Have a language expert improve your writing
Run a free plagiarism check in 10 minutes, generate accurate citations for free.
- Knowledge Base
Methodology
- How to Write a Literature Review | Guide, Examples, & Templates

How to Write a Literature Review | Guide, Examples, & Templates
Published on January 2, 2023 by Shona McCombes . Revised on September 11, 2023.
What is a literature review? A literature review is a survey of scholarly sources on a specific topic. It provides an overview of current knowledge, allowing you to identify relevant theories, methods, and gaps in the existing research that you can later apply to your paper, thesis, or dissertation topic .
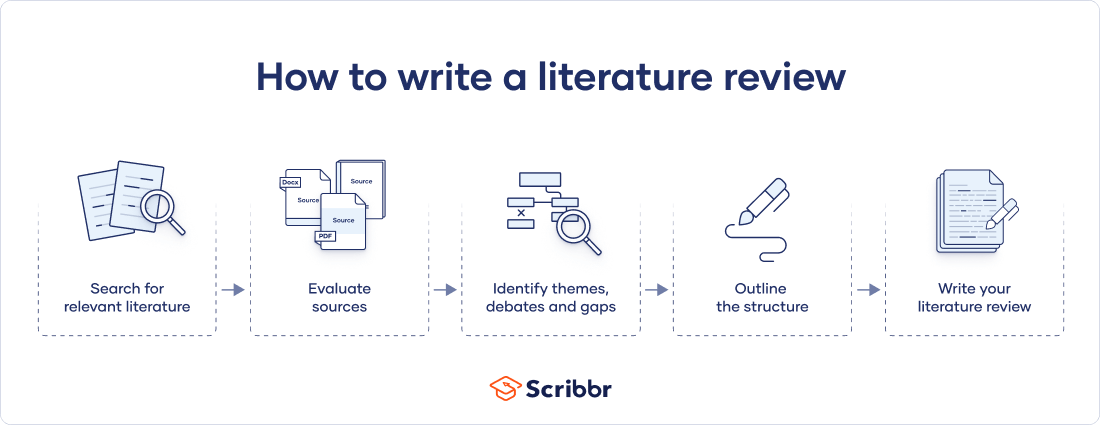
There are five key steps to writing a literature review:
- Search for relevant literature
- Evaluate sources
- Identify themes, debates, and gaps
- Outline the structure
- Write your literature review
A good literature review doesn’t just summarize sources—it analyzes, synthesizes , and critically evaluates to give a clear picture of the state of knowledge on the subject.
Instantly correct all language mistakes in your text
Upload your document to correct all your mistakes in minutes

Table of contents
What is the purpose of a literature review, examples of literature reviews, step 1 – search for relevant literature, step 2 – evaluate and select sources, step 3 – identify themes, debates, and gaps, step 4 – outline your literature review’s structure, step 5 – write your literature review, free lecture slides, other interesting articles, frequently asked questions, introduction.
- Quick Run-through
- Step 1 & 2
When you write a thesis , dissertation , or research paper , you will likely have to conduct a literature review to situate your research within existing knowledge. The literature review gives you a chance to:
- Demonstrate your familiarity with the topic and its scholarly context
- Develop a theoretical framework and methodology for your research
- Position your work in relation to other researchers and theorists
- Show how your research addresses a gap or contributes to a debate
- Evaluate the current state of research and demonstrate your knowledge of the scholarly debates around your topic.
Writing literature reviews is a particularly important skill if you want to apply for graduate school or pursue a career in research. We’ve written a step-by-step guide that you can follow below.
Prevent plagiarism. Run a free check.
Writing literature reviews can be quite challenging! A good starting point could be to look at some examples, depending on what kind of literature review you’d like to write.
- Example literature review #1: “Why Do People Migrate? A Review of the Theoretical Literature” ( Theoretical literature review about the development of economic migration theory from the 1950s to today.)
- Example literature review #2: “Literature review as a research methodology: An overview and guidelines” ( Methodological literature review about interdisciplinary knowledge acquisition and production.)
- Example literature review #3: “The Use of Technology in English Language Learning: A Literature Review” ( Thematic literature review about the effects of technology on language acquisition.)
- Example literature review #4: “Learners’ Listening Comprehension Difficulties in English Language Learning: A Literature Review” ( Chronological literature review about how the concept of listening skills has changed over time.)
You can also check out our templates with literature review examples and sample outlines at the links below.
Download Word doc Download Google doc
Before you begin searching for literature, you need a clearly defined topic .
If you are writing the literature review section of a dissertation or research paper, you will search for literature related to your research problem and questions .
Make a list of keywords
Start by creating a list of keywords related to your research question. Include each of the key concepts or variables you’re interested in, and list any synonyms and related terms. You can add to this list as you discover new keywords in the process of your literature search.
- Social media, Facebook, Instagram, Twitter, Snapchat, TikTok
- Body image, self-perception, self-esteem, mental health
- Generation Z, teenagers, adolescents, youth
Search for relevant sources
Use your keywords to begin searching for sources. Some useful databases to search for journals and articles include:
- Your university’s library catalogue
- Google Scholar
- Project Muse (humanities and social sciences)
- Medline (life sciences and biomedicine)
- EconLit (economics)
- Inspec (physics, engineering and computer science)
You can also use boolean operators to help narrow down your search.
Make sure to read the abstract to find out whether an article is relevant to your question. When you find a useful book or article, you can check the bibliography to find other relevant sources.
You likely won’t be able to read absolutely everything that has been written on your topic, so it will be necessary to evaluate which sources are most relevant to your research question.
For each publication, ask yourself:
- What question or problem is the author addressing?
- What are the key concepts and how are they defined?
- What are the key theories, models, and methods?
- Does the research use established frameworks or take an innovative approach?
- What are the results and conclusions of the study?
- How does the publication relate to other literature in the field? Does it confirm, add to, or challenge established knowledge?
- What are the strengths and weaknesses of the research?
Make sure the sources you use are credible , and make sure you read any landmark studies and major theories in your field of research.
You can use our template to summarize and evaluate sources you’re thinking about using. Click on either button below to download.
Take notes and cite your sources
As you read, you should also begin the writing process. Take notes that you can later incorporate into the text of your literature review.
It is important to keep track of your sources with citations to avoid plagiarism . It can be helpful to make an annotated bibliography , where you compile full citation information and write a paragraph of summary and analysis for each source. This helps you remember what you read and saves time later in the process.
To begin organizing your literature review’s argument and structure, be sure you understand the connections and relationships between the sources you’ve read. Based on your reading and notes, you can look for:
- Trends and patterns (in theory, method or results): do certain approaches become more or less popular over time?
- Themes: what questions or concepts recur across the literature?
- Debates, conflicts and contradictions: where do sources disagree?
- Pivotal publications: are there any influential theories or studies that changed the direction of the field?
- Gaps: what is missing from the literature? Are there weaknesses that need to be addressed?
This step will help you work out the structure of your literature review and (if applicable) show how your own research will contribute to existing knowledge.
- Most research has focused on young women.
- There is an increasing interest in the visual aspects of social media.
- But there is still a lack of robust research on highly visual platforms like Instagram and Snapchat—this is a gap that you could address in your own research.
There are various approaches to organizing the body of a literature review. Depending on the length of your literature review, you can combine several of these strategies (for example, your overall structure might be thematic, but each theme is discussed chronologically).
Chronological
The simplest approach is to trace the development of the topic over time. However, if you choose this strategy, be careful to avoid simply listing and summarizing sources in order.
Try to analyze patterns, turning points and key debates that have shaped the direction of the field. Give your interpretation of how and why certain developments occurred.
If you have found some recurring central themes, you can organize your literature review into subsections that address different aspects of the topic.
For example, if you are reviewing literature about inequalities in migrant health outcomes, key themes might include healthcare policy, language barriers, cultural attitudes, legal status, and economic access.
Methodological
If you draw your sources from different disciplines or fields that use a variety of research methods , you might want to compare the results and conclusions that emerge from different approaches. For example:
- Look at what results have emerged in qualitative versus quantitative research
- Discuss how the topic has been approached by empirical versus theoretical scholarship
- Divide the literature into sociological, historical, and cultural sources
Theoretical
A literature review is often the foundation for a theoretical framework . You can use it to discuss various theories, models, and definitions of key concepts.
You might argue for the relevance of a specific theoretical approach, or combine various theoretical concepts to create a framework for your research.
Like any other academic text , your literature review should have an introduction , a main body, and a conclusion . What you include in each depends on the objective of your literature review.
The introduction should clearly establish the focus and purpose of the literature review.
Depending on the length of your literature review, you might want to divide the body into subsections. You can use a subheading for each theme, time period, or methodological approach.
As you write, you can follow these tips:
- Summarize and synthesize: give an overview of the main points of each source and combine them into a coherent whole
- Analyze and interpret: don’t just paraphrase other researchers — add your own interpretations where possible, discussing the significance of findings in relation to the literature as a whole
- Critically evaluate: mention the strengths and weaknesses of your sources
- Write in well-structured paragraphs: use transition words and topic sentences to draw connections, comparisons and contrasts
In the conclusion, you should summarize the key findings you have taken from the literature and emphasize their significance.
When you’ve finished writing and revising your literature review, don’t forget to proofread thoroughly before submitting. Not a language expert? Check out Scribbr’s professional proofreading services !
This article has been adapted into lecture slides that you can use to teach your students about writing a literature review.
Scribbr slides are free to use, customize, and distribute for educational purposes.
Open Google Slides Download PowerPoint
If you want to know more about the research process , methodology , research bias , or statistics , make sure to check out some of our other articles with explanations and examples.
- Sampling methods
- Simple random sampling
- Stratified sampling
- Cluster sampling
- Likert scales
- Reproducibility
Statistics
- Null hypothesis
- Statistical power
- Probability distribution
- Effect size
- Poisson distribution
Research bias
- Optimism bias
- Cognitive bias
- Implicit bias
- Hawthorne effect
- Anchoring bias
- Explicit bias
A literature review is a survey of scholarly sources (such as books, journal articles, and theses) related to a specific topic or research question .
It is often written as part of a thesis, dissertation , or research paper , in order to situate your work in relation to existing knowledge.
There are several reasons to conduct a literature review at the beginning of a research project:
- To familiarize yourself with the current state of knowledge on your topic
- To ensure that you’re not just repeating what others have already done
- To identify gaps in knowledge and unresolved problems that your research can address
- To develop your theoretical framework and methodology
- To provide an overview of the key findings and debates on the topic
Writing the literature review shows your reader how your work relates to existing research and what new insights it will contribute.
The literature review usually comes near the beginning of your thesis or dissertation . After the introduction , it grounds your research in a scholarly field and leads directly to your theoretical framework or methodology .
A literature review is a survey of credible sources on a topic, often used in dissertations , theses, and research papers . Literature reviews give an overview of knowledge on a subject, helping you identify relevant theories and methods, as well as gaps in existing research. Literature reviews are set up similarly to other academic texts , with an introduction , a main body, and a conclusion .
An annotated bibliography is a list of source references that has a short description (called an annotation ) for each of the sources. It is often assigned as part of the research process for a paper .
Cite this Scribbr article
If you want to cite this source, you can copy and paste the citation or click the “Cite this Scribbr article” button to automatically add the citation to our free Citation Generator.
McCombes, S. (2023, September 11). How to Write a Literature Review | Guide, Examples, & Templates. Scribbr. Retrieved August 19, 2024, from https://www.scribbr.com/dissertation/literature-review/
Is this article helpful?
Shona McCombes
Other students also liked, what is a theoretical framework | guide to organizing, what is a research methodology | steps & tips, how to write a research proposal | examples & templates, what is your plagiarism score.
Methodological Approaches to Literature Review
- Living reference work entry
- First Online: 09 May 2023
- Cite this living reference work entry

- Dennis Thomas 2 ,
- Elida Zairina 3 &
- Johnson George 4
716 Accesses
1 Citations
The literature review can serve various functions in the contexts of education and research. It aids in identifying knowledge gaps, informing research methodology, and developing a theoretical framework during the planning stages of a research study or project, as well as reporting of review findings in the context of the existing literature. This chapter discusses the methodological approaches to conducting a literature review and offers an overview of different types of reviews. There are various types of reviews, including narrative reviews, scoping reviews, and systematic reviews with reporting strategies such as meta-analysis and meta-synthesis. Review authors should consider the scope of the literature review when selecting a type and method. Being focused is essential for a successful review; however, this must be balanced against the relevance of the review to a broad audience.
This is a preview of subscription content, log in via an institution to check access.
Access this chapter
Institutional subscriptions
Similar content being viewed by others

