.1994.261. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 110. Romieu I, Hernandez-Avila M, Lazcano E, Lopez L, Romero-Jaime R. Breast cancer and lactation history in Mexican women. Am J Epidemiol. 1996;143:543–52. doi: 10.1093/oxfordjournals.aje.a008784. [ DOI ] [ PubMed ] [ Google Scholar ]
- 111. Rookus MA, van Leeuwen FE. Oral contraceptives and risk of breast cancer in women aged 20-54 years. Netherlands Oral Contraceptives and Breast Cancer Study Group. Lancet. 1994;344:844–51. doi: 10.1016/s0140-6736(94)92826-6. [ DOI ] [ PubMed ] [ Google Scholar ]
- 112. Shantakumar S, Terry MB, Teitelbaum SL, Britton JA, Millikan RC, Moorman PG, et al. Reproductive factors and breast cancer risk among older women. Breast Cancer Res Treat. 2007;102:365–74. doi: 10.1007/s10549-006-9343-4. [ DOI ] [ PubMed ] [ Google Scholar ]
- 113. Shema L, Ore L, Ben-Shachar M, Haj M, Linn S. The association between breastfeeding and breast cancer occurrence among Israeli Jewish women: a case control study. J Cancer Res Clin Oncol. 2007;133:539–46. doi: 10.1007/s00432-007-0199-8. [ DOI ] [ PubMed ] [ Google Scholar ]
- 114. Siskind V, Schofield F, Rice D, Bain C. Breast cancer and breastfeeding: results from an Australian case-control study. Am J Epidemiol. 1989;130:229–36. doi: 10.1093/oxfordjournals.aje.a115329. [ DOI ] [ PubMed ] [ Google Scholar ]
- 115. Stuebe AM, Willett WC, Xue F, Michels KB. Lactation and incidence of premenopausal breast cancer: a longitudinal study. Arch Intern Med. 2009;169:1364–71. doi: 10.1001/archinternmed.2009.231. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 116. Stuver SO, Hsieh CC, Bertone E, Trichopoulos D. The association between lactation and breast cancer in an international case-control study: a re-analysis by menopausal status. Int J Cancer. 1997;71:166–9. doi: 10.1002/(sici)1097-0215(19970410)71:2<166::aid-ijc7>3.0.co;2-z. [ DOI ] [ PubMed ] [ Google Scholar ]
- 117. Sugawara Y, Kakizaki M, Nagai M, Tomata Y, Hoshi R, Watanabe I, et al. Lactation pattern and the risk for hormone-related female cancer in Japan: the Ohsaki Cohort Study. Eur J Cancer Prev. 2013;22:187–92. doi: 10.1097/CEJ.0b013e3283564610. [ DOI ] [ PubMed ] [ Google Scholar ]
- 118. Tao SC, Yu MC, Ross RK, Xiu KW. Risk factors for breast cancer in Chinese women of Beijing. Int J Cancer. 1988;42:495–8. doi: 10.1002/ijc.2910420404. [ DOI ] [ PubMed ] [ Google Scholar ]
- 119. Tessaro S, Beria JU, Tomasi E, Victora CG. Breastfeeding and breast cancer: a case-control study in Southern Brazil. Cad Saude Publica. 2003;19:1593–601. doi: 10.1590/s0102-311x2003000600004. [ DOI ] [ PubMed ] [ Google Scholar ]
- 120. Thomas DB, Noonan EA. Breast cancer and prolonged lactation. The WHO Collaborative Study of Neoplasia and Steroid Contraceptives. Int J Epidemiol. 1993;22:619–26. doi: 10.1093/ije/22.4.619. [ DOI ] [ PubMed ] [ Google Scholar ]
- 121. Tryggvadottir L, Tulinius H, Eyfjord JE, Sigurvinsson T. Breastfeeding and reduced risk of breast cancer in an Icelandic cohort study. Am J Epidemiol. 2001;154:37–42. doi: 10.1093/aje/154.1.37. [ DOI ] [ PubMed ] [ Google Scholar ]
- 122. Ursin G, Bernstein L, Wang Y, Lord SJ, Deapen D, Liff JM, et al. Reproductive factors and risk of breast carcinoma in a study of white and African-American women. Cancer. 2004;101:353–62. doi: 10.1002/cncr.20373. [ DOI ] [ PubMed ] [ Google Scholar ]
- 123. Wakai K, Ohno Y, Watanabe S, Sakamoto G, Kasumi F, Suzuki S, et al. Risk factors for breast cancer among Japanese women in Tokyo: a case-control study. J Epidemiol. 1994;4:65–71. [ Google Scholar ]
- 124. Wang QS, Ross RK, Yu MC, Ning JP, Henderson BE, Kimm HT. A case-control study of breast cancer in Tianjin, China. Cancer Epidemiol Biomarkers Prev. 1992;1:435–9. [ PubMed ] [ Google Scholar ]
- 125. Warner ET, Colditz GA, Palmer JR, Partridge AH, Rosner BA, Tamimi RM. Reproductive factors and risk of premenopausal breast cancer by age at diagnosis: are there differences before and after age 40? Breast Cancer Res Treat. 2013;142:165–75. doi: 10.1007/s10549-013-2721-9. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 126. White E, Malone KE, Weiss NS, Daling JR. Breast cancer among young U.S. women in relation to oral contraceptive use. J Natl Cancer Inst. 1994;86:505–14. doi: 10.1093/jnci/86.7.505. [ DOI ] [ PubMed ] [ Google Scholar ]
- 127. Work ME, John EM, Andrulis IL, Knight JA, Liao Y, Mulligan AM, et al. Reproductive risk factors and oestrogen/progesterone receptor-negative breast cancer in the Breast Cancer Family Registry. Br J Cancer. 2014;110:1367–77. doi: 10.1038/bjc.2013.807. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 128. Wu AH, Ziegler RG, Pike MC, Nomura AM, West DW, Kolonel LN, et al. Menstrual and reproductive factors and risk of breast cancer in Asian-Americans. Br J Cancer. 1996;73:680–6. doi: 10.1038/bjc.1996.118. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 129. Xing P, Li J, Jin F. A case-control study of reproductive factors associated with subtypes of breast cancer in Northeast China. Med Oncol. 2010;27:926–31. doi: 10.1007/s12032-009-9308-7. [ DOI ] [ PubMed ] [ Google Scholar ]
- 130. Yang CP, Weiss NS, Band PR, Gallagher RP, White E, Daling JR. History of lactation and breast cancer risk. Am J Epidemiol. 1993;138:1050–6. doi: 10.1093/oxfordjournals.aje.a116823. [ DOI ] [ PubMed ] [ Google Scholar ]
- 131. Yavari P, Mosavizadeh M, Sadrol-Hefazi B, Mehrabi Y. Reproductive characteristics and the risk of breast cancer–a case-control study in Iran. Asian Pac J Cancer Prev. 2005;6:370–5. [ PubMed ] [ Google Scholar ]
- 132. Yoo KY, Tajima K, Kuroishi T, Hirose K, Yoshida M, Miura S, et al. Independent protective effect of lactation against breast cancer: a case-control study in Japan. Am J Epidemiol. 1992;135:726–33. doi: 10.1093/oxfordjournals.aje.a116359. [ DOI ] [ PubMed ] [ Google Scholar ]
- 133. Yuan JM, Yu MC, Ross RK, Gao YT, Henderson BE. Risk factors for breast cancer in Chinese women in Shanghai. Cancer Res. 1988;48:1949–53. [ PubMed ] [ Google Scholar ]
- 134. Zheng T, Duan L, Liu Y, Zhang B, Wang Y, Chen Y, et al. Lactation reduces breast cancer risk in Shandong Province, China. Am J Epidemiol. 2000;152:1129–35. doi: 10.1093/aje/152.12.1129. [ DOI ] [ PubMed ] [ Google Scholar ]
- 135. Zheng T, Holford TR, Mayne ST, Owens PH, Zhang Y, Zhang B, et al. Lactation and breast cancer risk: a case-control study in Connecticut. Br J Cancer. 2001;84:1472–6. doi: 10.1054/bjoc.2001.1793. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 136. The Cancer and Steroid Hormone Study of the Centers for Disease Control and the National Institute of Child Health and Human Development. The reduction in risk of ovarian cancer associated with oral-contraceptive use. N Engl J Med. 1987;316:650–5. doi: 10.1056/NEJM198703123161102. [ DOI ] [ PubMed ] [ Google Scholar ]
- 137. Antoniou AC, Rookus M, Andrieu N, Brohet R, Chang-Claude J, Peock S, et al. Reproductive and hormonal factors, and ovarian cancer risk for BRCA1 and BRCA2 mutation carriers: results from the International BRCA1/2 Carrier Cohort Study. Cancer Epidemiol Biomarkers Prev. 2009;18:601–10. doi: 10.1158/1055-9965.EPI-08-0546. [ DOI ] [ PubMed ] [ Google Scholar ]
- 138. Booth M, Beral V, Smith P. Risk factors for ovarian cancer: a case-control study. Br J Cancer. 1989;60:592–8. doi: 10.1038/bjc.1989.320. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 139. Chen Y, Wu PC, Lang JH, Ge WJ, Hartge P, Brinton LA. Risk factors for epithelial ovarian cancer in Beijing, China. Int J Epidemiol. 1992;21:23–9. doi: 10.1093/ije/21.1.23. [ DOI ] [ PubMed ] [ Google Scholar ]
- 140. Chiaffarino F, Pelucchi C, Negri E, Parazzini F, Franceschi S, Talamini R, et al. Breastfeeding and the risk of epithelial ovarian cancer in an Italian population. Gynecol Oncol. 2005;98:304–8. doi: 10.1016/j.ygyno.2005.05.006. [ DOI ] [ PubMed ] [ Google Scholar ]
- 141. Cramer DW, Hutchison GB, Welch WR, Scully RE, Ryan KJ. Determinants of ovarian cancer risk. I. Reproductive experiences and family history. J Natl Cancer Inst. 1983;71:711–6. [ PubMed ] [ Google Scholar ]
- 142. Danforth KN, Tworoger SS, Hecht JL, Rosner BA, Colditz GA, Hankinson SE. Breastfeeding and risk of ovarian cancer in two prospective cohorts. Cancer Causes Control. 2007;18:517–23. doi: 10.1007/s10552-007-0130-2. [ DOI ] [ PubMed ] [ Google Scholar ]