Reviewing Literature for and as Research

Discussion and Conclusion

Systematic Reviews in Educational Research: Methodology, Perspectives and Application
Akobeng AK. Principles of evidence based medicine. Arch Dis Child. 2005;90(8):837–40.
Article CAS PubMed PubMed Central Google Scholar
Alharbi A, Stevenson M. Refining Boolean queries to identify relevant studies for systematic review updates. J Am Med Inform Assoc. 2020;27(11):1658–66.
Article PubMed PubMed Central Google Scholar
Arksey H, O’Malley L. Scoping studies: towards a methodological framework. Int J Soc Res Methodol. 2005;8(1):19–32.
Article Google Scholar
Aromataris E MZE. JBI manual for evidence synthesis. 2020.
Google Scholar
Aromataris E, Pearson A. The systematic review: an overview. Am J Nurs. 2014;114(3):53–8.
Article PubMed Google Scholar
Aromataris E, Riitano D. Constructing a search strategy and searching for evidence. A guide to the literature search for a systematic review. Am J Nurs. 2014;114(5):49–56.
Babineau J. Product review: covidence (systematic review software). J Canad Health Libr Assoc Canada. 2014;35(2):68–71.
Baker JD. The purpose, process, and methods of writing a literature review. AORN J. 2016;103(3):265–9.
Bastian H, Glasziou P, Chalmers I. Seventy-five trials and eleven systematic reviews a day: how will we ever keep up? PLoS Med. 2010;7(9):e1000326.
Bramer WM, Rethlefsen ML, Kleijnen J, Franco OH. Optimal database combinations for literature searches in systematic reviews: a prospective exploratory study. Syst Rev. 2017;6(1):1–12.
Brown D. A review of the PubMed PICO tool: using evidence-based practice in health education. Health Promot Pract. 2020;21(4):496–8.
Cargo M, Harris J, Pantoja T, et al. Cochrane qualitative and implementation methods group guidance series – paper 4: methods for assessing evidence on intervention implementation. J Clin Epidemiol. 2018;97:59–69.
Cook DJ, Mulrow CD, Haynes RB. Systematic reviews: synthesis of best evidence for clinical decisions. Ann Intern Med. 1997;126(5):376–80.
Article CAS PubMed Google Scholar
Counsell C. Formulating questions and locating primary studies for inclusion in systematic reviews. Ann Intern Med. 1997;127(5):380–7.
Cummings SR, Browner WS, Hulley SB. Conceiving the research question and developing the study plan. In: Cummings SR, Browner WS, Hulley SB, editors. Designing Clinical Research: An Epidemiological Approach. 4th ed. Philadelphia (PA): P Lippincott Williams & Wilkins; 2007. p. 14–22.
Eriksen MB, Frandsen TF. The impact of patient, intervention, comparison, outcome (PICO) as a search strategy tool on literature search quality: a systematic review. JMLA. 2018;106(4):420.
Ferrari R. Writing narrative style literature reviews. Medical Writing. 2015;24(4):230–5.
Flemming K, Booth A, Hannes K, Cargo M, Noyes J. Cochrane qualitative and implementation methods group guidance series – paper 6: reporting guidelines for qualitative, implementation, and process evaluation evidence syntheses. J Clin Epidemiol. 2018;97:79–85.
Grant MJ, Booth A. A typology of reviews: an analysis of 14 review types and associated methodologies. Health Inf Libr J. 2009;26(2):91–108.
Green BN, Johnson CD, Adams A. Writing narrative literature reviews for peer-reviewed journals: secrets of the trade. J Chiropr Med. 2006;5(3):101–17.
Gregory AT, Denniss AR. An introduction to writing narrative and systematic reviews; tasks, tips and traps for aspiring authors. Heart Lung Circ. 2018;27(7):893–8.
Harden A, Thomas J, Cargo M, et al. Cochrane qualitative and implementation methods group guidance series – paper 5: methods for integrating qualitative and implementation evidence within intervention effectiveness reviews. J Clin Epidemiol. 2018;97:70–8.
Harris JL, Booth A, Cargo M, et al. Cochrane qualitative and implementation methods group guidance series – paper 2: methods for question formulation, searching, and protocol development for qualitative evidence synthesis. J Clin Epidemiol. 2018;97:39–48.
Higgins J, Thomas J. In: Chandler J, Cumpston M, Li T, Page MJ, Welch VA, editors. Cochrane Handbook for Systematic Reviews of Interventions version 6.3, updated February 2022). Available from www.training.cochrane.org/handbook.: Cochrane; 2022.
International prospective register of systematic reviews (PROSPERO). Available from https://www.crd.york.ac.uk/prospero/ .
Khan KS, Kunz R, Kleijnen J, Antes G. Five steps to conducting a systematic review. J R Soc Med. 2003;96(3):118–21.
Landhuis E. Scientific literature: information overload. Nature. 2016;535(7612):457–8.
Lockwood C, Porritt K, Munn Z, Rittenmeyer L, Salmond S, Bjerrum M, Loveday H, Carrier J, Stannard D. Chapter 2: Systematic reviews of qualitative evidence. In: Aromataris E, Munn Z, editors. JBI Manual for Evidence Synthesis. JBI; 2020. Available from https://synthesismanual.jbi.global . https://doi.org/10.46658/JBIMES-20-03 .
Chapter Google Scholar
Lorenzetti DL, Topfer L-A, Dennett L, Clement F. Value of databases other than medline for rapid health technology assessments. Int J Technol Assess Health Care. 2014;30(2):173–8.
Moher D, Liberati A, Tetzlaff J, Altman DG, the PRISMA Group. Preferred reporting items for (SR) and meta-analyses: the PRISMA statement. Ann Intern Med. 2009;6:264–9.
Mulrow CD. Systematic reviews: rationale for systematic reviews. BMJ. 1994;309(6954):597–9.
Munn Z, Peters MDJ, Stern C, Tufanaru C, McArthur A, Aromataris E. Systematic review or scoping review? Guidance for authors when choosing between a systematic or scoping review approach. BMC Med Res Methodol. 2018;18(1):143.
Munthe-Kaas HM, Glenton C, Booth A, Noyes J, Lewin S. Systematic mapping of existing tools to appraise methodological strengths and limitations of qualitative research: first stage in the development of the CAMELOT tool. BMC Med Res Methodol. 2019;19(1):1–13.
Murphy CM. Writing an effective review article. J Med Toxicol. 2012;8(2):89–90.
NHMRC. Guidelines for guidelines: assessing risk of bias. Available at https://nhmrc.gov.au/guidelinesforguidelines/develop/assessing-risk-bias . Last published 29 August 2019. Accessed 29 Aug 2022.
Noyes J, Booth A, Cargo M, et al. Cochrane qualitative and implementation methods group guidance series – paper 1: introduction. J Clin Epidemiol. 2018b;97:35–8.
Noyes J, Booth A, Flemming K, et al. Cochrane qualitative and implementation methods group guidance series – paper 3: methods for assessing methodological limitations, data extraction and synthesis, and confidence in synthesized qualitative findings. J Clin Epidemiol. 2018a;97:49–58.
Noyes J, Booth A, Moore G, Flemming K, Tunçalp Ö, Shakibazadeh E. Synthesising quantitative and qualitative evidence to inform guidelines on complex interventions: clarifying the purposes, designs and outlining some methods. BMJ Glob Health. 2019;4(Suppl 1):e000893.
Peters MD, Godfrey CM, Khalil H, McInerney P, Parker D, Soares CB. Guidance for conducting systematic scoping reviews. Int J Evid Healthcare. 2015;13(3):141–6.
Polanin JR, Pigott TD, Espelage DL, Grotpeter JK. Best practice guidelines for abstract screening large-evidence systematic reviews and meta-analyses. Res Synth Methods. 2019;10(3):330–42.
Article PubMed Central Google Scholar
Shea BJ, Grimshaw JM, Wells GA, et al. Development of AMSTAR: a measurement tool to assess the methodological quality of systematic reviews. BMC Med Res Methodol. 2007;7(1):1–7.
Shea BJ, Reeves BC, Wells G, et al. AMSTAR 2: a critical appraisal tool for systematic reviews that include randomised or non-randomised studies of healthcare interventions, or both. Brit Med J. 2017;358
Sterne JA, Hernán MA, Reeves BC, et al. ROBINS-I: a tool for assessing risk of bias in non-randomised studies of interventions. Br Med J. 2016;355
Stroup DF, Berlin JA, Morton SC, et al. Meta-analysis of observational studies in epidemiology: a proposal for reporting. JAMA. 2000;283(15):2008–12.
Tawfik GM, Dila KAS, Mohamed MYF, et al. A step by step guide for conducting a systematic review and meta-analysis with simulation data. Trop Med Health. 2019;47(1):1–9.
The Critical Appraisal Program. Critical appraisal skills program. Available at https://casp-uk.net/ . 2022. Accessed 29 Aug 2022.
The University of Melbourne. Writing a literature review in Research Techniques 2022. Available at https://students.unimelb.edu.au/academic-skills/explore-our-resources/research-techniques/reviewing-the-literature . Accessed 29 Aug 2022.
The Writing Center University of Winconsin-Madison. Learn how to write a literature review in The Writer’s Handbook – Academic Professional Writing. 2022. Available at https://writing.wisc.edu/handbook/assignments/reviewofliterature/ . Accessed 29 Aug 2022.
Thompson SG, Sharp SJ. Explaining heterogeneity in meta-analysis: a comparison of methods. Stat Med. 1999;18(20):2693–708.
Tricco AC, Lillie E, Zarin W, et al. A scoping review on the conduct and reporting of scoping reviews. BMC Med Res Methodol. 2016;16(1):15.
Tricco AC, Lillie E, Zarin W, et al. PRISMA extension for scoping reviews (PRISMA-ScR): checklist and explanation. Ann Intern Med. 2018;169(7):467–73.
Yoneoka D, Henmi M. Clinical heterogeneity in random-effect meta-analysis: between-study boundary estimate problem. Stat Med. 2019;38(21):4131–45.
Yuan Y, Hunt RH. Systematic reviews: the good, the bad, and the ugly. Am J Gastroenterol. 2009;104(5):1086–92.
Download references
Author information
Authors and affiliations.
Centre of Excellence in Treatable Traits, College of Health, Medicine and Wellbeing, University of Newcastle, Hunter Medical Research Institute Asthma and Breathing Programme, Newcastle, NSW, Australia
Dennis Thomas
Department of Pharmacy Practice, Faculty of Pharmacy, Universitas Airlangga, Surabaya, Indonesia
Elida Zairina
Centre for Medicine Use and Safety, Monash Institute of Pharmaceutical Sciences, Faculty of Pharmacy and Pharmaceutical Sciences, Monash University, Parkville, VIC, Australia
Johnson George
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Johnson George .
Section Editor information
College of Pharmacy, Qatar University, Doha, Qatar
Derek Charles Stewart
Department of Pharmacy, University of Huddersfield, Huddersfield, United Kingdom
Zaheer-Ud-Din Babar
Rights and permissions
Reprints and permissions
Copyright information
© 2023 Springer Nature Switzerland AG
About this entry
Cite this entry.
Thomas, D., Zairina, E., George, J. (2023). Methodological Approaches to Literature Review. In: Encyclopedia of Evidence in Pharmaceutical Public Health and Health Services Research in Pharmacy. Springer, Cham. https://doi.org/10.1007/978-3-030-50247-8_57-1
Download citation
DOI : https://doi.org/10.1007/978-3-030-50247-8_57-1
Received : 22 February 2023
Accepted : 22 February 2023
Published : 09 May 2023
Publisher Name : Springer, Cham
Print ISBN : 978-3-030-50247-8
Online ISBN : 978-3-030-50247-8
eBook Packages : Springer Reference Biomedicine and Life Sciences Reference Module Biomedical and Life Sciences
- Publish with us
Policies and ethics
- Find a journal
- Track your research

How To Write An A-Grade Literature Review
3 straightforward steps (with examples) + free template.
By: Derek Jansen (MBA) | Expert Reviewed By: Dr. Eunice Rautenbach | October 2019
Quality research is about building onto the existing work of others , “standing on the shoulders of giants”, as Newton put it. The literature review chapter of your dissertation, thesis or research project is where you synthesise this prior work and lay the theoretical foundation for your own research.
Long story short, this chapter is a pretty big deal, which is why you want to make sure you get it right . In this post, I’ll show you exactly how to write a literature review in three straightforward steps, so you can conquer this vital chapter (the smart way).
Overview: The Literature Review Process
- Understanding the “ why “
- Finding the relevant literature
- Cataloguing and synthesising the information
- Outlining & writing up your literature review
- Example of a literature review
But first, the “why”…
Before we unpack how to write the literature review chapter, we’ve got to look at the why . To put it bluntly, if you don’t understand the function and purpose of the literature review process, there’s no way you can pull it off well. So, what exactly is the purpose of the literature review?
Well, there are (at least) four core functions:
- For you to gain an understanding (and demonstrate this understanding) of where the research is at currently, what the key arguments and disagreements are.
- For you to identify the gap(s) in the literature and then use this as justification for your own research topic.
- To help you build a conceptual framework for empirical testing (if applicable to your research topic).
- To inform your methodological choices and help you source tried and tested questionnaires (for interviews ) and measurement instruments (for surveys ).
Most students understand the first point but don’t give any thought to the rest. To get the most from the literature review process, you must keep all four points front of mind as you review the literature (more on this shortly), or you’ll land up with a wonky foundation.
Okay – with the why out the way, let’s move on to the how . As mentioned above, writing your literature review is a process, which I’ll break down into three steps:
- Finding the most suitable literature
- Understanding , distilling and organising the literature
- Planning and writing up your literature review chapter
Importantly, you must complete steps one and two before you start writing up your chapter. I know it’s very tempting, but don’t try to kill two birds with one stone and write as you read. You’ll invariably end up wasting huge amounts of time re-writing and re-shaping, or you’ll just land up with a disjointed, hard-to-digest mess . Instead, you need to read first and distil the information, then plan and execute the writing.

Step 1: Find the relevant literature
Naturally, the first step in the literature review journey is to hunt down the existing research that’s relevant to your topic. While you probably already have a decent base of this from your research proposal , you need to expand on this substantially in the dissertation or thesis itself.
Essentially, you need to be looking for any existing literature that potentially helps you answer your research question (or develop it, if that’s not yet pinned down). There are numerous ways to find relevant literature, but I’ll cover my top four tactics here. I’d suggest combining all four methods to ensure that nothing slips past you:
Method 1 – Google Scholar Scrubbing
Google’s academic search engine, Google Scholar , is a great starting point as it provides a good high-level view of the relevant journal articles for whatever keyword you throw at it. Most valuably, it tells you how many times each article has been cited, which gives you an idea of how credible (or at least, popular) it is. Some articles will be free to access, while others will require an account, which brings us to the next method.
Method 2 – University Database Scrounging
Generally, universities provide students with access to an online library, which provides access to many (but not all) of the major journals.
So, if you find an article using Google Scholar that requires paid access (which is quite likely), search for that article in your university’s database – if it’s listed there, you’ll have access. Note that, generally, the search engine capabilities of these databases are poor, so make sure you search for the exact article name, or you might not find it.
Method 3 – Journal Article Snowballing
At the end of every academic journal article, you’ll find a list of references. As with any academic writing, these references are the building blocks of the article, so if the article is relevant to your topic, there’s a good chance a portion of the referenced works will be too. Do a quick scan of the titles and see what seems relevant, then search for the relevant ones in your university’s database.
Method 4 – Dissertation Scavenging
Similar to Method 3 above, you can leverage other students’ dissertations. All you have to do is skim through literature review chapters of existing dissertations related to your topic and you’ll find a gold mine of potential literature. Usually, your university will provide you with access to previous students’ dissertations, but you can also find a much larger selection in the following databases:
- Open Access Theses & Dissertations
- Stanford SearchWorks
Keep in mind that dissertations and theses are not as academically sound as published, peer-reviewed journal articles (because they’re written by students, not professionals), so be sure to check the credibility of any sources you find using this method. You can do this by assessing the citation count of any given article in Google Scholar. If you need help with assessing the credibility of any article, or with finding relevant research in general, you can chat with one of our Research Specialists .
Alright – with a good base of literature firmly under your belt, it’s time to move onto the next step.
Need a helping hand?
Step 2: Log, catalogue and synthesise
Once you’ve built a little treasure trove of articles, it’s time to get reading and start digesting the information – what does it all mean?
While I present steps one and two (hunting and digesting) as sequential, in reality, it’s more of a back-and-forth tango – you’ll read a little , then have an idea, spot a new citation, or a new potential variable, and then go back to searching for articles. This is perfectly natural – through the reading process, your thoughts will develop , new avenues might crop up, and directional adjustments might arise. This is, after all, one of the main purposes of the literature review process (i.e. to familiarise yourself with the current state of research in your field).
As you’re working through your treasure chest, it’s essential that you simultaneously start organising the information. There are three aspects to this:
- Logging reference information
- Building an organised catalogue
- Distilling and synthesising the information
I’ll discuss each of these below:
2.1 – Log the reference information
As you read each article, you should add it to your reference management software. I usually recommend Mendeley for this purpose (see the Mendeley 101 video below), but you can use whichever software you’re comfortable with. Most importantly, make sure you load EVERY article you read into your reference manager, even if it doesn’t seem very relevant at the time.
2.2 – Build an organised catalogue
In the beginning, you might feel confident that you can remember who said what, where, and what their main arguments were. Trust me, you won’t. If you do a thorough review of the relevant literature (as you must!), you’re going to read many, many articles, and it’s simply impossible to remember who said what, when, and in what context . Also, without the bird’s eye view that a catalogue provides, you’ll miss connections between various articles, and have no view of how the research developed over time. Simply put, it’s essential to build your own catalogue of the literature.
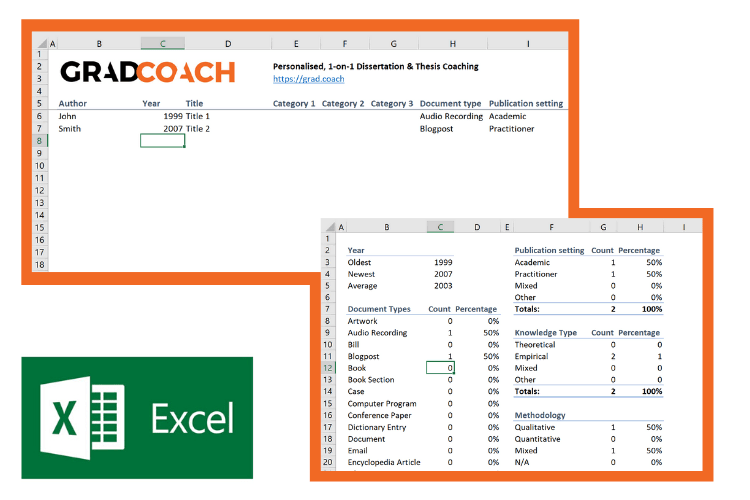
I would suggest using Excel to build your catalogue, as it allows you to run filters, colour code and sort – all very useful when your list grows large (which it will). How you lay your spreadsheet out is up to you, but I’d suggest you have the following columns (at minimum):
- Author, date, title – Start with three columns containing this core information. This will make it easy for you to search for titles with certain words, order research by date, or group by author.
- Categories or keywords – You can either create multiple columns, one for each category/theme and then tick the relevant categories, or you can have one column with keywords.
- Key arguments/points – Use this column to succinctly convey the essence of the article, the key arguments and implications thereof for your research.
- Context – Note the socioeconomic context in which the research was undertaken. For example, US-based, respondents aged 25-35, lower- income, etc. This will be useful for making an argument about gaps in the research.
- Methodology – Note which methodology was used and why. Also, note any issues you feel arise due to the methodology. Again, you can use this to make an argument about gaps in the research.
- Quotations – Note down any quoteworthy lines you feel might be useful later.
- Notes – Make notes about anything not already covered. For example, linkages to or disagreements with other theories, questions raised but unanswered, shortcomings or limitations, and so forth.
If you’d like, you can try out our free catalog template here (see screenshot below).
2.3 – Digest and synthesise
Most importantly, as you work through the literature and build your catalogue, you need to synthesise all the information in your own mind – how does it all fit together? Look for links between the various articles and try to develop a bigger picture view of the state of the research. Some important questions to ask yourself are:
- What answers does the existing research provide to my own research questions ?
- Which points do the researchers agree (and disagree) on?
- How has the research developed over time?
- Where do the gaps in the current research lie?
To help you develop a big-picture view and synthesise all the information, you might find mind mapping software such as Freemind useful. Alternatively, if you’re a fan of physical note-taking, investing in a large whiteboard might work for you.
Step 3: Outline and write it up!
Once you’re satisfied that you have digested and distilled all the relevant literature in your mind, it’s time to put pen to paper (or rather, fingers to keyboard). There are two steps here – outlining and writing:
3.1 – Draw up your outline
Having spent so much time reading, it might be tempting to just start writing up without a clear structure in mind. However, it’s critically important to decide on your structure and develop a detailed outline before you write anything. Your literature review chapter needs to present a clear, logical and an easy to follow narrative – and that requires some planning. Don’t try to wing it!
Naturally, you won’t always follow the plan to the letter, but without a detailed outline, you’re more than likely going to end up with a disjointed pile of waffle , and then you’re going to spend a far greater amount of time re-writing, hacking and patching. The adage, “measure twice, cut once” is very suitable here.
In terms of structure, the first decision you’ll have to make is whether you’ll lay out your review thematically (into themes) or chronologically (by date/period). The right choice depends on your topic, research objectives and research questions, which we discuss in this article .
Once that’s decided, you need to draw up an outline of your entire chapter in bullet point format. Try to get as detailed as possible, so that you know exactly what you’ll cover where, how each section will connect to the next, and how your entire argument will develop throughout the chapter. Also, at this stage, it’s a good idea to allocate rough word count limits for each section, so that you can identify word count problems before you’ve spent weeks or months writing!
PS – check out our free literature review chapter template…
3.2 – Get writing
With a detailed outline at your side, it’s time to start writing up (finally!). At this stage, it’s common to feel a bit of writer’s block and find yourself procrastinating under the pressure of finally having to put something on paper. To help with this, remember that the objective of the first draft is not perfection – it’s simply to get your thoughts out of your head and onto paper, after which you can refine them. The structure might change a little, the word count allocations might shift and shuffle, and you might add or remove a section – that’s all okay. Don’t worry about all this on your first draft – just get your thoughts down on paper.

Once you’ve got a full first draft (however rough it may be), step away from it for a day or two (longer if you can) and then come back at it with fresh eyes. Pay particular attention to the flow and narrative – does it fall fit together and flow from one section to another smoothly? Now’s the time to try to improve the linkage from each section to the next, tighten up the writing to be more concise, trim down word count and sand it down into a more digestible read.
Once you’ve done that, give your writing to a friend or colleague who is not a subject matter expert and ask them if they understand the overall discussion. The best way to assess this is to ask them to explain the chapter back to you. This technique will give you a strong indication of which points were clearly communicated and which weren’t. If you’re working with Grad Coach, this is a good time to have your Research Specialist review your chapter.
Finally, tighten it up and send it off to your supervisor for comment. Some might argue that you should be sending your work to your supervisor sooner than this (indeed your university might formally require this), but in my experience, supervisors are extremely short on time (and often patience), so, the more refined your chapter is, the less time they’ll waste on addressing basic issues (which you know about already) and the more time they’ll spend on valuable feedback that will increase your mark-earning potential.
Literature Review Example
In the video below, we unpack an actual literature review so that you can see how all the core components come together in reality.
Let’s Recap
In this post, we’ve covered how to research and write up a high-quality literature review chapter. Let’s do a quick recap of the key takeaways:
- It is essential to understand the WHY of the literature review before you read or write anything. Make sure you understand the 4 core functions of the process.
- The first step is to hunt down the relevant literature . You can do this using Google Scholar, your university database, the snowballing technique and by reviewing other dissertations and theses.
- Next, you need to log all the articles in your reference manager , build your own catalogue of literature and synthesise all the research.
- Following that, you need to develop a detailed outline of your entire chapter – the more detail the better. Don’t start writing without a clear outline (on paper, not in your head!)
- Write up your first draft in rough form – don’t aim for perfection. Remember, done beats perfect.
- Refine your second draft and get a layman’s perspective on it . Then tighten it up and submit it to your supervisor.