- 143. Greggi S, Parazzini F, Paratore MP, Chatenoud L, Legge F, Mancuso S, et al. Risk factors for ovarian cancer in central Italy. Gynecol Oncol. 2000;79:50–4. doi: 10.1006/gyno.2000.5909. [ DOI ] [ PubMed ] [ Google Scholar ]
- 144. Gwinn ML, Lee NC, Rhodes PH, Layde PM, Rubin GL. Pregnancy, breast feeding, and oral contraceptives and the risk of epithelial ovarian cancer. J Clin Epidemiol. 1990;43:559–68. doi: 10.1016/0895-4356(90)90160-q. [ DOI ] [ PubMed ] [ Google Scholar ]
- 145. Harlow BL, Weiss NS, Roth GJ, Chu J, Daling JR. Case-control study of borderline ovarian tumors: reproductive history and exposure to exogenous female hormones. Cancer Res. 1988;48:5849–52. [ PubMed ] [ Google Scholar ]
- 146. Hartge P, Schiffman MH, Hoover R, McGowan L, Lesher L, Norris HJ. A case-control study of epithelial ovarian cancer. Am J Obstet Gynecol. 1989;161:10–6. doi: 10.1016/0002-9378(89)90221-4. [ DOI ] [ PubMed ] [ Google Scholar ]
- 147. Huusom LD, Frederiksen K, Hogdall EV, Glud E, Christensen L, Hogdall CK, et al. Association of reproductive factors, oral contraceptive use and selected lifestyle factors with the risk of ovarian borderline tumors: a Danish case-control study. Cancer Causes Control. 2006;17:821–9. doi: 10.1007/s10552-006-0022-x. [ DOI ] [ PubMed ] [ Google Scholar ]
- 148. Jordan SJ, Cushing-Haugen KL, Wicklund KG, Doherty JA, Rossing MA. Breast-feeding and risk of epithelial ovarian cancer. Cancer Causes Control. 2012;23:919–27. doi: 10.1007/s10552-012-9963-4. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 149. Jordan SJ, Green AC, Whiteman DC, Webb PM. Risk factors for benign, borderline and invasive mucinous ovarian tumors: epidemiological evidence of a neoplastic continuum? Gynecol Oncol. 2007;107:223–30. doi: 10.1016/j.ygyno.2007.06.006. [ DOI ] [ PubMed ] [ Google Scholar ]
- 150. Kurta ML, Moysich KB, Weissfeld JL, Youk AO, Bunker CH, Edwards RP, et al. Use of fertility drugs and risk of ovarian cancer: results from a U.S.-based case-control study. Cancer Epidemiol Biomarkers Prev. 2012;21:1282–92. doi: 10.1158/1055-9965.EPI-12-0426. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 151. Le DC, Kubo T, Fujino Y, Sokal DC, Vach TH, Pham TM, et al. Reproductive factors in relation to ovarian cancer: a case-control study in Northern Vietnam. Contraception. 2012;86:494–9. doi: 10.1016/j.contraception.2012.02.019. [ DOI ] [ PubMed ] [ Google Scholar ]
- 152. McLaughlin JR, Risch HA, Lubinski J, Moller P, Ghadirian P, Lynch H, et al. Reproductive risk factors for ovarian cancer in carriers of BRCA1 or BRCA2 mutations: a case-control study. Lancet Oncol. 2007;8:26–34. doi: 10.1016/S1470-2045(06)70983-4. [ DOI ] [ PubMed ] [ Google Scholar ]
- 153. Mills PK, Riordan DG, Cress RD. Epithelial ovarian cancer risk by invasiveness and cell type in the Central Valley of California. Gynecol Oncol. 2004;95:215–25. doi: 10.1016/j.ygyno.2004.07.012. [ DOI ] [ PubMed ] [ Google Scholar ]
- 154. Mink PJ, Folsom AR, Sellers TA, Kushi LH. Physical activity, waist-to-hip ratio, and other risk factors for ovarian cancer: a follow-up study of older women. Epidemiology. 1996;7:38–45. doi: 10.1097/00001648-199601000-00008. [ DOI ] [ PubMed ] [ Google Scholar ]
- 155. Moorman PG, Calingaert B, Palmieri RT, Iversen ES, Bentley RC, Halabi S, et al. Hormonal risk factors for ovarian cancer in premenopausal and postmenopausal women. Am J Epidemiol. 2008;167dan:1059–69. doi: 10.1093/aje/kwn006. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 156. Mori M, Harabuchi I, Miyake H, Casagrande JT, Henderson BE, Ross RK. Reproductive, genetic, and dietary risk factors for ovarian cancer. Am J Epidemiol. 1988;128:771–7. doi: 10.1093/oxfordjournals.aje.a115030. [ DOI ] [ PubMed ] [ Google Scholar ]
- 157. Mori M, Nishida T, Sugiyama T, Komai K, Yakushiji M, Fukuda K, et al. Anthropometric and other risk factors for ovarian cancer in a case-control study. Jpn J Cancer Res. 1998;89:246–53. doi: 10.1111/j.1349-7006.1998.tb00555.x. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 158. Ness RB, Grisso JA, Klapper J, Schlesselman JJ, Silberzweig S, Vergona R, et al. Risk of ovarian cancer in relation to estrogen and progestin dose and use characteristics of oral contraceptives. SHARE Study Group. Steroid Hormones and Reproductions. Am J Epidemiol. 2000;152:233–41. doi: 10.1093/aje/152.3.233. [ DOI ] [ PubMed ] [ Google Scholar ]
- 159. Permuth-Wey J, Chen YA, Tsai YY, Chen Z, Qu X, Lancaster JM, et al. Inherited variants in mitochondrial biogenesis genes may influence epithelial ovarian cancer risk. Cancer Epidemiol Biomarkers Prev. 2011;20:1131–45. doi: 10.1158/1055-9965.EPI-10-1224. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 160. Pieta B, Chmaj-Wierzchowska K, Opala T. Past obstetric history and risk of ovarian cancer. Ann Agric Environ Med. 2012;19:385–8. [ PubMed ] [ Google Scholar ]
- 161. Riman T, Dickman PW, Nilsson S, Correia N, Nordlinder H, Magnusson CM, et al. Risk factors for epithelial borderline ovarian tumors: results of a Swedish case-control study. Gynecol Oncol. 2001;83:575–85. doi: 10.1006/gyno.2001.6451. [ DOI ] [ PubMed ] [ Google Scholar ]
- 162. Rosenblatt KA, Thomas DB. Lactation and the risk of epithelial ovarian cancer. The WHO Collaborative Study of Neoplasia and Steroid Contraceptives. Int J Epidemiol. 1993;22:192–7. doi: 10.1093/ije/22.2.192. [ DOI ] [ PubMed ] [ Google Scholar ]
- 163. Rossing MA, Tang MT, Flagg EW, Weiss LK, Wicklund KG. A case-control study of ovarian cancer in relation to infertility and the use of ovulation-inducing drugs. Am J Epidemiol. 2004;160:1070–8. doi: 10.1093/aje/kwh315. [ DOI ] [ PubMed ] [ Google Scholar ]
- 164. Salazar-Martinez E, Lazcano-Ponce EC, Gonzalez Lira-Lira G, Escudero-De los Rios P, Salmeron-Castro J, Hernandez-Avila M. Reproductive factors of ovarian and endometrial cancer risk in a high fertility population in Mexico. Cancer Res. 1999;59:3658–62. [ PubMed ] [ Google Scholar ]
- 165. Siskind V, Green A, Bain C, Purdie D. Breastfeeding, menopause, and epithelial ovarian cancer. Epidemiology. 1997;8:188–91. doi: 10.1097/00001648-199703000-00011. [ DOI ] [ PubMed ] [ Google Scholar ]
- 166. Titus-Ernstoff L, Rees JR, Terry KL, Cramer DW. Breast-feeding the last born child and risk of ovarian cancer. Cancer Causes Control. 2010;21:201–7. doi: 10.1007/s10552-009-9450-8. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 167. Tsilidis KK, Allen NE, Key TJ, Dossus L, Lukanova A, Bakken K, et al. Oral contraceptive use and reproductive factors and risk of ovarian cancer in the European Prospective Investigation into Cancer and Nutrition. Br J Cancer. 2011;105:1436–42. doi: 10.1038/bjc.2011.371. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 168. Tung KH, Goodman MT, Wu AH, McDuffie K, Wilkens LR, Kolonel LN, et al. Reproductive factors and epithelial ovarian cancer risk by histologic type: a multiethnic case-control study. Am J Epidemiol. 2003;158:629–38. doi: 10.1093/aje/kwg177. [ DOI ] [ PubMed ] [ Google Scholar ]
- 169. Weiderpass E, Sandin S, Inoue M, Shimazu T, Iwasaki M, Sasazuki S, et al. Risk factors for epithelial ovarian cancer in Japan – results from the Japan Public Health Center-based Prospective Study cohort. Int J Oncol. 2012;40:21–30. doi: 10.3892/ijo.2011.1194. [ DOI ] [ PubMed ] [ Google Scholar ]
- 170. Whittemore AS, Harris R, Itnyre J. Characteristics relating to ovarian cancer risk: collaborative analysis of 12 US case-control studies. II. Invasive epithelial ovarian cancers in white women. Collaborative Ovarian Cancer Group. Am J Epidemiol. 1992;136:1184–203. doi: 10.1093/oxfordjournals.aje.a116427. [ DOI ] [ PubMed ] [ Google Scholar ]
- 171. Wilailak S, Vipupinyo C, Suraseranivong V, Chotivanich K, Kietpeerakool C, Tanapat Y, et al. Depot medroxyprogesterone acetate and epithelial ovarian cancer: a multicentre case-control study. BJOG. 2012;119:672–7. doi: 10.1111/j.1471-0528.2012.03298.x. [ DOI ] [ PubMed ] [ Google Scholar ]
- 172. Yen ML, Yen BL, Bai CH, Lin RS. Risk factors for ovarian cancer in Taiwan: a case-control study in a low-incidence population. Gynecol Oncol. 2003;89:318–24. doi: 10.1016/s0090-8258(03)00088-x. [ DOI ] [ PubMed ] [ Google Scholar ]
- 173. Zhang M, Xie X, Lee AH, Binns CW. Prolonged lactation reduces ovarian cancer risk in Chinese women. Eur J Cancer Prev. 2004;13:499–502. doi: 10.1097/00008469-200412000-00006. [ DOI ] [ PubMed ] [ Google Scholar ]