Psst… there’s more!
This post is an extract from our bestselling short course, Literature Review Bootcamp . If you want to work smart, you don't want to miss this .
38 Comments
Thank you very much. This page is an eye opener and easy to comprehend.
This is awesome!
I wish I come across GradCoach earlier enough.
But all the same I’ll make use of this opportunity to the fullest.
Thank you for this good job.
Keep it up!
You’re welcome, Yinka. Thank you for the kind words. All the best writing your literature review.
Thank you for a very useful literature review session. Although I am doing most of the steps…it being my first masters an Mphil is a self study and one not sure you are on the right track. I have an amazing supervisor but one also knows they are super busy. So not wanting to bother on the minutae. Thank you.
You’re most welcome, Renee. Good luck with your literature review 🙂
This has been really helpful. Will make full use of it. 🙂
Thank you Gradcoach.
Really agreed. Admirable effort
thank you for this beautiful well explained recap.
Thank you so much for your guide of video and other instructions for the dissertation writing.
It is instrumental. It encouraged me to write a dissertation now.
Thank you the video was great – from someone that knows nothing thankyou
an amazing and very constructive way of presetting a topic, very useful, thanks for the effort,
It is timely
It is very good video of guidance for writing a research proposal and a dissertation. Since I have been watching and reading instructions, I have started my research proposal to write. I appreciate to Mr Jansen hugely.
I learn a lot from your videos. Very comprehensive and detailed.
Thank you for sharing your knowledge. As a research student, you learn better with your learning tips in research
I was really stuck in reading and gathering information but after watching these things are cleared thanks, it is so helpful.
Really helpful, Thank you for the effort in showing such information
This is super helpful thank you very much.
Thank you for this whole literature writing review.You have simplified the process.
I’m so glad I found GradCoach. Excellent information, Clear explanation, and Easy to follow, Many thanks Derek!
You’re welcome, Maithe. Good luck writing your literature review 🙂
Thank you Coach, you have greatly enriched and improved my knowledge
Great piece, so enriching and it is going to help me a great lot in my project and thesis, thanks so much
This is THE BEST site for ANYONE doing a masters or doctorate! Thank you for the sound advice and templates. You rock!
Thanks, Stephanie 🙂
This is mind blowing, the detailed explanation and simplicity is perfect.
I am doing two papers on my final year thesis, and I must stay I feel very confident to face both headlong after reading this article.
thank you so much.
if anyone is to get a paper done on time and in the best way possible, GRADCOACH is certainly the go to area!
This is very good video which is well explained with detailed explanation
Thank you excellent piece of work and great mentoring
Thanks, it was useful
Thank you very much. the video and the information were very helpful.
Good morning scholar. I’m delighted coming to know you even before the commencement of my dissertation which hopefully is expected in not more than six months from now. I would love to engage my study under your guidance from the beginning to the end. I love to know how to do good job
Thank you so much Derek for such useful information on writing up a good literature review. I am at a stage where I need to start writing my one. My proposal was accepted late last year but I honestly did not know where to start
Like the name of your YouTube implies you are GRAD (great,resource person, about dissertation). In short you are smart enough in coaching research work.
This is a very well thought out webpage. Very informative and a great read.
Very timely.
I appreciate.
Very comprehensive and eye opener for me as beginner in postgraduate study. Well explained and easy to understand. Appreciate and good reference in guiding me in my research journey. Thank you
Thank you. I requested to download the free literature review template, however, your website wouldn’t allow me to complete the request or complete a download. May I request that you email me the free template? Thank you.
Submit a Comment Cancel reply
Your email address will not be published. Required fields are marked *
Save my name, email, and website in this browser for the next time I comment.
- Print Friendly
Academia.edu no longer supports Internet Explorer.
To browse Academia.edu and the wider internet faster and more securely, please take a few seconds to upgrade your browser .
Enter the email address you signed up with and we'll email you a reset link.
- We're Hiring!
- Help Center