- 174. Chowdhury S, Sarkar NR, Roy SK. Impact of lactational performance on bone mineral density in marginally-nourished Bangladeshi women. J Health Popul Nutr. 2002;20:26–30. [ PubMed ] [ Google Scholar ]
- 175. Drinkwater BL, Chesnut CH., 3rd Bone density changes during pregnancy and lactation in active women: a longitudinal study. Bone Miner. 1991;14:153–60. doi: 10.1016/0169-6009(91)90092-e. [ DOI ] [ PubMed ] [ Google Scholar ]
- 176. Hawker GA, Forsmo S, Cadarette SM, Schei B, Jaglal SB, Forsen L, et al. Correlates of forearm bone mineral density in young Norwegian women: the Nord-Trondelag Health Study. Am J Epidemiol. 2002;156:418–27. doi: 10.1093/aje/kwf061. [ DOI ] [ PubMed ] [ Google Scholar ]
- 177. Henderson PH, 3rd, Sowers M, Kutzko KE, Jannausch ML. Bone mineral density in grand multiparous women with extended lactation. Am J Obstet Gynecol. 2000;182:1371–7. doi: 10.1067/mob.2000.107468. [ DOI ] [ PubMed ] [ Google Scholar ]
- 178. Lenora J, Lekamwasam S, Karlsson MK. Effects of multiparity and prolonged breast-feeding on maternal bone mineral density: a community-based cross-sectional study. BMC Womens Health. 2009;9:19. doi: 10.1186/1472-6874-9-19. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 179. Wiklund PK, Xu L, Wang Q, Mikkola T, Lyytikainen A, Volgyi E, et al. Lactation is associated with greater maternal bone size and bone strength later in life. Osteoporos Int. 2012;23:1939–45. doi: 10.1007/s00198-011-1790-z. [ DOI ] [ PubMed ] [ Google Scholar ]
- 180. Benitez I, de la Cruz J, Suplido A, Oblepias V, Kennedy K, Visness C. Extending lactational amenorrhoea in Manila: a successful breast-feeding education programme. J Biosoc Sci. 1992;24:211–31. doi: 10.1017/s002193200001974x. [ DOI ] [ PubMed ] [ Google Scholar ]
- 181. Dada OA, Akesode FA, Olanrewaju DM, Olowu OA, Sule-Odu O, Fakoya TA, et al. Infant feeding and lactational amenorrhea in Sagamu, Nigeria. Afr J Reprod Health. 2002;6:39–50. [ PubMed ] [ Google Scholar ]
- 182. Davies-Adetugbo AA, Ojofeitimi EO. Maternal education, breastfeeding behaviours and lactational amenorrhoea: studies among two ethnic communities in Ile Ife, Nigeria. Nutr Health. 1996;11:115–26. doi: 10.1177/026010609601100204. [ DOI ] [ PubMed ] [ Google Scholar ]
- 183. Dewey KG, Cohen RJ, Rivera LL, Canahuati J, Brown KH. Effects of age at introduction of complementary foods to breast-fed infants on duration of lactational amenorrhea in Honduran women. Am J Clin Nutr. 1997;65:1403–9. doi: 10.1093/ajcn/65.5.1403. [ DOI ] [ PubMed ] [ Google Scholar ]
- 184. Egbuonu I, Ezechukwu CC, Chukwuka JO, Ikechebelu JI. Breast-feeding, return of menses, sexual activity and contraceptive practices among mothers in the first six months of lactation in Onitsha, South Eastern Nigeria. J Obstet Gynaecol. 2005;25:500–3. doi: 10.1080/01443610500171250. [ DOI ] [ PubMed ] [ Google Scholar ]
- 185. Ingram J, Hunt L, Woolridge M, Greenwood R. The association of progesterone, infant formula use and pacifier use with the return of menstruation in breastfeeding women: a prospective cohort study. Eur J Obstet Gynecol Reprod Biol. 2004;114:197–202. doi: 10.1016/j.ejogrb.2003.12.003. [ DOI ] [ PubMed ] [ Google Scholar ]
- 186. Kumar S, Reddaiah VP. Lactational amenorrhea in urban poor women and its implications for use of contraception. Indian Pediatr. 1988;25:987–92. [ PubMed ] [ Google Scholar ]
- 187. Lewis PR, Brown JB, Renfree MB, Short RV. The resumption of ovulation and menstruation in a well-nourished population of women breastfeeding for an extended period of time. Fertil Steril. 1991;55:529–36. [ PubMed ] [ Google Scholar ]
- 188. Radwan H, Mussaiger AO, Hachem F. Breast-feeding and lactational amenorrhea in the United Arab Emirates. J Pediatr Nurs. 2009;24:62–8. doi: 10.1016/j.pedn.2007.09.005. [ DOI ] [ PubMed ] [ Google Scholar ]
- 189. Ravera M, Ravera C, Reggiori A, Cocozza E, Cianta F, Riccioni G, et al. A study of breastfeeding and the return of menses in Hoima District, Uganda. East Afr Med J. 1995;72:147–9. [ PubMed ] [ Google Scholar ]
- 190. WHO. The World Health Organization Multinational Study of Breast-feeding and Lactational Amenorrhea. I. Description of infant feeding patterns and of the return of menses. World Health Organization Task Force on Methods for the Natural Regulation of Fertility. Fertil Steril. 1998;70:448–60. doi: 10.1016/s0015-0282(98)00190-3. [ DOI ] [ PubMed ] [ Google Scholar ]
- 191. Sarkar NR, Taylor R. Weight loss during prolonged lactation in rural Bangladeshi mothers. J Health Popul Nutr. 2005;23:177–83. [ PubMed ] [ Google Scholar ]
- 192. Stuebe AM, Kleinman K, Gillman MW, Rifas-Shiman SL, Gunderson EP, Rich-Edwards J. Duration of lactation and maternal metabolism at 3 years postpartum. J Womens Health (Larchmt) 2010;19:941–50. doi: 10.1089/jwh.2009.1660. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 193. Onyango AW, Nommsen-Rivers L, Siyam A, Borghi E, de Onis M, Garza C, et al. Post-partum weight change patterns in the WHO Multicentre Growth Reference Study. Matern Child Nutr. 2011;7:228–40. doi: 10.1111/j.1740-8709.2010.00295.x. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 194. Monteiro da Silva Mda C, Marlucia Oliveira A, Pereira Magalhaes de Oliveira L, Silva dos Santos Fonseca DN, Portela de Santana ML, de Araujo Goes Neto E, et al. Determinants of postpartum weight variation in a cohort of adult women; a hierarchical approach. Nutr Hosp. 2013;28:660–70. doi: 10.3305/nh.2013.28.3.6391. [ DOI ] [ PubMed ] [ Google Scholar ]
- 195. Samano R, Martinez-Rojano H, Godinez Martinez E, Sanchez Jimenez B, Villeda Rodriguez GP, Perez Zamora J, et al. Effects of breastfeeding on weight loss and recovery of pregestational weight in adolescent and adult mothers. Food Nutr Bull. 2013;34:123–30. doi: 10.1177/156482651303400201. [ DOI ] [ PubMed ] [ Google Scholar ]
- 196. Sakai T. Does breastfeeding reduce risk for breast cancer? A short lesson in evidence-based practice MCN. Am J Matern Child Nurs. 2001;26:42–5. doi: 10.1097/00005721-200101000-00011. [ DOI ] [ PubMed ] [ Google Scholar ]
- 197. Velie EM, Nechuta S, Osuch JR. Lifetime reproductive and anthropometric risk factors for breast cancer in postmenopausal women. Breast Dis. 2005;24:17–35. doi: 10.3233/bd-2006-24103. [ DOI ] [ PubMed ] [ Google Scholar ]
- 198. Althuis MD, Fergenbaum JH, Garcia-Closas M, Brinton LA, Madigan MP, Sherman ME. Etiology of hormone receptor-defined breast cancer: a systematic review of the literature. Cancer Epidemiol Biomarkers Prev. 2004;13:1558–68. [ PubMed ] [ Google Scholar ]
- 199. Ma H, Bernstein L, Pike MC, Ursin G. Reproductive factors and breast cancer risk according to joint estrogen and progesterone receptor status: a meta-analysis of epidemiological studies. Breast Cancer Res. 2006;8:R43. doi: 10.1186/bcr1525. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 200. Newcomb PA. Lactation and breast cancer risk. J Mammary Gland Biol Neoplasia. 1997;2:311–8. doi: 10.1023/a:1026344707161. [ DOI ] [ PubMed ] [ Google Scholar ]
- 201. Collaborative Group on Hormonal Factors in Breast Cancer. Breast cancer and breastfeeding: collaborative reanalysis of individual data from 47 epidemiological studies in 30 countries, including 50302 women with breast cancer and 96973 women without the disease. Lancet. 2002;360:187–95. doi: 10.1016/S0140-6736(02)09454-0. [ DOI ] [ PubMed ] [ Google Scholar ]
- 202. Henderson BE, Feigelson HS. Hormonal carcinogenesis. Carcinogenesis. 2000;21:427–33. doi: 10.1093/carcin/21.3.427. [ DOI ] [ PubMed ] [ Google Scholar ]
- 203. Smalley M, Ashworth A. Stem cells and breast cancer: a field in transit. Nat Rev Cancer. 2003;3:832–44. doi: 10.1038/nrc1212. [ DOI ] [ PubMed ] [ Google Scholar ]
- 204. Jacob S, Spencer NA, Bullivant SB, Sellergren SA, Mennella JA, McClintock MK. Effects of breastfeeding chemosignals on the human menstrual cycle. Hum Reprod. 2004;19:422–9. doi: 10.1093/humrep/deh057. [ DOI ] [ PubMed ] [ Google Scholar ]
- 205. McNeilly AS. Lactational control of reproduction. Reprod Fertil Dev. 2001;13:583–90. doi: 10.1071/rd01056. [ DOI ] [ PubMed ] [ Google Scholar ]
- 206. Miller SC, Bowman BM. Rapid improvements in cortical bone dynamics and structure after lactation in established breeder rats. Anat Rec A Discov Mol Cell Evol Biol. 2004;276:143–9. doi: 10.1002/ar.a.10138. [ DOI ] [ PubMed ] [ Google Scholar ]
- 207. Vekemans M. Postpartum contraception: the lactational amenorrhea method. Eur J Contracept Reprod Health Care. 1997;2:105–11. doi: 10.3109/13625189709167463. [ DOI ] [ PubMed ] [ Google Scholar ]
- 208. Boardley DJ, Sargent RG, Coker AL, Hussey JR, Sharpe PA. The relationship between diet, activity, and other factors, and postpartum weight change by race. Obstet Gynecol. 1995;86:834–8. doi: 10.1016/0029-7844(95)00283-W. [ DOI ] [ PubMed ] [ Google Scholar ]
- 209. Gunderson EP, Abrams B, Selvin S. The relative importance of gestational gain and maternal characteristics associated with the risk of becoming overweight after pregnancy. Int J Obes Relat Metab Disord. 2000;24:1660–8. doi: 10.1038/sj.ijo.0801456. [ DOI ] [ PubMed ] [ Google Scholar ]
- 210. WHO. Indicators for assessing breastfeeding practices. Geneva: World Health Organization; 1991. [ Google Scholar ]
- 211. Kabat GC, Kim MY, Woods NF, Habel LA, Messina CR, Wactawski-Wende J, et al. Reproductive and menstrual factors and risk of ductal carcinoma in situ of the breast in a cohort of postmenopausal women. Cancer Causes Control. 2011;22:1415–24. doi: 10.1007/s10552-011-9814-8. [ DOI ] [ PubMed ] [ Google Scholar ]
- 212. Saeki T, Sano M, Komoike Y, Sonoo H, Honjyo H, Ochiai K, et al. No increase of breast cancer incidence in Japanese women who received hormone replacement therapy: overview of a case-control study of breast cancer risk in Japan. Int J Clin Oncol. 2008;13:8–11. doi: 10.1007/s10147-007-0728-0. [ DOI ] [ PubMed ] [ Google Scholar ]
- View on publisher site
- PDF (379.7 KB)
- Collections

Similar articles
Cited by other articles, links to ncbi databases.
- Download .nbib .nbib
- Format: AMA APA MLA NLM
Add to Collections
Breastfeeding initiation and support: A literature review of what women value and the impact of early discharge
Affiliations.
- 1 School of Nursing and Midwifery, Flinders University, Australia.
- 2 School of Nursing and Midwifery, Flinders University, Australia. Electronic address: [email protected].
- PMID: 27773608
- DOI: 10.1016/j.wombi.2016.09.013
Problem: Early discharge following birth has become an emerging phenomenon in many countries. It is likely early discharge has an impact on the establishment of breastfeeding.
Objective: To critically appraise the evidence on what women value in relation to breastfeeding initiation and support, and investigate the impact early discharge can have on these values.
Method: A literature search was conducted for publications since 2005 using the following databases: Cumulative Index of Nursing and Allied Health Literature (CINAHL), Medline, Scopus and PsycINFO; 21 primary articles were selected and included in the review.
Findings: There is no standard definition for 'early discharge' worldwide. Due to inconsistent definitions worldwide and minimal literature using a 24h definition, research defining early discharge as up to 72h postpartum is included. Seven key factors in relation to breastfeeding initiation and support following early discharge were identified, namely trust and security, consistent advice, practical breastfeeding support, breastfeeding education, comfortable environment, positive attitudes and emotional support, and individualised care.
Conclusion: The findings suggest individualised postnatal lengths of stay may be beneficial for the initiation of breastfeeding. Five values were not impacted by early discharge, but rather individual midwives' practice. There is consensus in the literature that early discharge promoted a comfortable environment to support breastfeeding initiation. Wide variations in the definition of early postnatal discharge made it difficult to draw influential conclusions. Therefore, further research is required.
Keywords: Breastfeeding; Early discharge; Initiation or establish; Length of stay; Postnatal care.
Copyright © 2016 Australian College of Midwives. Published by Elsevier Ltd. All rights reserved.
Publication types
- Breast Feeding / psychology*
- Infant, Newborn
- Length of Stay
- Mothers / psychology*
- Patient Discharge
- Postnatal Care / psychology*
- Postpartum Period / psychology*
- Open access
- Published: 18 June 2016
Early initiation of breastfeeding: a systematic literature review of factors and barriers in South Asia
- Indu K. Sharma 1 &
- Abbey Byrne 1
International Breastfeeding Journal volume 11 , Article number: 17 ( 2016 ) Cite this article
30k Accesses
118 Citations
6 Altmetric
Metrics details
Early or timely initiation of breastfeeding is crucial in preventing newborn deaths and influences childhood nutrition however remains low in South Asia and the factors and barriers warrant greater consideration for improved action. This review synthesises the evidence on factors and barriers to initiation of breastfeeding within 1 h of birth in South Asia encompassing Afghanistan, Bangladesh, Bhutan, India, Maldives, Nepal, Pakistan and Sri Lanka.
Studies published between 1990 and 2013 were systematically reviewed through identification in Academic Search Complete, CINAHL, Global Health, MEDLINE and Scopus databases. Twenty-five studies meeting inclusion criteria were included for review. Structured thematic analysis based on leading frameworks was undertaken to understand factors and barriers.
Factors at geographical, socioeconomic, individual, and health-specific levels, such as residence, education, occupation, income, mother’s age and newborn’s gender, and ill health of mother and newborn at delivery, affect early or timely breastfeeding initiation in South Asia. Reported barriers impact through influence on acceptability by traditional feeding practices, priests’ advice, prelacteal feeding and discarding colostrum, mother-in-law’s opinion; availability and accessibility through lack of information, low access to media and health services, and misperception, support and milk insufficiency, involvement of mothers in decision making.
Conclusions
Whilst some barriers manifest similarly across the region some factors are context-specific thus tailored interventions are imperative. Initiatives halting factors and directed towards contextual barriers are required for greater impact on newborn survival and improved nutrition in the South Asia region.
Child survival is an ongoing public health priority in the South Asia region, which includes eight countries - Afghanistan, Bangladesh, Bhutan, India, Maldives, Nepal, Pakistan and Sri-Lanka [ 1 ]. Countries within the region have made significant progress towards Millennium Development Goal 4 (MDG 4) to reduce the under-five mortality rate (U5MR) by two-thirds by 2015 [ 2 ]. However the regional U5MR remains off target at 58 deaths per 1000 live births compared to the target of 42 deaths per 1000 live births [ 3 ]. Progress has largely been for children aged 1–59 months and now the critical priority is mortality among newborns (birth to 28 days). In the South Asia region, the neonatal mortality rate (NMR) now accounts for 53 % of the U5MR, in contrast to 34 % in Sub-Sahara Africa, and comprises 40 % of all newborn deaths in developing regions of the world [ 3 ]. The burden is unequal within the region: the NMR (expressed as deaths per 1000 live births) in 2012 was estimated to be as high as 42 in Pakistan yet as low as six in Sri-Lanka and the Maldives [ 3 ]. Improving newborn survival is critical for further reductions in U5MR and achievement of MDG 4, particularly in the South Asia region.
Early or timely initiation of breastfeeding, specifically within 1 h of birth, refers to the best practice recommendation by the World Health Organization (WHO) [ 4 ]. A recent systematic review and meta-analysis revealed that breastfeeding initiation after the first hour of birth doubles the risk of neonatal mortality [ 5 ]. In specific countries, initiating within 1 h reduced deaths by 19 % in Nepal [ 6 ] and 22 % in Ghana [ 7 ]. The evidence, drawn from meta-analysis and over 63 developing countries, shows that early initiation of breastfeeding prevents newborn infections, averts newborn death due to sepsis, pneumonia, diarrhoea and hypothermia, and facilitates sustained breastfeeding [ 8 ]. In South Asia, merely 41 % of newborns are breastfed within 1 h of birth [ 1 ]. Several South Asian countries have some of the worst early initiation of breastfeeding practices in the world; the rates in Pakistan, India, Bangladesh and Nepal are only 29, 41, 47 and 45 % respectively [ 1 ].