Medical YouTube Videos and Methods of Evaluation: Literature Review

2018, JMIR medical education
Online medical education has relevance to public health literacy and physician efficacy, yet it requires a certain standard of reliability. While the internet has the potential to be a viable medical education tool, the viewer must be able to discern which information is reliable. Our aim was to perform a literature review to determine and compare the various methods used when analyzing YouTube videos for patient education efficacy, information accuracy, and quality. In November 2016, a comprehensive search within PubMed and Embase resulted in 37 included studies. The review revealed that each video evaluation study first established search terms, exclusion criteria, and methods to analyze the videos in a consistent manner. The majority of the evaluators devised a scoring system, but variations were innumerable within each study's methods. In comparing the 37 studies, we found that overall, common steps were taken to evaluate the content. However, a concrete set of methods did n...
Related Papers
International Journal of Online and Biomedical Engineering (iJOE)
Abiodun Opanuga
Luis Fernandez-Luque , Elia Gabarron
Background: Recent publications on YouTube have advocated its potential for patient education. However, a reliable description of what could be considered quality information for patient education on YouTube is missing.
Health Informatics Journal
Joel Greenstein
Juan-José Boté-Vericad
This paper is a systematised literature review of YouTube research in health with the aim of identify the different keyword search strategies, retrieval strategies and scoring systems to assess video content. A total of 176 peer-reviewed papers about video content analysis and video evaluation were extracted from the PubMed database. Concerning keyword search strategy, 16 papers (9.09 %) reported that search terms were obtained from tools like Google Trends or other sources. In just one paper, a librarian was included in the research team. Manual retrieval is a common technique, and just four studies (2.27 %) reported using a different methodology. Manual retrieval also produces YouTube algorithm dependencies and consequently obtains biased results. Most other methodologies to analyse video content are based on written medical guidelines instead of video because a standard methodology is lacking. For several reasons, reliability cannot be verified. In addition, because studies canno...
Heather Doucette
Objective To determine the potential value of YouTube videos as health decision aids for the public. Methods An integrative review was performed to explore 3 questions: 1) What is the validity of health-related YouTube videos created for the public? 2) Are YouTube videos an effective tool for supporting the public in decision making regarding the treatment, prevention, and diagnosis of disease? 3) How can health professionals ensure their videos will be readily accessible to those searching online for health-related information? Systematic searches of PubMed, CINAHL, and Web of Science were conducted. The returns were screened using inclusion and exclusion criteria and studies found were critically appraised. Results Fifty-eight studies assessed the validity of videos on given topics and 9 studies examined the effectiveness of videos in supporting decision making. These studies demonstrated that the majority of health-related YouTube videos lack validity. However, evidence-based vid...
Abdulhadi Shoufan
Background: You Tube is a valuable source of health-related educational material which can have a profound impact on people's health-related behaviors and decisions. However, YouTube contains a wide variety of unverified content that may promote unhealthy behaviors and activities. We aim in this systematic review to provide insight into the published literature concerning the quality of health information and educational videos found on YouTube.Methods: A search of peer-reviewed original articles was conducted regarding the educational value of YouTube medical videos which were published in English. We searched Google Scholar, Medline (through PubMed), EMBASE, Scopus, Direct Science, Web of Science, and ProQuest databases. A literature search was conducted between April 1 and April 31 of 2021. Based on the eligibility criteria, 202 artilces covering 30 medical categories were included in the qualitative synthesis.Results: We reviewed approximately 22,300 videos in all of the stu...
Vernon Curran
BACKGROUND Video has been a powerful teaching and learning tool in medical education, enabling knowledge, skill and attitude formation in a variety of areas and reaching learners with various learning and communication styles. The millennial generation has grown up with video at their fingertips at any time and any place, and social networking sites such as YouTube enable the sharing of video amongst a vast online community. YouTube has emerged as a growing educational resource for both learners and medical educators. However, the usefulness of YouTube in supporting teaching and learning across the continuum of medical education has not been explored in detail. Given the increasing usage of YouTube in medical education, a review of the literature on YouTube and its utilization in medical education could inform more effective adoption and usage by institutions, educators, practitioners and learners. OBJECTIVE To explore the use of YouTube across the medical education continuum. METHO...
IRAQI J MED SCI
Iraqi Medical Education
The role of online social networks in our everyday life has become crucial and undeniable. YouTube is a mainstay in online social networks. Created in 2005, YouTube is the third most visited Web site on the internet. Its educational value has been exemplified by the establishment of YouTube Education. Given the relative easiness of producing and uploading videos on YouTube and its free content, it has become a pool of a huge quantity of educational videos in different specialties uploaded by students and teachers. This paper aims to provide hints on effective usage of YouTube in medical education by evaluating an already existing video in order to recommend it to your students and by highlighting how to create and optimize your educational videos.
Medical Bulletin of Haseki
Kerem Taken
Melissa Beauchemin
Loading Preview
Sorry, preview is currently unavailable. You can download the paper by clicking the button above.
RELATED PAPERS
Journal of Medical Internet Research
Professor Samy Azer
JMIR cancer
Akram Jaffar
Interactive Journal of Medical Research
Susan Hingle
International Ophthalmology
Murat Oklar
Denise Harrison
Academic medicine : journal of the Association of American Medical Colleges
Clinical Cardiology
Rajesh Sachdeva
International Journal of Surgery: Protocols
Gideon Adegboyega
Middle black sea journal of health science
Nurse Education Today
Carol Haigh
Gland Surgery
Mahmoud Shalaby
Journal of Media & Management
Vaageessan Masilamani
behrang ghabchi
Joachim Allgaier
Konuralp Tıp Dergisi
Emre Emekli
Matthew Rutman
Reviews in Medical Virology
Abdullah Zafar
Jef Van den Eynde
Archivio Italiano di Urologia e Andrologia
Alberto Melchionna
The American Journal of Emergency Medicine
Neşe Yeniçeri
Facial Plastic Surgery
fatih savran
Journal of Korean Medical Science
Yavuzalp Solak
Journal of Community Hospital Internal Medicine Perspectives
RELATED TOPICS
- We're Hiring!
- Help Center
- Find new research papers in:
- Health Sciences
- Earth Sciences
- Cognitive Science
- Mathematics
- Computer Science
- Academia ©2024
Log in using your username and password
- Search More Search for this keyword Advanced search
- Latest content
- Current issue
- BMJ Journals
You are here
- Volume 28, Issue 6
- Rapid reviews methods series: Guidance on literature search
- Article Text
- Article info
- Citation Tools
- Rapid Responses
- Article metrics
- http://orcid.org/0000-0001-6644-9845 Irma Klerings 1 ,
- Shannon Robalino 2 ,
- http://orcid.org/0000-0003-4808-3880 Andrew Booth 3 ,
- http://orcid.org/0000-0002-2903-6870 Camila Micaela Escobar-Liquitay 4 ,
- Isolde Sommer 1 ,
- http://orcid.org/0000-0001-5531-3678 Gerald Gartlehner 1 , 5 ,
- Declan Devane 6 , 7 ,
- Siw Waffenschmidt 8
- On behalf of the Cochrane Rapid Reviews Methods Group
- 1 Department for Evidence-Based Medicine and Evaluation , University of Krems (Danube University Krems) , Krems , Niederösterreich , Austria
- 2 Center for Evidence-based Policy , Oregon Health & Science University , Portland , Oregon , USA
- 3 School of Health and Related Research (ScHARR) , The University of Sheffield , Sheffield , UK
- 4 Research Department, Associate Cochrane Centre , Instituto Universitario Escuela de Medicina del Hospital Italiano de Buenos Aires , Buenos Aires , Argentina
- 5 RTI-UNC Evidence-based Practice Center , RTI International , Research Triangle Park , North Carolina , USA
- 6 School of Nursing & Midwifery, HRB TMRN , National University of Ireland Galway , Galway , Ireland
- 7 Evidence Synthesis Ireland & Cochrane Ireland , University of Galway , Galway , Ireland
- 8 Information Management Department , Institute for Quality and Efficiency in Healthcare , Cologne , Germany
- Correspondence to Irma Klerings, Department for Evidence-based Medicine and Evaluation, Danube University Krems, Krems, Niederösterreich, Austria; irma.klerings{at}donau-uni.ac.at
This paper is part of a series of methodological guidance from the Cochrane Rapid Reviews Methods Group. Rapid reviews (RR) use modified systematic review methods to accelerate the review process while maintaining systematic, transparent and reproducible methods. In this paper, we address considerations for RR searches. We cover the main areas relevant to the search process: preparation and planning, information sources and search methods, search strategy development, quality assurance, reporting, and record management. Two options exist for abbreviating the search process: (1) reducing time spent on conducting searches and (2) reducing the size of the search result. Because screening search results is usually more resource-intensive than conducting the search, we suggest investing time upfront in planning and optimising the search to save time by reducing the literature screening workload. To achieve this goal, RR teams should work with an information specialist. They should select a small number of relevant information sources (eg, databases) and use search methods that are highly likely to identify relevant literature for their topic. Database search strategies should aim to optimise both precision and sensitivity, and quality assurance measures (peer review and validation of search strategies) should be applied to minimise errors.
- Evidence-Based Practice
- Systematic Reviews as Topic
- Information Science
Data availability statement
No data are available.
This is an open access article distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited, appropriate credit is given, any changes made indicated, and the use is non-commercial. See: http://creativecommons.org/licenses/by-nc/4.0/ .
https://doi.org/10.1136/bmjebm-2022-112079
Statistics from Altmetric.com
Request permissions.
If you wish to reuse any or all of this article please use the link below which will take you to the Copyright Clearance Center’s RightsLink service. You will be able to get a quick price and instant permission to reuse the content in many different ways.
WHAT IS ALREADY KNOWN ON THIS TOPIC
Compared with systematic reviews, rapid reviews (RR) often abbreviate or limit the literature search in some way to accelerate review production. However, RR guidance rarely specifies how to select topic-appropriate search approaches.
WHAT THIS STUDY ADDS
This paper presents an overview of considerations and recommendations for RR searching, covering the complete search process from the planning stage to record management. We also provide extensive appendices with practical examples, useful sources and a glossary of terms.
HOW THIS STUDY MIGHT AFFECT RESEARCH, PRACTICE OR POLICY
There is no one-size-fits-all solution for RR literature searching: review teams should consider what search approaches best fit their RR project.
Introduction
This paper is part of a series from the Cochrane Rapid Reviews Methods Group (RRMG) providing methodological guidance for rapid reviews (RRs). 1–3 While the RRMG’s guidance 4 5 on Cochrane RR production includes brief advice on literature searching, we aim to provide in-depth recommendations for the entire search process.
Literature searching is the foundation for all reviews; therefore, it is important to understand the goals of a specific RR. The scope of RRs varies considerably (from focused questions to overviews of broad topics). 6 As with conventional systematic reviews (SRs), there is not a one-size-fits-all approach for RR literature searches. We aim to support RR teams in choosing methods that best fit their project while understanding the limitations of modified search methods. Our recommendations derive from current systematic search guidance, evidence on modified search methods and practical experience conducting RRs.
This paper presents considerations and recommendations, described briefly in table 1 . The table also includes a comparison to the SR search process based on common recommendations. 7–10 We provide supplemental materials, including a list of additional resources, further details of our recommendations, practical examples, and a glossary (explaining the terms written in italics) in online supplemental appendices A–C .
Supplemental material
- View inline
Recommendations for rapid review literature searching
Preparation and planning
Given that the results of systematic literature searches underpin a review, planning the searches is integral to the overall RR preparation. The RR search process follows the same steps as an SR search; therefore, RR teams must be familiar with the general standards of systematic searching . Templates (see online supplemental appendix B ) and reporting guidance 11 for SR searches can also be adapted to structure the RR search process.
Developing a plan for the literature search forms part of protocol development and should involve an information specialist (eg, librarian). Information specialists can assist in refining the research question, selecting appropriate search methods and resources, designing and executing search strategies, and reporting the search methods. At minimum, specialist input should include assessing information sources and methods and providing feedback on the primary database search strategy.
Two options exist for abbreviating the search process: (1) reducing time spent on conducting searches (eg, using automation tools, reusing existing search strategies, omitting planning or quality assurance steps) and (2) reducing the size of the search result (eg, limiting the number of information sources, increasing the precision of search strategies, using study design filters). Study selection (ie, screening search results) is usually more resource-intensive than searching, 12 particularly for topics with complex or broad concepts or diffuse terminology; thus, the second option may be more efficient for the entire RR. Investing time upfront in optimising search sensitivity (ie, completeness) and precision (ie, positive predictive value) can save time in the long run by reducing the screening and selection workload.
Preliminary or scoping searches are critical to this process. They inform the choice of search methods and identify potentially relevant literature. Texts identified through preliminary searching serve as known relevant records that can be used throughout the search development process (see sections on database selection, development and validation of search strategies).
In addition to planning the search itself, the review team should factor in time for quality assurance steps (eg, search strategy peer review) and the management of search results (eg, deduplication, full-text retrieval).
Information sources and methods
To optimise the balance of search sensitivity and precision, RR teams should prioritise the most relevant information sources for the topic and the type of evidence required. These can include bibliographic databases (eg, MEDLINE/PubMed), grey literature sources and targeted supplementary search methods. Note that this approach differs from the Methodological Expectations of Cochrane Intervention Reviews Standards 9 where the same core set of information sources is required for every review and further supplemented by additional topic-specific and evidence-specific sources.
Choosing bibliographic databases
For many review topics, most evidence is found in peer-reviewed journal articles, making bibliographic databases the main resource of systematic searching. Limiting the number of databases searched can be a viable option in RRs, but it is important to prioritise topic-appropriate databases.
MEDLINE has been found to have high coverage for studies included in SRs 13 14 and is an appealing database choice because access is free via PubMed. However, coverage varies depending on topics and relevant study designs. 15 16 Additionally, even if all eligible studies for a topic were available in MEDLINE, search strategies will usually miss some eligible studies because search sensitivity is lower than database coverage. 13 17 This means searching MEDLINE alone is not a viable option, and additional information sources or search methods are required. Known relevant records can be used to help assess the coverage of selected databases (see also online supplemental appendix C ).
Further information sources and search techniques
Supplementary systematic search methods have three main goals, to identify (1) grey literature, (2) published literature not covered by the selected bibliographic databases and (3) database-covered literature that was not retrieved by the database searches.
When RRs search only a small number of databases, supplementary searches can be particularly important to pick up eligible studies not identified via database searching. While supplementary methods might increase the time spent on searching, they sometimes better optimise search sensitivity and precision, saving time in the long run. 18 Depending on the topic and relevant evidence, such methods can offer an alternative to adding additional specialised database searches. To decide if and what supplementary searches are helpful, it is important to evaluate what literature might be missed by the database searches and how this might affect the specific RR.
Study registries and other grey literature
Some studies indicate that the omission of grey literature searches rarely affects review conclusions. 17 19 However, the relevance of study registries and other grey literature sources is topic-dependent. 16 19–21 For example, randomised controlled trials (RCTs) on newly approved drugs are typically identified in ClinicalTrials.gov. 20 For rapidly evolving topics such as COVID-19, preprints are an important source. 21 For public health interventions, various types of grey literature may be important (eg, evaluations conducted by local public health agencies). 22
Further supplementary search methods
Other supplementary techniques (eg, checking reference lists, reviewing specific websites or electronic table of contents, contacting experts) may identify additional studies not retrieved by database searches. 23 One of the most common approaches involves checking reference lists of included studies and relevant reviews. This method may identify studies missed by limited database searches. 12 Another promising citation-based approach is using the ‘similar articles’ option in PubMed, although research has focused on updating existing SRs. 24 25
Considerations for RRs of RCTs
Databases and search methods to identify RCTs have been particularly well researched. 17 20 24 26 27 For this reason, it is possible to give more precise recommendations for RRs based on RCTs than for other types of review. Table 2 provides an overview of the most important considerations; additional information can be found in online supplemental appendix C .
Information sources for identification of randomised controlled trials (RCTs)
Search strategies
We define ‘search strategy’ as a Boolean search query in a specific database (eg, MEDLINE) using a specific interface (eg, Ovid). When several databases are searched, this query is usually developed in a primary database and interface (eg, Ovid MEDLINE) and translated to other databases.
Developing search strategies
Optimising search strategy precision while aiming for high sensitivity is critical in reducing the number of records retrieved. Preliminary searches provide crucial information to aid efficient search strategy development. Reviewing the abstracts and subject headings used in known relevant records will assist in identifying appropriate search terms. Text analysis tools can also be used to support this process, 28 29 for example, to develop ‘objectively derived’ search strategies. 30
Reusing or adapting complete search strategies (eg, from SRs identified by the preliminary searches) or selecting elements of search strategies for reuse can accelerate search strategy development. Additionally, validated search filters (eg, for study design) can be used to reduce the size of the search result without compromising the sensitivity of a search strategy. 31 However, quality assurance measures are necessary whether the search strategy is purpose-built, reused or adapted (see the ‘Quality assurance’ section.)
Database-specific and interface-specific functionalities can also be used to improve searches’ precision and reduce the search result’s size. Some options are: restricting to records where subject terms have been assigned as the major focus of an article (eg, major descriptors in MeSH), using proximity operators (ie, terms adjacent or within a set number of words), frequency operators (ie, terms have to appear a minimum number of times in an abstract) or restricting search terms to the article title. 32–34
Automated syntax translation can save time and reduce errors when translating a primary search strategy to different databases. 35 36 However, manual adjustments will usually be necessary.
The time taken to learn how to use supporting technologies (eg, text analysis, syntax translation) proficiently should not be underestimated. The time investment is most likely to pay off for frequent searchers. A later paper in this series will address supporting software for the entire review process.
Limits and restrictions
Limits and restrictions (eg, publication dates, language) are another way to reduce the number of records retrieved but should be tailored to the topic and applied with caution. For example, if most studies about an intervention were published 10 years ago, then an arbitrary cut-off of ‘the last 5 years’ will miss many relevant studies. 37 Similarly, limiting to ‘English only’ is acceptable for most cases, but early in the COVID-19 pandemic, a quarter of available research articles were written in Chinese. 38 Depending on the RR topic, certain document types (eg, conference abstracts, dissertations) might be excluded if not considered relevant to the research question.
Note also that preset limiting functions in search interfaces (eg, limit to humans) often rely on subject headings (eg, MeSH) alone. They will miss eligible studies that lack or have incomplete subject indexing. Using (validated) search filters 31 is preferable.
Updating existing reviews
One approach to RR production involves updating an existing SR. In this case, preliminary searches should be used to check if new evidence is available. If the review team decide to update the review, they should assess the original search methods and adapt these as necessary.
One option is to identify the minimum set of databases required to retrieve all the original included studies. 39 Any reused search strategies should be validated and peer-reviewed (see below) and optimised for precision and/or sensitivity.
Additionally, it is important to assess whether the topic terminology or the relevant databases have changed since the original SR search.
In some cases, designing a new search process may be more efficient than reproducing the original search.
Quality assurance and search strategy peer review
Errors in search strategies are common and can impact the sensitivity and comprehensiveness of the search result. 40 If an RR search uses a small number of information sources, such errors could affect the identification of relevant studies.
Validation of search strategies
The primary database search strategy should be validated using known relevant records (if available). This means testing if the primary search strategy retrieves eligible studies found through preliminary searching. If some known studies are not identified, the searcher assesses the reasons and decides if revisions are necessary. Even a precision-focused systematic search should identify the majority—we suggest at least 80%–90%—of known studies. This is based on benchmarks for sensitivity-precision-maximising search filters 41 and assumes that the set of known studies is representative of the whole of relevant studies.
Peer review of search strategies
Ideally, an information specialist should review the planned information sources and search methods and use the PRESS (Peer Review of Electronic Search Strategies) checklist 42 to assess the primary search strategy. Turnaround time has to be factored into the process from the outset (eg, waiting for feedback, revising the search strategy). PRESS recommends a maximum turnaround time of five working days for feedback, but in-house peer review often takes only a few hours.
If the overall RR time plan does not allow for a full peer review of the search strategy, a review team member with search experience should check the search strategy for spelling errors and correct use of Boolean operators (AND, OR, NOT) at a minimum.
Reporting and record management
Record management requirements of RRs are largely identical to SRs and have to be factored into the time plan. Teams should develop a data management plan and review the relevant reporting standards at the project’s outset. PRISMA-S (Preferred Reporting Items for Systematic Reviews and Meta-Analyses literature search extension) 11 is a reporting standard for SR searches that can be adapted for RRs.
Reference management software (eg, EndNote, 43 Zotero 44 ) should be used to track search results, including deduplication. Note that record management for database searches is less time-consuming than for many supplementary or grey literature searches, which often require manual entry into reference management software. 12
Additionally, software platforms for SR production (eg, Covidence, 45 EPPI-Reviewer, 46 Systematic Review Data Repository Plus 47 ) can provide a unified way to keep track of records throughout the whole review process, which can improve management and save time. These platforms and other dedicated tools (eg, SRA Deduplicator) 48 also offer automated deduplication. However, the time and cost investment necessary to appropriately use these tools have to be considered.
Decisions about search methods for an RR need to consider where time can be most usefully invested and processes accelerated. The literature search should be considered in the context of the entire review process, for example, protocol development and literature screening: Findings of preliminary searches often affect the development and refinement of the research question and the review’s eligibility criteria . In turn, they affect the number of records retrieved by the searches and therefore the time needed for literature selection.
For this reason, focusing only on reducing time spent on designing and conducting searches can be a false economy when seeking to speed up review production. While some approaches (eg, text analysis, automated syntax translation) may save time without negatively affecting search validity, others (eg, skipping quality assurance steps, using convenient information sources without considering their topic appropriateness) may harm the entire review. Information specialists can provide crucial aid concerning the appropriate design of search strategies, choice of methods and information sources.
For this reason, we consider that investing time at the outset of the review to carefully choose a small number of highly appropriate search methods and optimise search sensitivity and precision likely leads to better and more manageable results.
Ethics statements
Patient consent for publication.
Not applicable.
- Gartlehner G ,
- Nussbaumer-Streit B ,
- Nussbaumer Streit B ,
- Garritty C ,
- Tricco AC ,
- Nussbaumer-Streit B , et al
- Trivella M ,
- Hamel C , et al
- Hartling L ,
- Guise J-M ,
- Kato E , et al
- Lefebvre C ,
- Glanville J ,
- Briscoe S , et al
- Higgins JPT ,
- Lasserson T ,
- Chandler J , et al
- European network for Health Technology Assessment (EUnetHTA)
- Rethlefsen ML ,
- Kirtley S ,
- Waffenschmidt S , et al
- Klerings I , et al
- Bramer WM ,
- Giustini D ,
- Halladay CW ,
- Trikalinos TA ,
- Schmid IT , et al
- Frandsen TF ,
- Eriksen MB ,
- Hammer DMG , et al
- Klerings I ,
- Wagner G , et al
- Husk K , et al
- Featherstone R ,
- Nuspl M , et al
- Knelangen M ,
- Hausner E ,
- Metzendorf M-I , et al
- Gianola S ,
- Bargeri S , et al
- Hillier-Brown FC ,
- Moore HJ , et al
- Varley-Campbell J , et al
- Sampson M ,
- de Bruijn B ,
- Urquhart C , et al
- Fitzpatrick-Lewis D , et al
- Affengruber L ,
- Waffenschmidt S ,
- Kaiser T , et al
- The InterTASC Information Specialists’ Sub-Group
- Kleijnen J , et al
- Jacob C , et al
- Kaunelis D ,
- Mensinkai S , et al
- Mast F , et al
- Sanders S ,
- Carter M , et al
- Marshall IJ ,
- Marshall R ,
- Wallace BC , et al
- Fidahic M ,
- Runjic R , et al
- Hopewell S ,
- Salvador-Oliván JA ,
- Marco-Cuenca G ,
- Arquero-Avilés R
- Navarro-Ruan T ,
- Hobson N , et al
- McGowan J ,
- Salzwedel DM , et al
- Clarivate Analytics
- Corporation for Digital Scholarship
- Veritas Health Innovation Ltd
- Graziosi S ,
- Brunton J , et al
- Agency for Healthcare Research and Quality
- Institute for Evidence-Based Healthcare
Supplementary materials
Supplementary data.
This web only file has been produced by the BMJ Publishing Group from an electronic file supplied by the author(s) and has not been edited for content.
- Data supplement 1
Twitter @micaelaescb
Collaborators On behalf of the Cochrane Rapid Reviews Methods Group: Declan Devane, Gerald Gartlehner, Isolde Sommer.
Contributors IK, SR, AB, CME-L and SW contributed to the conceptualisation of this paper. IK, AB and CME-L wrote the first draft of the manuscript. All authors critically reviewed and revised the manuscript. IK is responsible for the overall content.
Funding The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests AB is co-convenor of the Cochrane Qualitative and Implementation Methods Group. In the last 36 months, he received royalties from Systematic Approaches To a Successful Literature Review (Sage 3rd edn), payment or honoraria form the Agency for Healthcare Research and Quality, and travel support from the WHO. DD works part time for Cochrane Ireland and Evidence Synthesis Ireland, which are funded within the University of Ireland Galway (Ireland) by the Health Research Board (HRB) and the Health and Social Care, Research and Development (HSC R&D) Division of the Public Health Agency in Northern Ireland.
Patient and public involvement Patients and/or the public were not involved in the design, or conduct, or reporting, or dissemination plans of this research.
Provenance and peer review Not commissioned; externally peer reviewed.
Supplemental material This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Linked Articles
- Research methods and reporting Rapid reviews methods series: Guidance on team considerations, study selection, data extraction and risk of bias assessment Barbara Nussbaumer-Streit Isolde Sommer Candyce Hamel Declan Devane Anna Noel-Storr Livia Puljak Marialena Trivella Gerald Gartlehner BMJ Evidence-Based Medicine 2023; 28 418-423 Published Online First: 19 Apr 2023. doi: 10.1136/bmjebm-2022-112185
- Research methods and reporting Rapid reviews methods series: Guidance on assessing the certainty of evidence Gerald Gartlehner Barbara Nussbaumer-Streit Declan Devane Leila Kahwati Meera Viswanathan Valerie J King Amir Qaseem Elie Akl Holger J Schuenemann BMJ Evidence-Based Medicine 2023; 29 50-54 Published Online First: 19 Apr 2023. doi: 10.1136/bmjebm-2022-112111
- Research methods and reporting Rapid Reviews Methods Series: Involving patient and public partners, healthcare providers and policymakers as knowledge users Chantelle Garritty Andrea C Tricco Maureen Smith Danielle Pollock Chris Kamel Valerie J King BMJ Evidence-Based Medicine 2023; 29 55-61 Published Online First: 19 Apr 2023. doi: 10.1136/bmjebm-2022-112070
Read the full text or download the PDF:
This paper is in the following e-collection/theme issue:
Published on 19.8.2024 in Vol 26 (2024)
This is a member publication of Open University
Prevalence of Health Misinformation on Social Media—Challenges and Mitigation Before, During, and Beyond the COVID-19 Pandemic: Scoping Literature Review
Authors of this article:

- Dhouha Kbaier 1 , PhD ;
- Annemarie Kane 2 , PhD ;
- Mark McJury 3 ;
- Ian Kenny 1 , PhD
1 School of Computing and Communications, The Open University, Milton Keynes, United Kingdom
2 Faculty of Arts and Social Sciences, The Open University, Milton Keynes, United Kingdom
3 School of Physical Sciences, The Open University, Milton Keynes, United Kingdom
Corresponding Author:
Dhouha Kbaier, PhD
School of Computing and Communications
The Open University
Walton Hall
Milton Keynes, MK7 6AA
United Kingdom
Email: [email protected]
Background: This scoping review accompanies our research study “The Experience of Health Professionals With Misinformation and Its Impact on Their Job Practice: Qualitative Interview Study.” It surveys online health misinformation and is intended to provide an understanding of the communication context in which health professionals must operate.
Objective: Our objective was to illustrate the impact of social media in introducing additional sources of misinformation that impact health practitioners’ ability to communicate effectively with their patients. In addition, we considered how the level of knowledge of practitioners mitigated the effect of misinformation and additional stress factors associated with dealing with outbreaks, such as the COVID-19 pandemic, that affect communication with patients.
Methods: This study used a 5-step scoping review methodology following Arksey and O’Malley’s methodology to map relevant literature published in English between January 2012 and March 2024, focusing on health misinformation on social media platforms. We defined health misinformation as a false or misleading health-related claim that is not based on valid evidence or scientific knowledge. Electronic searches were performed on PubMed, Scopus, Web of Science, and Google Scholar. We included studies on the extent and impact of health misinformation in social media, mitigation strategies, and health practitioners’ experiences of confronting health misinformation. Our independent reviewers identified relevant articles for data extraction.
Results: Our review synthesized findings from 70 sources on online health misinformation. It revealed a consensus regarding the significant problem of health misinformation disseminated on social network platforms. While users seek trustworthy sources of health information, they often lack adequate health and digital literacies, which is exacerbated by social and economic inequalities. Cultural contexts influence the reception of such misinformation, and health practitioners may be vulnerable, too. The effectiveness of online mitigation strategies like user correction and automatic detection are complicated by malicious actors and politicization. The role of health practitioners in this context is a challenging one. Although they are still best placed to combat health misinformation, this review identified stressors that create barriers to their abilities to do this well. Investment in health information management at local and global levels could enhance their capacity for effective communication with patients.
Conclusions: This scoping review underscores the significance of addressing online health misinformation, particularly in the postpandemic era. It highlights the necessity for a collaborative global interdisciplinary effort to ensure equitable access to accurate health information, thereby empowering health practitioners to effectively combat the impact of online health misinformation. Academic research will need to be disseminated into the public domain in a way that is accessible to the public. Without equipping populations with health and digital literacies, the prevalence of online health misinformation will continue to pose a threat to global public health efforts.
Introduction
The global adoption of the internet has made health information more accessible, and the development of digital technology has enabled its rapid dissemination. However, the internet has also made possible the dissemination of false and misleading health misinformation and disinformation, with negative consequences, including the potential to exacerbate health inequalities. Health practitioners have found themselves at the forefront of communicating with patients who have taken on board health misinformation in the context of its proliferation on the web. This paper (associated with the study by Ismail et al [ 1 ]) surveyed the current literature concerning online health misinformation to establish the extent and scope of the problem, with special reference to the needs of health practitioners in their efforts to mitigate its impact. Several studies have established useful definitions of the terms misinformation and disinformation and distinctions between them. Misinformation has been defined as information that is not supported by evidence and contradicts the best-supported evidence available [ 2 , 3 ]. Wang et al [ 4 ] made a further distinction between online misinformation and disinformation, in particular on social media platforms. For Wang et al [ 4 ], misinformation is information that is not known to be false and is shared without malice. By contrast, disinformation involves the knowing and sharing of false information with the purpose of causing harm. This paper follows the distinctions of Wang et al [ 4 ] to use the terms misinformation and disinformation as appropriate.
It is important to acknowledge at the outset that digital technology in health and social contexts presents both risks and opportunities for equity among different information audiences [ 5 ]. However, there has recently been a change in the reception and assessment of the role of the internet, social media in particular, among researchers, even predating the COVID-19 pandemic. In the early days of social media, researchers largely identified prosocial and altruistic uses of social media platforms such as Facebook and Twitter by the public. However, considerable disquiet about the impact of social media and its potential for the spread of “fake news” and the amplification of conspiracy theories has displaced the more positive evaluation that was apparent when social media was in its infancy [ 6 ]. In the majority of the current research, there is a view that digital technology, particularly social media, has amplified the problem of health misinformation. The risk most frequently identified, either explicitly or implicitly, is the susceptibility of ordinary users, who may be lacking sophisticated levels of health and digital literacies, to health misinformation. Further risks noted in the literature include disinformation disseminated by organized trolling networks and bots that can be hard to distinguish from human users. The recognition of these risks underpins an emerging policy discourse about the threat of health misinformation, particularly the role of social media in its spread, in which health information and misinformation has become a politicized issue. From one policy perspective, there is an assumption that social media users are vulnerable, even passive, recipients of health misinformation rather than reflective interpreters of the available information. The corollary of this is that correcting misinformation with authoritative knowledge will solve the problem. However, a survey of the literature suggested that neither assumption fully expresses the complexity of how health misinformation is disseminated, received, and used via the internet. This may be because although there is a growing body of evidence on the extent of online health misinformation, there is much less research about what users do with health misinformation, why users consume health misinformation, and why (and which) people believe health misinformation [ 7 - 9 ].
In this scoping review, we reviewed the current state of knowledge regarding the prevalence of online misinformation before and during the COVID-19 pandemic and the impact that has on users’ understanding of health information. We considered this context with special reference to patients’ understanding, health practitioners’ practice in response to that, and policy makers’ concerns. The pressures and distractions that health professionals face in attempting to mitigate the impacts of online health misinformation are discussed in relation to patients’ health and digital literacies and the politicization of health information and misinformation.
Information Sources
We conducted a comprehensive literature search to identify relevant studies that explored health misinformation on social media platforms. The search was conducted across multiple electronic databases, including PubMed, Scopus, Web of Science, and Google Scholar.
The search terms included a combination of relevant keywords and phrases, including “health misinformation,” “social media,” “online health communities,” and “COVID-19 pandemic.” The search was not limited by publication date. Detailed search strategies are provided in Multimedia Appendix 1 .
Study Selection
Our study selection process followed a scoping approach, where we aimed to identify and include studies that provided insights into the prevalence and challenges of health misinformation on social media platforms. Initially, 2 researchers independently screened titles and abstracts of the identified articles to determine their relevance. Articles that did not meet the inclusion criteria were excluded at this stage.
Inclusion Criteria
Articles were included if they discussed health misinformation on social media, addressed the challenges posed by health misinformation, or were relevant to the period before, during, and after the COVID-19 pandemic.
Any disagreements between the 2 researchers were resolved through discussion and consensus. Full-text articles were then retrieved for the remaining studies, and a further assessment of eligibility was conducted based on the same inclusion criteria.
Data Extraction
We gathered information on (1) study objectives, (2) research methods, (3) findings, and (4) key themes related to health misinformation. This process was performed independently by 2 researchers, and any discrepancies were resolved through discussion.
Data Synthesis and Analysis
We adopted a scoping review content analysis approach to analyze the data extracted from the selected articles. The analysis process involved identifying key themes and patterns related to health misinformation on social media. The content analysis allowed us to gain a deeper understanding of the challenges posed by health misinformation and the strategies for its mitigation, both before and during the COVID-19 pandemic.
Results of Search
In our article selection process ( Figure 1 ), we initiated our search by identifying a total of 4563 articles from various databases. Following the removal of duplicates, 1295 articles were excluded, leaving us with 3268 unique articles. Subsequently, these articles underwent an initial screening, which involved evaluating their abstracts and titles, resulting in the exclusion of 2635 articles that did not align with our inclusion criteria. Further scrutiny was applied during full-text screening, which was conducted on 633 articles. Among these, 563 articles were found ineligible due to reasons such as not meeting the inclusion criteria (n=378 articles), being classified as literature reviews, editorials, or letters (n=174 articles), or the full texts being inaccessible (n=11 articles). A total of 70 articles were ultimately included in this scoping review.