Insufficient attention is afforded to the public health issue of early or timely initiation of breastfeeding, and the causes of poor practice, even though this preventive intervention is highly cost-effective [ 6 , 7 , 9 ]. Breastfeeding research predominantly focuses on exclusive breastfeeding to the age of 6 months and other infant and young child feeding (IYCF) indicators [ 7 , 10 , 11 ]. Existing systematic literature reviews on early initiation primarily draw on evidence from developed countries and on the effect of skin-to-skin contact on breastfeeding rates [ 12 – 15 ]. It is important to understand the factors associated with delayed breastfeeding initiation and the existing barriers and facilitators to early initiation in order to design and deliver effective strategies to improve the practice [ 7 ] and accelerate progress in newborn survival.
This systematic literature review synthesises published evidence on the factors and barriers associated with the initiation of breastfeeding within 1 h of birth in South Asian countries to inform a future of relevant, context-specific actions.
Protocol of the systematic literature review was proposed in the University of Melbourne Master of Public Health research project and was approved by the University prior to commencement. The search was undertaken from July to September, 2013. The methods and reporting were developed and conducted with systematic methodology and consistent with the PRISMA reporting guidelines [ 16 ].
Source of literature
This drew on published literature in the electronic bibliographic databases of: Academic Search Complete, Cumulative Index to Nursing and Allied Health (CINAHL), Global Health, MEDLINE Web of Knowledge and Scopus and supplemented by scanning the reference lists of papers included for review.
Search terms
Search terms were applied with various Boolean operators for three core concepts: breastfeeding; timing of breastfeeding initiation; and countries in South Asia.
The various search terms are:
Breastfeed* or “Breast feed*” or Breastfed* or Breast-fed or “Breast fed*” Breast-feed* or “breast milk” or “breastmilk” or “breast-milk”
Initiat* or colostrum or “pre-lacteal” or “pre lacteal” or prelacteal or “early” or delay South Asia*" or “South East Asia*” or “Southern Asia*” or “South Eastern Asia*” or “Southern East Asia*” or SEAR or Afghan* or Bangladesh* or Bhutan* or India* or Maldives or Nepal* or Pakistan* or “Sri Lanka*”.
MeSH heading was used for breastfeeding; and ASIA South-eastern or Asia. A detailed search strategy of one database is presented in Additional file 1 .
Inclusion and exclusion criteria
The eligibility of studies for review was assessed on a set of four inclusion and exclusion criteria, based on the reporting of factors and/or barriers, timing of breastfeeding initiation, country, year, language, study design and full text availability. The set of criteria are shown in Table 1 . Identification of barriers was based on ‘ issues that drive the reasons why people do not have or make use of services’ , as the widely applied definition in literature and by Jacobs et al. (2011) [ 17 ] in the analytical framework for analysis of health service barriers.
Study selection and data extraction
Studies retrieved from databases were exported to Endnote X5 and duplicated citations were removed. Abstracts were screened for relevance to the study question and country of the study. All other inclusion and exclusion criteria were applied through assessment of the full text publications.
Studies selected for inclusion were transferred to a Microsoft Excel spreadsheet for extraction of data items of: setting, population, methods, factors and reported barriers to early initiation of breastfeeding, and for thematic analysis.
Quality appraisal
Quality of included studies was appraised separately for qualitative and quantitative methods assessing features of study design, methodology and analysis. Studies were classified into strong, moderate and weak based on criteria set within two different tools: Critical Appraisal Skills Programme (CASP) and Effective Public Health Practice Project (EPHPP) tools. Qualitative studies were appraised using the CASP tool which contains a checklist of ten screening questions regarding the aim of the research, appropriateness of the qualitative methodology, appropriateness of research design to address aim, appropriateness of recruitment strategy, data collection methods, relationship between researcher and participants, ethical issues, data analysis, statement of findings and value of research [ 18 ]. This tool has previously been evaluated, revised and reviewed [ 19 ]. Quantitative studies were appraised using the EPHPP tool to rate studies based on given criteria on the basis of: selection bias, study design, confounders, blinding, data collection methods, withdrawals and drop-outs, intervention integrity (for intervention studies) and analyses [ 20 , 21 ]. This tool has demonstrated high inter-reliability across individual domains and high intra-class correlation coefficient value [ 20 ]. For mixed-method studies, the CASP tool was applied to the qualitative elements and the EPHPP tool to the quantitative elements.
These quality appraisal methods and associated rankings assess the validity of individual studies. These are not a means to weighting the magnitude of study findings between studies, rather the conclusions of the quality appraisal indicate the rigor of the study and through such the confidence, or weight, with which the study findings can be taken.
Synthesis of results
The results were synthesized according to the two features being addressed; the factors, and the barriers, associated with delayed initiation of breastfeeding. The results concerning factors were synthesized systematically according to the level at which the factors exert influence on early breastfeeding initiation. This approach was based on the framework for analysis of barriers with a health system lens established by The SURE Collaboration for structured and systematic analyses [ 22 ]. The levels relevant to the factors of this health issue were identified to be: geographical, health-specific, socio-economic, and individual. The results on barriers were synthesised using thematic analysis and arranged based on the analytical framework of barriers affecting health care in low-resource Asia settings developed through a review by Jacobs et al. [ 17 ], adapted from Peters et al. [ 23 ] and Ensor and Cooper [ 24 ]. This analytical framework provided a structured and comprehensive perspective on barriers experienced in the health sector, categorised as accessibility, availability and acceptability barriers in terms of both supply and demand [ 17 ].
Study selection
The search strategy retrieved 1723 studies. After applying the process of selection, summarised in Fig. 1 , 25 studies were included for review. Scanning reference lists of reviewed articles did not produce additional results, suggesting that the search was comprehensive.
Flow chart of selection process
Studies selected for review represented Bangladesh (four), India (eight), Maldives (one), Nepal (three), Pakistan (six) and Sri Lanka (two). One study was multi-country across Bangladesh, India, Nepal and Sri Lanka while no studies were retrieved from Afghanistan and Bhutan. Two studies used qualitative methods, 17 used quantitative methods and six were mixed-methods studies.
Participants in the included studies were ever-married women of reproductive age, typically with at least one child; traditional birth attendants (TBAs); mother-in-laws; and fathers. Several studies involve random selection of participants while others targeted new mothers and fathers, untrained TBAs, ethnic minority women, attendees of immunisation clinics, postnatal mothers, mothers who were currently breastfeeding and those who had discontinued breastfeeding.
The summarised characteristics of included studies are presented in Table 2 , with study details in Additional file 2 .
Quality of studies
Based on the CASP criteria, both qualitative studies reviewed were of moderate quality owing to limitations in the research design, recruitment strategy and data analysis. Based on the EPHPP, none of the quantitative studies were high-quality ranking because all were moderately-weighted cross-sectional design. Eight studies were moderate quality, while nine were weak based on design, unreliable data collection method and no controlling for confounding factors. Of the six mixed-method studies, four were weak in quantitative and moderate in qualitative design; one was moderate and one was weak in both qualitative and quantitative design.
Factors associated with early initiation of breastfeeding
The factors associated with timely or early initiation of breastfeeding as revealed by the existing literature, according to the levels for analysis, are: geographical, socioeconomic, individual and health-specific. The results pertaining to factors are detailed below, and presented in summary in Fig. 2 .
Geographical factors
Geographical factors found to have a pattern with early initiation of breastfeeding varied across countries. Delayed initiation rate is higher for those living in North Central Province in Sri Lanka [ 25 ], Central region in India [ 26 ], Sindh province in Pakistan [ 27 ] and lower in the plains (Tarai) region of Nepal [ 28 ]. Although residing in a rural area was associated with delayed initiation in India [ 26 ] and Sri Lanka [ 25 ], residing in urban areas was significantly associated with delayed initiation in Bangladesh [ 29 ]. All five of these studies have moderate quality grading.
Socioeconomic factors
The social and economic circumstances of a woman and the household have much influence on timing of breastfeeding initiation in the South Asian context, pertinently the education of mother, occupation of mother, household wealth and family size and family type. Delayed initiation of breastfeeding is more prevalent among women who have no formal education in Bangladesh [ 29 , 30 ], India [ 26 ], Nepal [ 31 ] and Pakistan [ 32 ]. In Bangladesh, delayed initiation is associated with low schooled husbands [ 29 ]. However, working status of mothers is contrasting depending on the setting. Working mothers in Pakistan are more likely to delay initiation compared to non-working mothers [ 27 ] whilst in India non-working mothers are more likely to delay initiation [ 26 ]. Breastfeeding initiation based on wealth also contrasts between countries. Delayed initiation is more likely by women from poorest households in Bangladesh [ 29 , 30 ] yet by those of the richest households in Sri Lanka [ 25 ]. In an urban area of India, Kolkata, early initiation practices were higher among women from lower-income groups [ 33 ]. In terms of family type and size, women with nuclear families (not residing with the mother-in-law), with fewer children, are more likely to delay initiation in Nepal [ 34 ]. Results relating to socioeconomic influence from studies in India and Bangladesh [ 25 – 27 , 29 , 30 ] are more strongly founded based of moderate quality grading, whilst those of Nepal, Pakistan and Sri Lanka [ 31 – 34 ] were of weak quality grading.
Individual factors
Birth order, previous birth interval, teenage motherhood and having a male child are linked with early initiation of breastfeeding. For their first-born child, women are less likely to initiate breastfeeding within 1 h of birth, as reported in Sri Lanka [ 25 , 35 ], India [ 36 ] and Pakistan (no association in multivariate analysis) [ 27 ]. Additionally, delayed initiation is more likely for children of five or later birth order in Bangladesh [ 29 ]. Similarly, children of teenage mothers (aged 15–19 years) and male child were less likely to be breastfed within 1 h of birth [ 25 ]. Most of the studies reporting the individual factors of timely or early initiation of breastfeeding are with moderate quality except one high quality [ 25 ].
Health related factors
Many reviewed studies specify health and physiological conditions of mother, health and physiological condition of newborn and delivery factors as health related factors associated with either the practice or non-practice of early initiation of breastfeeding.