Characteristics of Included Documents (n=70)
The majority (65/70, 93%) of documents were published in the last 10 years and originated predominantly in North America (42/70, 60%), Europe (19/70, 27%), and Asia (11/70, 16%). The funding sources were mainly public (61/70, 87%). The documents were classified as original research papers (38/70, 54%), subjective “opinion” articles (editorials, viewpoints, commentaries, and letters to the journal; 11/70, 16%), and knowledge syntheses or reviews (9/70, 13%) which included systematic reviews (n=6), descriptive reviews (n=2), and 1 integrated theoretic review.
Extent and Impact of Health Misinformation Disseminated Across a Range of Outlets
This section will review the literature concerning the extent and impact of the problem of health misinformation, including the spread of antivaccination discourse. In a study by Wood et al [ 10 ] among health practitioners in North Carolina, 94.2% of the respondents reported encounters with patient health misinformation within the previous year. While the sources of this misinformation were not broken down and identified by Wood et al [ 10 ], several other studies linked patient health misinformation to the prevalence of health misinformation on social media sites, identifying the latter as a significant problem [ 4 , 11 - 15 ]. There is a growing consensus among researchers, health professionals, and policy makers about the need to confront, challenge, and even prevent the online dissemination of health misinformation [ 16 ]. Since the emergence of online social networks, users have increasingly sought and shared health information on social media sites. It is estimated that around 70% of adult internet users search health matters on the web. With the emergence of social media platforms, there has been a rise in “peer-to-peer health care,” through which individuals seek and share health information, forming online health communities with others who have similar health concerns [ 3 ]. In addition, health organizations and health professionals are increasingly using social media to disseminate and promote health information and advice. The opportunities for sharing and promoting good health information via the internet are evident, and it is important to acknowledge that in online health communities, users share experiences and receive and give different kinds of support, including emotional support, to cope with specific health conditions. However, the medium has also enabled the dissemination of health misinformation, and the prosocial aspects of sharing are also likely to involve the sharing of misinformation, putting the health of users at risk [ 3 ].
Misinformation Spreads on Social Media
There is a high degree of consensus among researchers that mainly because of the increasing popularity of social media, the internet has become a space for the dissemination and amplification of “fake news,” misleading information, and rumor, including health misinformation and antivaccine conspiracy theories [ 17 ]. The COVID-19 pandemic has heightened these concerns, resulting in a proliferation of recent studies and rapid reviews focusing on the online spread of misinformation. Lee et al [ 18 ] proposed that the proliferation of health misinformation during the COVID-19 pandemic became a major public health issue. At the earliest signs of the emerging COVID-19 pandemic, the director-general of the World Health Organization, Tedros Adhanom Ghebreyesus, speaking at the February 2020 Munich Security Conference, expressed concern about the risk of an infodemic of health misinformation disseminated via social media, identifying “vaccine hesitancy” as 1 of the top 10 global health threats [ 19 ]. Bapaye and Bapaye [ 20 ] agreed that the risks of misinformation on social networking sites constitute a global issue, referring specifically to the COVID-19 infodemic.
However, this is not in itself a new problem; longstanding concerns about “fake news” and misinformation in traditional media have been evident since the early decades of the 20th century [ 21 ], and the prevalence of misinformation on internet platforms certainly predates the COVID-19 pandemic. Therefore, because the COVID-19 pandemic has only intensified the concern regarding health misinformation, it might be more appropriate to see the pandemic as symptomatic of, and crystallizing, the challenges of countering health misinformation in the digital age, as the development of digital technology and the internet have brought about profound changes in the capacity of both misinformation and disinformation to spread globally and amplify rapidly [ 4 ].
Suarez-Lledo and Alvarez-Galvez [ 16 ] undertook a review of 69 studies of health misinformation on social media to identify the main health misinformation topics and their frequency on different social media platforms. The studies surveyed used a variety of research methods, including social network analysis (28%), evaluation of content (26%), evaluation of quality (24%), content/text analysis (16%), and sentiment analysis (6%). Suarez-Lledo and Alvarez-Galvez [ 16 ] concluded that the incidence of health misinformation was highest on Twitter, in particular, regarding the use of tobacco and other drugs, with some studies citing 87% of such posts containing misinformation. However, health misinformation about vaccines was also prevalent, with around 43% of posts containing misinformation, with the human papillomavirus vaccine being the most affected. This review by Suarez-Lledo and Alvarez-Galvez [ 16 ] confirmed many of the findings from earlier surveys. For example, in their survey of 57 articles, Wang et al [ 4 ] found that the most frequently discussed topics were regarding vaccination and infectious diseases, including Ebola and the Zika virus. Other topics such as nutrition, cancer, water fluoridation, and smoking were also prevalent. The studies they surveyed had tended to find that a high degree of misinformation on these topics was being shared and liked on social media.
Lee et al [ 18 ] conducted a cross-sectional online survey in South Korea to examine the prevalence of COVID-19 misinformation and the impact of exposure to COVID-19 misinformation on beliefs and behaviors. They found that exposure to COVID-19 misinformation was associated with misinformation belief, which then resulted in fewer preventive behaviors. Therefore, they highlighted the potential of misinformation to undermine global efforts in disease control and argued that public health strategies are needed to combat the proliferation of misinformation. Bapaye and Bapaye [ 20 ] conducted a cross-sectional online questionnaire survey of 1137 WhatsApp users in India. They noted that most research on the prevalence of misinformation in social media has focused on Twitter and Facebook and on the Global North. Measured by age, researchers found that users aged >65 years were the most vulnerable to accepting the veracity of messages containing health misinformation (K=0.38, 95% CI 0.341-0.419) Respondents aged 19 to 25 years displayed much lower vulnerability (K=0.31, 95% CI 0.301-0.319) than those aged >25 years ( P <.05). Measured by occupational category, users employed in nonprofessional occupations had the highest vulnerability (K=0.38, 95% CI 0.356-0.404); this was significantly higher than those of professionals and students ( P <.05). Notably, the vulnerability of health professionals was not significantly different from those of other occupation groups ( P >.05).
The authors concluded that in a developing country, WhatsApp users aged >65 years and those involved in nonprofessional occupations are the most vulnerable to false information disseminated via WhatsApp. Crucially, they noted that health care workers, who might be expected by laypersons to have expert knowledge, were as likely to be vulnerable to health misinformation as other occupation groups.
Antivaxxer Spread Before, During, and Beyond the COVID-19 Pandemic
Much of the current unease from researchers, understandably, centers on health misinformation about vaccines in the wake of the COVID-19 pandemic. In particular, there is concern about the growth and spread of so-called antivaxxer misinformation and beliefs. In 2019, the United States had its biggest measles outbreak in 30 years, with most cases involving people who had not been vaccinated. Hotez [ 22 ] claimed that much of the reason for the growth of antivaccine beliefs is because of a campaign of misinformation. He argued that social media sites are meeting places for the sharing of antivaccine views. To evade social media platforms’ automated moderation tools, which tend to focus on words, several antivaxxer groups, including one with around 250,000 members, began using visual codes, such as the carrot emoji, to hide antivaxxer content.
However, some of the misinformation has gained credibility because it has come from sources that laypersons would expect to be trustworthy. For example, in 1998, the British medical journal The Lancet published a paper by Dr Andrew Wakefield claiming a link between the measles, mumps, rubella vaccine and the onset of autism spectrum disorder. Wakefield’s paper was later rebutted, and an overwhelming body of evidence now refutes its conclusions [ 23 ]. However, despite long being discredited, Wakefield’s claims have remained a part of the antivaccine discourse. The persistence of the antivaccination narrative demonstrates the power of such discourses even in the face of evidence to challenge them.
Although strong antivaccine beliefs, and the more ambivalent attitude of vaccine hesitancy, have been around as long as there have been vaccines, until recent decades, they were on the margins. However, evidence supports the claim that they have been gaining momentum in the United States and Europe.
A survey by Skafle et al [ 24 ] aimed to synthesize the results from 19 studies in which the effect of social media misinformation on vaccine hesitancy was measured or discussed. The authors noted that the “vast majority” of studies were from industrialized Western countries. Only 1 study contained misinformation about autism as a side effect of COVID-19 vaccines. Nevertheless, the studies implied that information spread on social media had a negative effect on vaccine hesitancy and uptake. The conclusions from Skafle et al [ 24 ] were supported by data from online polling agencies. For example, a US YouGov poll from May 2020 found that only 55% of respondents would definitely take a COVID-19 vaccine if one were to become available, whereas 19% of respondents said that they would refuse and 26% were still undecided [ 25 ].
While much of the research about online vaccine discourse comes from the United States, there is also evidence that vaccine hesitancy has risen elsewhere. For example, in an Ipsos-MORI survey taken in December 2020, only 40% of respondents in France said they would take a COVID-19 vaccine, a figure symptomatic of a steep and swift decline in vaccine confidence in France [ 26 ]. However, interestingly, the same Ipsos-MORI poll indicated a rise in vaccine confidence among respondents in the United States since the earlier YouGov poll, cited earlier, by approximately 10% to 65%, and respondents in the United Kingdom expressed a still higher willingness to take a COVID-19 vaccine at approximately 77%. It is notable that in the United States and United Kingdom, the Ipsos-MORI results came after a period of intermittent lockdowns. The contrast with the results from France is, nevertheless, striking.
Understanding the Challenges Surrounding Health Misinformation
Here, we consider the challenges created by health misinformation on the web: (1) the role played by malicious actors on social media in spreading vaccine disinformation and misinformation and (2) how contextual and cultural issues have different effects on patients’ understanding of what is considered genuine, valid, and authentic health information.
Spread of Health Misinformation on Social Media by Malicious Actors
One strand of research presents the issue of health misinformation as a contest between trolls and bots on the one hand and the voices of trustworthy public health agencies on the other [ 6 ]. This view was supported by Hotez [ 22 ] and Broniatowski et al [ 11 ]. The latter investigated the role of bots and trolls as malicious actors mobilizing vaccination discourse on the web. Their study focused specifically on vaccine-related health messaging on Twitter. Comparing the rates of vaccine-related messages, they found that sophisticated bots and Russian trolls tweeted at higher rates than “average users.” However, the respective content from bots and trolls differed. Whereas bots communicated antivaccine messages, Russian troll accounts provided a seemingly balanced discussion of both provaccination and antivaccination arguments, implying an equivalence between them. The authors argued that amplifying and normalizing a debate is done with the purpose of sowing discord and may lead to undermining public confidence in scientific consensus about the effectiveness of vaccines. Wang et al [ 4 ] acknowledged that it is a challenge to readily distinguish between misinformation and disinformation on the web. They noted that disinformation, such as antivaccine propaganda, can unknowingly be spread by users with genuine concerns [ 4 ], as individuals increasingly seek health and healthy lifestyle information via the internet.
Contextual Factors Influencing the Reception of and Responses to Misinformation: Politicization of the Problem of Health Misinformation
The identification of online trolls, bots, and orchestrated networks as major contributors to the spread of health disinformation and misinformation is now part of mainstream political discourse in the United States. On July 16, 2021, a quarrel broke out between the president of the United States, Joe Biden, and Facebook over the spread of health misinformation on the company’s social media platforms. Speaking to journalists, Biden blamed social media companies for a rise in the number of deaths from COVID-19 among the unvaccinated in the United States. Referring explicitly to Facebook, the president claimed that by allowing the proliferation of health misinformation on its platforms, the company was “killing people” [ 27 ]. Discursive interventions from politicians are never neutral; nevertheless, Biden’s claim about the impact of health misinformation on social media is backed up by many of the studies surveyed for this paper. Facebook immediately rebutted Biden’s accusation by citing their rules, introduced in February 2021, which banned posts that make identifiably false claims about vaccines. Furthermore, Facebook challenged Biden’s claim by asserting that not only has Facebook provided more authoritative information about COVID-19 and vaccines than any other internet site, reaching 2 billion people with such posts, but also that the platform’s vaccine finder tool had been used by more than 3 million Americans.
These figures suggest that although antivaxxer groups find ways to evade detection, their reach may be countered by that of information grounded in current science. A spokesperson for the company said that, far from killing people, “The facts show that Facebook is helping save lives. Period” [ 27 ]. The argument between Biden and Facebook may indeed signal more lay awareness of the problem and echo the concerns of the recent academic research about the dissemination of health misinformation by organized bot and troll networks. Framed as it is, in terms of apportioning the blame for the spread of health misinformation, Biden’s intervention mirrors much of the academic discourse in the United States on the subject. However, it is also symptomatic of the politicization of health misinformation, arguably accelerated by the COVID-19 pandemic, which may thwart evidence-based decision-making. This point was emphasized strongly by Kyabaggu et al [ 5 ]. They framed the problem of pervasive misinformation and disinformation in terms of prime movers and beneficiaries who use it to advance sociopolitical agendas and entrench asymmetrical power, especially in times of uncertainty and threat, such as the COVID-19 pandemic.
Kyabaggu et al [ 5 ] identified government failures to adopt evidence-informed decision-making. They noted that such failures have costs that not only are economic but, crucially, result in poorer health outcomes. They cited as an example the United Kingdom government’s initial prevaccine herd immunity strategy. The intention of this strategy was to allow SARS-CoV-2 to indiscriminately spread to a critical mass to build up population immunity. The authors noted that this was “a particularly concerning example of evidence framing by a government.” Kyabaggu et al [ 5 ] argued that public acceptance of health risk messages and adoption of health-protecting behaviors is highly contingent on the degree to which governments engage in evidence-informed decision-making and communicate this basis effectively. The authors cited several instances of government actors failing to recognize misinformation, disseminating inconsistent or inaccurate information, and not using evidence- and information-based decision-making processes. In recent years, the public policy discourse in the United Kingdom has been veering away from evidence- and information-based decision-making, as politicians have denounced “experts” and their “influence” on policy [ 28 , 29 ].
Finally, Gruzd et al [ 30 ] reported on the impact of coordinated link-sharing behavior to spread and amplify conspiracy-related misinformation. They found a coalition of Facebook accounts that engaged in coordinated link sharing behavior to promote COVID-19 related misinformation. This coalition included US-based pro-Trump, QAnon, and antivaccination accounts.
Contextual Factors Influencing the Reception of and Responses to Misinformation: Health Literacies and Inequality
While the approach of Broniatowski et al [ 11 ], for example, provided a persuasive account of ways in which online health misinformation can be disseminated, there are limitations to this approach, as it did not provide an account of how users respond to the misinformation they encounter. The responses of ordinary users were assumed rather than investigated. Research by Vosoughi et al [ 31 ] provided a caveat to the claim that it is bots that accelerate the spread of misinformation. Their work supported that of Broniatowski et al [ 11 ] in suggesting that bots spread accurate and false information at the same rate. However, Vosoughi et al [ 31 ] also explained that misinformation spreads more rapidly than accurate information because humans, rather than bots, are more likely to spread misinformation [ 31 ]. This claim was further supported by Wang [ 32 ], who suggested that in democracies, where ideas compete for attention in a marketplace, accurate scientific information, which, for the layperson, may be boring or difficult to understand, is easily crowded out by information that is more easily grasped or sensational. Mokhtari and Mirzaei [ 12 ] located this problem specifically in the context of the COVID-19 pandemic. They considered that high mortality from COVID-19, its complexity, and its unknown features resulted in fear, anxiety, and mental pressure among people worldwide. To allay anxiety, people needed health information literacy, defined by the American Library Association as a set of abilities individuals require to recognize when information is needed and to locate, evaluate, and use it effectively [ 33 ]. In addition, Wang [ 32 ] noted that individuals are differentially vulnerable to health misinformation depending on their level of health literacy and that models need to account for this. Mokhtari and Mirzaei [ 12 ] argued that not only information and health literacies but also media literacy are needed. However, studies in the field of health literacy suggest that significant inequalities in health and digital literacies exist.
Researchers have argued that “vastly undervalued and unrecognized” health literacy ought to be considered the best “social vaccine” for preventing COVID-19 in populations [ 5 ]. However, inequalities in health literacy persist. Kyabaggu et al [ 5 ] defined health literacy as encompassing cognitive and social skills that determine individuals’ motivation and ability to access, understand, and use information, including quantitative health risk information, in ways that promote and maintain good health across the life course. They asserted that health literacy is an essential self-management skill and community resource for health, noting that health literacy is positively associated with patients’ involvement in clinical decision-making, willingness to express health concerns, and compliance with clinical guidance. However, despite research demonstrating the importance of health literacy, evidence, even from high-income countries, suggested relatively low levels of health literacy.
Kyabaggu et al [ 5 ] drew a link between health literacy and digital literacy. They suggested that the latter can be understood as health literacy in digital information and technology spaces. They argued that inequalities in health outcomes are exacerbated by a widening digital divide. While digital technology in health and social contexts presents both new risks and opportunities for equity in different information audiences, the ways in which power and privilege operated in the COVID-19 misinformation discourse have not been sufficiently examined. Although socially and economically disadvantaged groups were at a greater risk of exposure to COVID-19, their voices and experiences were often marginalized. In addition, inequalities in access to accurate information are not only related to issues of digital access and literacy but are also situational. For example, disadvantaged individuals may have fewer social connections, and low pay may necessitate longer working hours, militating against individuals having the resources of time and energy to seek out accurate health information and enhance their level of health literacy.
The experiences of specific groups may also go unreported. Quraishi [ 34 ] addressed the impact of misinformation on South Asian students—a fast-growing group in the United States, but one that often receives little media attention. Quraishi [ 34 ] concluded that there is a relationship between the COVID-19 pandemic and students’ academic performance and mental health, as well as an increase in the spread of misinformation regarding COVID-19 public safety guidelines.
Older adults can be a vulnerable group in relation to their comparatively poor digital literacy. Zhou et al [ 35 ] reported on the accuracy of older adults in judging health information credibility. They found that on average, participants only successfully judged 41.38% of health articles. Attractive headlines increased participant credibility judgments on the content, and of the articles shared with others, 62.5% contained falsehoods.
Contextual Factors Influencing the Reception of and Responses to Misinformation: Cultures and Values
Larson and Broniatowski [ 19 ] argued that developing the kinds of literacy advocated by Mokhtari and Mirzaei [ 12 ] and Tully et al [ 2 ] will not address the deep-seated problems they identified. The work by Kyabaggu et al [ 5 ] supported this, and noted that the infodemic crisis is not merely a health and digital literacy issue. Some demographics may be more vulnerable to persuasive communication from broader sociocultural forces. Kyabaggu et al [ 5 ] argued that in considering the social determinants of health, attention must be paid not only to digital and health literacies but also to the ways in which these literacies coexist and interact with other influences. Larson and Broniatowski [ 19 ] suggested that one of the strongest determinants of vaccine confidence or vaccine hesitancy is the level of trust or distrust in the institutions that produce vaccines. A higher level of trust encourages the willingness to accept a high level of risk for a greater benefit. A lower level of trust militates against the acceptance of even a low level of perceived risk. For Larson and Broniatowski [ 19 ], it is not simply the presence of misinformation on social media networks but the social and cultural context of users’ reception of that information that influences responses. Health information operates in a complex and contentious social world. Individuals and communities respond to new information in terms of already developed political, cultural, and social values that influence whether they trust or distrust authority. Populations may be characterized by trust or mistrust of scientific institutions and government. Trust has been eroded through the exposure of fraud, research scandals, and misconduct by major multinational pharmaceutical companies, for example. Communities may be predisposed to distrust the government and its agents depending on their own status or identity. According to Goldenberg [ 36 ], these contexts can make misinformation and health conspiracy theories compelling.
Strategies to Correct Online Misinformation
We address the additional pressures on health professionals in communicating accurate information to mitigate the effects of misinformation, particularly with regard to the additional requirements imposed as a result of the precautions being taken during the pandemic. One area of disagreement in the literature concerns the usefulness of user correction response.
Research Into User Correction Strategies
There is some disagreement as to whether engagement with misinformation by users spreads and reinforces it or even whether extended debates over health misinformation cause users to doubt the possibility of knowable facts. For example, Broniatowski et al [ 11 ] argued that when ordinary users directly confront vaccine-skeptic messages from bots, it only serves to legitimize the “debate.” By contrast, Tully et al [ 2 ] argued that social media users have a role to play in either spreading or stopping the spread of misinformation across platforms. Their research aimed to uncover what factors influenced users’ responses. Tully et al [ 2 ] acknowledged that a range of factors can influence the spread or prevention of misinformation, including the behavior of malicious actors such as bots and trolls; the platform’s terms of service; and content moderation policies. As already noted, while most users are not creators of misinformation, they may spread and amplify it by liking, sharing, or replying. In opposition to the work of Broniatowski et al [ 11 ], Tully et al [ 2 ] argued that the content of engagement is particularly important, as their research suggested that multiple corrections by social media users may be required to reduce misperceptions. However, they claimed that most people simply ignore misinformation when they see it on social media.
Tully et al [ 2 ] noted the promise in mobilizing users to engage in such correction, given the vast numbers of users on these sites, in comparison with professional fact-checkers and health authorities.
They considered whether the tone of a correction would influence perceptions of the credibility of the message. However, despite some mixed evidence, they concluded that overall, the tone was not a significant factor and that neutral, affirmative, and uncivil corrections were all effective at reducing misperceptions. They found that participants were generally unlikely to reply to the misinformation tweet. However, their content analysis of hypothetical replies suggested that when users did reply, they mainly provided correct information, particularly after seeing other corrections. Tully et al [ 2 ] concluded that user corrections offer “untapped potential” in responding to misinformation on social media, but further work is needed to consider how users can be mobilized to provide corrections, given their overall unwillingness to reply. However, a limitation of the experimental approach of Tully et al [ 2 ], acknowledged by the researchers, is that in asking individuals what they would hypothetically do, this may not reflect what they actually do in a real social media setting, especially in relation to an issue they care more strongly about. Although the experiment gauged attitudes, it did not delve into how strongly these attitudes were held. It is also not clear to what degree corrections were effective at reducing misperceptions and how reductions were measured.
By contrast, the results of experimental studies by Ittefaq [ 37 ] and Mourali and Drake [ 38 ] suggested that correcting misinformation is by no means a straightforward proposition. They noted the previous research on rebuttal, which suggested that properly designed corrections can mitigate the effects of misinformation. However, such studies have tended to compare responses to misinformation followed by correction with responses of a control group that receives no correction or receives an alternative correction. Mourali and Drake [ 38 ] argued that this static approach misses the dynamic nature of social media debate. They noted that the correction of misinformation is generally followed up with a rebuke by the original poster, inciting further correction and prolonged back-and-forth debate. Mourali and Drake [ 38 ] cited previous studies showing that exposure to conflicting information about health topics, including mammography, nutrition, and the human papillomavirus vaccine, may increase confusion and negative attitudes toward that particular health topic. The researchers found that initial exposure to misinformation had a negative impact on attitudes and intentions toward masking, consistent with previous studies that concluded that exposure to misinformation negatively impacts attitudes and intentions toward behaviors favored by science. Also consistent with previous research, they found that the first correction of the false claim improved attitudes and intentions toward masking. The authors suggested that this effect is partially explained by a decrease in the perceived strength of the argument underlying the false claim. However, this initial improvement diminished on further exposure to false claims and refutation attempts. This finding confirmed their hypothesis that extended exposure to false claims and refutation attempts appears to weaken belief in the possibility of objective knowledge, leading to less positive reactions toward masking as a science-based behavior. They concluded that the level of exposure to contradictory information needs to reach a certain threshold before it affects perceived truth objectivity. However, although people are more likely to share misinformation when its content is consistent with their existing beliefs or when its message is simple, direct, or sensational, correcting misinformation does reduce its likelihood of being shared on social media, an effect that persists even after multiple exposures.
Mourali and Drake [ 38 ] noted that each social media platform exhibits particular interaction norms, which may impact how users interpret the conversation. As their study was limited to a single platform, Reddit, and the debate was restricted to 4 exchanges between only 2 protagonists, the researchers acknowledged that these aspects limit the generalizability of the results. They suggested that future research could attempt to replicate their findings on different social media platforms, and to include more than 2 protagonists and more than 4 exchanges. They noted further that although extended debates are common on social media, it is not known how frequently they occur, echoing the comments by Suarez-Lledo and Alvarez-Galvez [ 16 ] that the extent of misinformation is not clear.
In contrast to the fairly sanguine view of Tully et al [ 2 ] about the potential of users to spread corrective information, Mourali and Drake [ 38 ] problematized the position, pointing to the potential for more complex and uncertain outcomes, whereas Larson and Broniatowski [ 19 ] argued that although the importance of correcting misinformation, item by item, should not be diminished, only if underlying issues driving misinformation are addressed can, for example, long-term vaccine confidence in populations be sustained. They argue that simply responding to misinformation with factual corrections is not likely to reverse the dissent that has been evident among antivaxxers or to necessarily persuade the more ambivalent vaccine-hesitant individuals. They identified deeper social and cultural issues at play, which have been discussed in this paper in the previous sections.