Five studies reported the mother’s health condition as a reason for delaying breastfeeding [ 37 – 41 ], specifically being unconscious after delivery [ 38 , 41 ], unable to sit, experiencing hypertension [ 37 ], fatigue [ 40 ], or generalised ‘illness’ after delivery [ 39 ].
Of the newborn, early initiation is comparatively lower among children of low birth weight [ 25 ], prematurity [ 36 ], and being ill or considered weak [ 38 , 41 ].
Delivery-related conditions have also been identified as a factor in the practice of early initiation of breastfeeding in South Asia. Seven qualitative studies conducted in Bangladesh [ 41 ], India [ 26 , 36 ], Nepal [ 28 ], Pakistan [ 27 ], Maldives [ 42 ] and Sri Lanka [ 35 ] highlighted delivery by caesarean section as a major factor. Similarly, two other studies specified that time for recovery from caesarean delivery [ 37 ] and delay in uniting the newborn and mother after caesarean section [ 41 ] as reasons for delayed initiation. Moreover, three studies reported specific care practices as factors to early initiation of breastfeeding among facility-based births, namely late delivery of the placenta [ 41 ], allocated time for recovery from delivery [ 37 ], delay in shifting women from the labour room [ 38 ], and delivery during the night [ 37 ].
Barriers to early initiation of breastfeeding
The identified barriers to the early initiation of breastfeeding in South Asia have been synthesised as supply side and demand side barriers in terms of accessibility, availability and acceptability, as presented in Table 3 .
Supply-side barriers
Barriers to availability.
Lack of availability of information for correct knowledge and misperception on breastfeeding was reported as a barrier. Lack of knowledge on the importance of early initiation and the perception that water must be given to the newborn because breast milk alone will not sustain the baby were observed in Bangladesh [ 41 ]. However, for the quantitative data the study based findings only on descriptive values without statistical associations.
Barriers to accessibility
Nine studies, eight of which were moderate quality grading [ 25 , 26 , 28 – 30 , 35 , 41 , 43 ], reported barriers to accessing initiation of breastfeeding in terms of antenatal and postnatal check-up, home delivery, and delivery by non-skilled attendants. No or few antenatal appointments, home delivery, delivery assistance and practices and no post-natal check-up have been reported in literature as supply side barriers to accessibility in terms of facilitation of breastfeeding practice. Six studies consistently reported no or few antenatal appointments as a barrier to early initiation of breastfeeding in Bangladesh [ 29 , 30 ], India [ 26 ], Nepal [ 31 ] and Sri Lanka [ 35 , 43 ]. In terms of delivery, home delivery is linked with delayed initiation, shown in Bangladesh [ 29 ], India [ 26 , 43 ], Sri Lanka [ 25 ] and Nepal [ 31 ]. Similarly, early initiation of breastfeeding is lower for women assisted by TBAs or friends/relatives during delivery in India compared to health professionals [ 26 ]. In contrast, in Nepal women assisted by TBAs are less likely to delay initiation compared to those assisted by health professionals [ 28 ]. In Bangladesh study results are conflicting, with one study reporting early initiation with birth assistance by medically trained providers [ 30 ], yet in a qualitative study mothers described that midwives discourage breastfeeding for first 3 days [ 41 ]. Moreover, women not receiving a postnatal check-up from a public health midwife are more likely to delay breastfeeding initiation compared to those receiving postnatal check-up in Sri Lanka [ 35 ], and India [ 26 ].
Demand-side barriers
Barriers to acceptability.
Four weak [ 36 , 39 , 44 , 45 ] and four moderate quality studies [ 41 , 46 – 48 ] highlight traditional feeding practices as demand side barriers to acceptance of early initiation of breastfeeding in South Asia. Specifically, breastfeeding according to time of birth and advice of priest, use of prelacteal feeds and discarding colostrum, and influence of mother in law are observed. A study conducted in Haryana of India revealed the practice of initiating breastfeeding in the evening after seeing stars if the child was born in morning and if the birth was in the night breastfeeding was started within a few hours or early morning [ 44 ]. In Bangladesh bathing rituals for mother and newborn must take place before initiating breastfeeding [ 41 ]. Moreover, a study conducted in Jammu of Kashmir State revealed advice of priests as a reason for delayed initiation of breastfeeding [ 45 ]. Negative perception of colostrum and the use of prelacteal feeds are common barriers, shown in four studies. In Pakistan women reported discarding colostrum, withholding breastfeeding and replacing with prelacteal feeding which is typically administered via a finger of an elderly person and perceived to clean the stomach and strengthen the newborn [ 46 ]. Another study described the perception that colostrum may harm or even kill the newborn because it is dirty and stored for 9 months in the breast [ 47 ]. Likewise, in a rural area of India mothers perceive that the first milk is harmful to the baby [ 48 ]. Mothers in urban India who accept giving colostrum are more likely to initiate breastfeeding within 1 h of the birth [ 36 ]. Influence of mother in law and/or elder women has also been observed as barrier, with decision-making around maternal and newborn care reportedly as a role of elderly women of family in India [ 39 ], and mother-in-law in India [ 45 ], Bangladesh [ 41 ], and Pakistan [ 46 ].
Lack of available support and milk insufficiency are demand side barriers. A study from Bangladesh reported lack of support as a barrier to early initiation of breastfeeding [ 41 ]. Milk insufficiency is reported by four studies (of weak to moderate quality grading) as the reason for not initiating breastfeeding within 1 h of birth [ 39 , 41 , 48 , 49 ].
Our review highlights two major types of barriers to access to information regarding the initiation of breastfeeding. Firstly, two moderate quality studies reveal lack of access to media, linked with low socio-economic status of a household and area, as reported barriers to early initiation of breastfeeding in South Asia. Women not watching television in Bangladesh [ 29 ] and India [ 26 ], and mothers not listening to radio or not reading the newspaper in India [ 26 ] are independent barriers to early breastfeeding initiation. Despite breastfeeding being of low direct cost and a highly cost-effective strategy [ 6 , 7 , 9 ], lack of access to information is often linked to wealth in access to services, media, and information. Secondly, three other studies with moderate quality grading [ 26 , 28 , 29 ] highlight lack of access of mothers in decision making as a barrier to the early initiation. Lack of mother’s involvement in decision making has been reported as reason for not initiating breastfeeding within 1 h of birth. Mothers are less likely to delay initiation if they have a final say in all categories of decision making in Nepal [ 28 ]. This was also reported in India [ 26 ] and Bangladesh [ 29 ] however was not significant after adjusting for other variables.
Early initiation of breastfeeding, specifically within 1 h of birth, refers to the best practice recommendation by the WHO [ 4 ]. Increasing early initiation of breastfeeding will directly support progress towards achieving MDG 4 through reduced neonatal mortality [ 5 – 7 , 50 ] as well as through improved childhood nutrition with associations reported with reduced moderate wasting and stunting prevalence, and the incidence of acute and persistent diarrhoea in children under 5 years [ 51 ].
The findings of this systematic review suggest that achieving more widespread practice of early breastfeeding initiation hinges on multisector interventions. For instance, access to universal primary education [ 52 ] will resolve the negative impact that lack of education for mothers and fathers has on breastfeeding initiation. This is also not exclusive to South Asia as lack of education is also reported as a factor to early breastfeeding initiation in Nigeria [ 53 ], Ethiopia [ 54 ], Tanzania [ 55 ] and Malawi [ 56 ]. Similarly, promotion of gender equality and empowerment of women [ 52 ], lack of decision making power of mothers is a barrier to early initiation of breastfeeding, which is consistent with findings in Tanzania [ 55 ], and mothers-in-law are often decision makers on pregnancy and childbirth-related practices. Further, progress in maternal health and the promotion of maternal health services such as antenatal appointments, skilled birth attendance and postnatal check-up given their impact on a mother’s decision and capacity to initate breastfeeding within 1 h of delivery. This is pertinent particularly in South Asia where more than half of deliveries in several South Asian countries occur outside health facilities [ 57 ] and home delivery was identified as a barrier to early initiation of breastfeeding. This association between home delivery and delayed breastfeeding initiation is consistent with reports from Nigeria [ 53 ], Tanzania [ 55 ], Ethiopia [ 54 ] and Malawi [ 56 ]. The low use of antenatal check-up is also an observed barrier in Vietnam [ 58 ], Turkey [ 59 ], Malawi [ 56 ] and Nigeria [ 53 ]. These consistencies confirm that promoting and facilitating the use of maternal health services should be prioritised to achieve progress on early initiation of breastfeeding. Actions targeting the factors and specific barriers identified in this review will have a synergistic effect on early breastfeeding initiation and achievement of other development goals.
One of the major findings of this review is the influence of traditional beliefs and role of mother in law on breastfeeding. Traditional feeding practices, such as prelacteal feeds, misperceptions regarding colostrum, and taking advice of priests and mothers in-laws that discourage breastfeeding immediately after birth have been highlighted. Therefore, strategies that engage social and family decision-makers to shape traditional beliefs and attitudes towards safer breastfeeding practices are imperative in South Asia [ 60 ].
Policies are in place to support recommended breastfeeding practices in South Asia. With the exception of India, all South Asian countries have a national IYCF strategy officially adapted by government [ 61 ]. Similarly, all countries have a National Breastfeeding Committee, have adopted the Baby Friendly Hospital Initiative (BFHI), and implement the International Code of Marketing of Breast milk Substitutes [ 61 ]. Yet, the rates of early breastfeeding initiation in the South Asian countries remain some of the lowest in the world [ 1 ]. Filling the gap, identified in this review, in evidence concerning socio-economic and political context that influence breastfeeding practices may lead to better informed and more context-specific policies that impact more significantly. Further, the exploration of factors and barriers presented sheds light on the factors and barriers that undermine the effective implementation of policies at the individual level.
This review was influenced by several limitations thus results should not be interpreted as a necessarily definitive list of all factors and barriers experienced by women in South Asia. As the South Asia region is highly diverse and ever-changing over time, as are the situations within each country, the results of these studies based on their size and scope cannot fully represent the region as a whole. Further, as no studies from Afghanistan and Bhutan met the inclusion criteria these studies and review results may not represent those two countries. However, the inclusion dates were limited and findings presented based on countries and detailing their specify context and participant type where possible to assist the use of the findings per situation.
The nature of the evidence, the lack of strong quality studies by design and sample size, limit the overall strength of the findings however this is not a topic suited to randomised controlled trials therefore this review reflects some of the highest quality that is likely to be generated. Studies classified as ‘weak’ were retained to afford a general sense of the documented factors and barriers however interpretation of the results of those studies is taken with caution and has been noted throughout presentation of the findings. Grey literature was not included thus it is possible that relevant unpublished articles were overlooked however the lack of peer-review for grey literature inflicts quality concerns. The findings are discussed in terms of countries generally however as these are drawn from isolated and qualitative studies with some being very small sample size (six) they are not nationally representative of the factors and barriers, with the exception of eight included studies, in Bangladesh, Nepal, India and Pakistan, that analysed nationally representative surveys and are moderate in quality [ 25 – 30 , 35 , 43 ]. Nevertheless, many factors are highlighted by not only the findings of one study, but also supported by more than one study with both moderate and weak quality grading, and thus the findings can be used to design programs to increase early or timely initiation of breastfeeding and reduce neonatal deaths. Afghanistan and Bhutan rank the lowest, in D-grade, in terms of implementation of the policies and programs of the global strategy on breastfeeding [ 62 ], yet no published studies were identified concerning the factors and barriers from these two countries, highlighting an important research gap.
Attention to raise rates of early breastfeeding initiation in South Asian countries is a public health priority given that the rates of early initiation of breastfeeding in the region is lowest, newborn mortality now accounts for more than half of the U5MR, and early initiation may prevent up to half of the newborn deaths and improve childhood nutritional status. This systematic review reveals that factors associated with and barriers to early initiation of breastfeeding in South Asia are predominantly on specific socioeconomic, health related and individual factors; and demand side barriers. As this study highlighted limited attention and evidence on the influence of the health care system and wider political context we suggest future studies that assess how such systems influence the early initiation of breastfeeding. Studies in Afghanistan and Bhutan would be of value to identify factors specific in these settings as this review found no studies in these countries. Further, the authors recommend national studies with sub-population representative samples providing analysis of the relative magnitude of specific factors which limit breastfeeding initiation to inform the direction of policy and resources for most effective action.
Factors and barriers manifest similarly across the region although contextual variations are observed, thus actions must be both general and aligned to specific settings. Initiatives that span the breadth of factors and directed towards local barriers are urgently needed to increase the practice of breastfeeding initiation within 1 h of birth and achieve greater reductions in neonatal mortality and improved child health in the South Asia region.
UNICEF. State of the World’s Children 2014: every child counts. New York: United Nations Children’s Fund (UNICEF); 2014.
Google Scholar
United Nations. The millennium development goals report 2013. New York: United Nations Publications; 2013. p. 68.
UNICEF, WHO, The World Bank, United Nations Population Division. Levels and trends in child mortality: report 2013. estimates developed by the un inter-agency group for child mortality estimation. New York: United Nations Children’s Fund; 2013.
WHO. Breastfeeding-early initiation: World Health Organization; 2012 [updated 2012]. http://www.who.int/elena/titles/early_breastfeeding/en/ Accessed 5 April 2013.
Khan J, Vesel L, Bahl R, Martines JC. Timing of breastfeeding initiation and exclusivity of breastfeeding during the first month of life: Effects on neonatal mortality and morbidity—a systematic review and meta-analysis. Matern Child Nutr. 2015;19:3.
Mullany LC, Katz J, Li YM, Khatry SK, LeClerq SC, Darmstadt GL, et al. Breast-feeding patterns, time to initiation, and mortality risk among newborns in southern. Nepal J Nutr. 2008;138(3):599–603.
CAS PubMed Google Scholar
Tawiah-Agyemang C, Kirkwood BR, Edmond K, Bazzano A, Hill Z. Early initiation of breast-feeding in Ghana: barriers and facilitators. J Perinatol. 2008;28:S46–52.
Article PubMed Google Scholar
Oddy WH. Breastfeeding in the first hour of life protects against neonatal mortality. J Pediatr. 2013;89(2):109–11.
Article Google Scholar
Jana AK. Interventions for promoting the initiation of breastfeeding The WHO reproductive health library. Geneva: World Health Organization; 2009. http://apps.who.int/rhl/pregnancy_childbirth/care_after_childbirth/cd001688_JanaAK_com/en/ .
Lawn JE, Kerber K, Enweronu-Laryea C, Cousens S. 3.6 Million neonatal deaths - what is progressing and what is not? Semin Perinatol. 2010;34(6):371–86.
Bhutta ZA, Ahmed T, Black RE, Cousens S, Dewey K, Giugliani E, et al. Maternal and child undernutrition 3 - What works? Interventions for maternal and child undernutrition and survival. Lancet. 2008;371(9610):417–40.
Dennis CL. Breastfeeding initiation and duration: A 1990–2000 literature review. JOGNN. 2002;31(1):12–32.
Dyson L, McCormick F, Renfrew MJ. Interventions for promoting the initiation of breastfeeding. Cochrane Database Syst Rev. 2005;2:CD001688.
PubMed Google Scholar
Moore ER, Anderson GC, Bergman N, Dowswell T. Early skin-to-skin contact for mothers and their healthy newborn infants. Cochrane Database Syst Rev. 2012;5:107.
Carfoot S, Williamson PR, Dickson R. A systematic review of randomised controlled trials evaluating the effect of mother/baby skin-to-skin care on successful breastfeeding. Midwifery. 2003;19(2):148–55.
Moher D, Liberati A, Tetzlaff J, Altman D, The PRISMA Group. Preferred Reporting Items for Systematic Reviews and Meta-Analyses: The PRISMA Statement. BMJ. 2009;339:b2535.
Article PubMed PubMed Central Google Scholar
Jacobs B, Ir P, Bigdeli M, Annear P, Van Damme W. Addressing access barriers to health services: an analytical framework for selecting appropriate interventions in low-income Asian countries. Health Policy Plann. 2012;27(4):288–300.
Critical Appraisal Skills Programme. Critical Appraisal Skills Programme (CASP) Qualitative Research Checklist, 2013. http://media.wix.com/ugd/dded87_29c5b002d99342f788c6ac670e49f274.pdf . Accessed 7 August 2013.
National Collaborating Centre for Methods and Tools. Critical appraisal tools to make sense of evidence: Hamilton, ON: McMaster University; 2011 [updated 16 December, 2011]. http://www.nccmt.ca/registry/view/eng/87.html Accessed 15 October 2013.
Armijo-Olivo S, Stiles CR, Hagen NA, Biondo PD, Cummings GG. Assessment of study quality for systematic reviews: a comparison of the cochrane collaboration risk of bias tool and the effective public health practice project quality assessment tool: methodological research. J Eval Clin Pract. 2012;18(1):12–8.
Effective Public Health Practice Project (EPHPP). Quality Assessment Tool for Quantitative Studies, 2009. http://www.ephpp.ca/PDF/Quality%20Assessment%20Tool_2010_2.pdf Accessed 2 June 2013.
The SURE Collaboration (Supporting the Use of Research Evidence). SURE Guide: Checklist for identifying factors affecting the implementation of a policy option. The SURE Collaboration: Geneva; 2011.
Peters D, Mirchandani G, Hansen P. Strategies for engaging the private sector in sexual and reproductive health: how effective are they? Health Policy Plan. 2004;19 Suppl 1:i5–i21.
Ensor T, Cooper S. Overcoming barriers to health service access: influencing the demand side. Health Policy Plan. 2004;19:69–79.
Seranath U, Siriwardena I, Godakandage SSP, Jayawickrama H, Fernando DN, Dibley MJ. Determinants of breastfeeding practices: an analysis of the Sri Lanka demographic and health survey 2006–2007. Matern Child Nutr. 2012;8(3):315–29.
Patel A, Badhoniya N, Khadse S, Senarath U, Agho KE, Dibley MJ, et al. Infant and young child feeding indicators and determinants of poor feeding practices in India: secondary data analysis of National family health survey 2005–06. Food Nutr Bull. 2010;31(2):314–33.
Hazir T, Akram DS, Nisar YB, Kazmi N, Agho KE, Abbasi S, et al. Determinants of suboptimal breast-feeding practices in Pakistan. Public Health Nutr. 2013;16(4):659–72.
Pandey S, Tiwari K, Senarath U, Agho KE, Dibley MJ, South Asia Infant Feeding Research N. Determinants of infant and young child feeding practices in Nepal: secondary data analysis of demographic and health survey 2006. Food Nutr Bull. 2010;31(2):334–51.
Mihrshahi S, Kabir I, Roy SK, Agho KE, Senarath U, Dibley MJ. Determinants of infant and young child feeding practices in Bangladesh: secondary data analysis of demographic and health survey 2004. Food Nutr Bull. 2010;31(2):295–313.
Rahman M, Haque SE, Zahan S, Islam O. Noninstitutional births and newborn care practices among adolescent mothers in Bangladesh. JOGNN. 2011;40(3):262–73.
Subedi N, Paudel S, Rana T, Poudyal AK. Infant and young child feeding practices in Chepang communities. J Nepal Health Res Counc. 2012;10(21):141–6.
Ali S, Ali SF, Imam AM, Ayub S, Billoo AG. Perception and practices of breastfeeding of infants 0–6 months in an urban and a semi-urban community in Pakistan: a cross-sectional study. J Pak Med Assoc. 2011;61(1):99–104.
Dihidar S, Bhattacharya BN, Mukherjee KL. Description of breastfeeding practices among poorer sections in Calcutta Metropolitan area and its impact on postpartum infecundity. J Child Health Care. 2002;6(3):203–19.
Article CAS PubMed Google Scholar
Subba SH, Chandrashekhar TS, Binu VS, Joshi HS, Rana MS, Dixit SB. Infant feeding practices of mothers in an urban area in Nepal. Kathmandu Univ Med J. 2007;5(1):42–7.
CAS Google Scholar
Senarath U, Dibley MJ, Godakandage SSP, Jayawickrama H, Wickramasinghe A, Agho KE, et al. Determinants of infant and young child feeding practices in Sri Lanka: secondary data analysis of demographic and health survey 2000. Food Nutr Bull. 2010;31(2):352–65.
Athavale AV, Athavale SA, Deshpande SG, Zodpey SP, Sangole S. Initiation of breast-feeding by urban women. Health Pop: Perspect Iss. 2004;27(2):117–25.
Badruddin SH, Inam SNB, Ramzanali S, Hendricks K. Constraints to adoption of appropriate breast feeding practices in a squatter settlement in Karachi, Pakistan. J Pak Med Assoc. 1997;47(2):63–8.
Ekambaram M, Vishnu Bhat B, Ahamed MAP. Knowledge, attitiude and practice of breastfeeding among postnatal mothers. Pediatr Res. 2010;14(2):119–24.
Parveen S, Sareen IB, Dahiya BR. Breast feeding practices in post IMNCI era in rural community of Haryana. Indian J Pub Health Res Develop. 2012;3(4):205–9.
Premani ZS, Kurji Z, Mithani Y. To explore the experiences of women on reasons in initiating and maintaining breastfeeding in urban area of Karachi, Pakistan: An exploratory study. ISRN Pediatr. 2011;2011:1–10.
Haider R, Rasheed S, ST G, Hassan N, Pachon H, Islam S, et al. Breastfeeding in infancy: identifying the program-relevant issues in Bangladesh. Int Breastfeed J. 2010;5:21.
Abdulraheem R, Binns CW. The infant feeding practices of mothers in the Maldives. Public Health Nutr. 2007;10(5):502–7.
Dibley MJ, Roy SK, Upul S, Archana P, Kalpana T, Agho KE, et al. Across-country comparisons of selected infant and young child feeding indicators and associated factors in four South Asian countries. Food Nutr Bull. 2010;31(2):366–79.
Kaushal M, Aggarwal R, Singal A, Shukla H, Kapoor SK, Paul VK. Breastfeeding practices and health-seeking behavior for neonatal sickness in a rural community. J Trop Pediatr. 2005;51(6):366–76.
Digra SK, Shirin N. Prevalence and pattern of breast feeding practices in rural women of Jammu. Pediatr OnCall. 2012; 9(1):Art#3.
Fikree FF, Ali TS, Durocher JM, Rahbar MH. Newborn care practices in low socioeconomic settlements of Karachi, Pakistan. Soc Sci Med. 2005;60(5):911–21.
Khadduri R, Marsh DR, Rasmussen B, Bari A, Nazir R, Darmstadt GL. Household knowledge and practices of newborn and maternal health in Haripur district, Pakistan. J Perinatol. 2008;28(3):182–7.
Bandyopadhyay M. Impact of ritual pollution on lactation and breastfeeding practices in rural West Bengal, India. Int Breastfeed J. 2009;4:2.
Moran AC, Choudhury N, Uz Zaman Khan N, Ahsan Karar Z, Wahed T, Faiz Rashid S, et al. Newborn care practices among slum dwellers in Dhaka, Bangladesh: a quantitative and qualitative exploratory study. BMC Pregnancy Childbirth. 2009;9:54.
Edmond KM, Kirkwood BR, Amenga-Etego S, Owusu-Agyei S, Hurt LS. Effect of early infant feeding practices on infection-specific neonatal mortality: an investigation of the causal links with observational data from rural Ghana. Am J Clin Nutr. 2007;86(4):1126–31.
Debes AK, Anjalee K, Walker N, Edmond K, Mullany LC. Time to initiation of breastfeeding and neonatal mortality and morbidity: a systematic review. BMC Public Health. 2013;13(Suppl3):S19.
Lomazzi M, Borisch B, Laaser U. The millennium development goals: experiences, achievements and what’s next. Glob Health Action. 2014;7:1–9.
Waheed Babatunde Y, Samson Babatunde A. Modelling the trend and determinants of breastfeeding initiation in Nigeria. Child Develop Res. 2013;2013:530396.
Setegn T, Gerbaba M, Belachew T. Determinants of timely initiation of breastfeeding among mothers in Goba Woreda, South East Ethiopia: a cross sectional study. BMC Public Health. 2011;11:217.
Victor R, Baines SK, Agho KE, Dibley MJ. Determinants of breastfeeding indicators among children less than 24 months of age in Tanzania: a secondary analysis of the 2010 Tanzania demographic and health survey. BMJ open. 2013;3(1).
Kazembe LN. Spatial modelling of initiation and duration of breastfeeding: analysis of breastfeeding behaviour in Malawi - I. World Health Pop. 2008;10(3):14–31.
Tey N-P, Lai S-l. Correlates of and barriers to the utilization of health services for delivery in South Asia and Sub-Saharan Africa. Sci World J. 2013;2013:423403.
Nguyen PH, Keithly SC, Nguyen NT, Nguyen TT, Tran LM, Hajeebhoy N. Prelacteal feeding practices in Vietnam: challenges and associated factors. BMC Public Health. 2013;13:932.
Orun E, Yalcin SS, Madendag Y, Ustunyurt-Eras Z, Kutluk S, Yurdakok K. Factors associated with breastfeeding initiation time in a Baby-Friendly Hospital. Turk J Pediatr. 2010;52(1):10–6.
Patel A, Banerjee A, Kaletwad A. Factors associated with prelacteal feeding and timely initiation of breastfeeding in hospital-delivered infants in India. J Hum Lact. 2013;29(4):572–8.
BPNI/IBFAN-Asia. Are our babies falling through the gaps? The state of policies and programme implementation of the global strategy for infant and young child feeding in 51 countries. Delhi: IBFAN Africa; 2012.
IBFAN. The State of the World’s breastfeeding: South Asia report card. India: International Baby Food Action Network Asia Pacific; 2006.
Download references
Acknowledgments
This review is a part of the first author’s Master of Public Health research project in The University of Melbourne, Australia. This research received no specific grant from any funding agency, commercial or not-for-profit sectors.
Authors’ contributions
IKS and AB formulated the research question; IKS and AB designed the study scope and methodology; IKS carried out the literature search and screening; IKS carried out initial data analysis followed by review by AB; IKS and AB wrote the manuscript. Both authors read and approved the final manuscript. Both made first revision and approved the final manuscript.
Competing interests
The authors declare that they have no competing interests.
Author information
Authors and affiliations.
Nossal Institute for Global Health, The University of Melbourne, Melbourne, VIC, Australia
Indu K. Sharma & Abbey Byrne
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Indu K. Sharma .
Additional files
Additional file 1:.
Detailed search strategy in one database. (DOCX 26 kb)
Additional file 2:
Detailed characteristics of included studies. (DOC 129 kb)
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License ( http://creativecommons.org/licenses/by/4.0/ ), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated.
Reprints and permissions
About this article
Cite this article.
Sharma, I.K., Byrne, A. Early initiation of breastfeeding: a systematic literature review of factors and barriers in South Asia. Int Breastfeed J 11 , 17 (2016). https://doi.org/10.1186/s13006-016-0076-7
Download citation
Received : 23 November 2015
Accepted : 10 June 2016
Published : 18 June 2016
DOI : https://doi.org/10.1186/s13006-016-0076-7
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Breastfeeding
- Early initiation of breastfeeding
- Timely initiation of breastfeeding
- Breastfeeding within 1 h of birth
International Breastfeeding Journal
ISSN: 1746-4358
- General enquiries: [email protected]

IMAGES
VIDEO
COMMENTS
This scoping review examined the existing empirical literature on women’s perceptions about and experiences of breastfeeding to identify how public health messaging can be tailored to improve breastfeeding rates.
Understanding the factors that influence infant feeding will help in promotion, protecting and supporting breast feeding. This review identified the determinants of infant feeding practices and...
In this Series paper, we examine how mother and baby attributes at the individual level interact with breastfeeding determinants at other levels, how these interactions drive breastfeeding outcomes, and what policies and interventions are necessary to achieve optimal breastfeeding.
Worldwide, breastfeeding saves the lives of infants and reduces their disease burden. Breastfeeding also reduces the disease burden for mothers. This article examines who chooses to breastfeed and for how long in the American context.
There is a need to know how effective breastfeeding interventions are in reaching the intended population; how well they work in promoting breastfeeding initiation and continuation; and how successful they are when implemented at the setting and staff level.
This study highlights the growing body of literature on effective interventions that address breastfeeding barriers. The literature suffers from some methodological challenges and continues to be primarily focused on high- and upper-middle income settings.
This review supports the hypothesis that breastfeeding is protective against breast and ovarian carcinoma, and exclusive breastfeeding and predominant breastfeeding increase the duration of lactational amenorrhoea.
There is a need to know how effective breastfeeding interventions are in reaching the intended population; how well they work in promoting breastfeeding initiation and continuation; and how successful they are when implemented at the setting and staff level.
Seven key factors in relation to breastfeeding initiation and support following early discharge were identified, namely trust and security, consistent advice, practical breastfeeding support, breastfeeding education, comfortable environment, positive attitudes and emotional support, and individualised care.
This systematic literature review synthesises published evidence on the factors and barriers associated with the initiation of breastfeeding within 1 h of birth in South Asian countries to inform a future of relevant, context-specific actions.