Research Into Effective Models to Accomplish the Automatic Detection of Health Misinformation in Online Health Communities
Here, we consider examples of research into the automatic detection of health misinformation in online health communities. Zhao et al [ 3 ] began from the premise that there is a vast amount of health misinformation, creating a challenge for health communities in identifying misinformation. Rather than relying on users’ ability to correct misinformation, they proposed that there is a need for an effective model to achieve automatic detection of health misinformation in online health communities. This view was also put forward by Weinzierl and Harabagiu [ 39 ]. Focusing specifically on COVID-19 vaccine misinformation, they argued that automatic detection of misinformation on social media is an essential first step in delivering interventions designed to address vaccine hesitancy.
Zhao et al [ 3 ] identified much of the existing analysis as concentrating on the linguistic features of communications only. They wanted to examine the underresearched area of whether integrating user behavioral features with linguistic features, sentiment features, and topic features could effectively distinguish misinformation from accurate information in online health communities. Their study combined the aforementioned features to build a detection model targeting misinformation in online health communities’ contexts. The behavioral features targeted were discussion initiation, interaction engagement, influential scope, relational mediation, and informational independence. Descriptions of these behavioral features are reproduced in Table 1 .
| Behavioral feature | Measurement | Description |
| Discussion initiation | The number of threads a user created | To reflect the activity of a user in terms of initiating new discussions |
| Interaction engagement | The number of replies and the number of replies to a reply a user created | To reflect the activity of a user in terms of interacting with other users |
| Influential scope | Degree centrality | To reflect the potential communication ability of a user |
| Relational mediation | Betweenness centrality | To assess the potential of a user for the control of communication in the community |
| Informational independence | Closeness centrality | To assess the ability of a user to instantly communicate with others without going through many intermediaries |
The authors tested their detection model on a data set collected from a real online health community, selecting as their data source Zibizheng Ba, an autism forum on the Baidu Tieba online health community site hosted by the Chinese web service Baidu. Baidu Tieba claims to be one of the largest interest-based discussion platforms in China. Users can generate topic-based discussion forums on the platform, share information, and make friends with other users. Posts on Baidu Tieba are indexed by Baidu, China’s most popular search engine, so users can readily find misinformation when searching for health-related information through the search engine. The authors developed a python-based web crawler to collect data from the forum. To train the health misinformation detection model, 5000 records were sampled from the whole data set by stratification according to 3 types of records (ie, thread, reply, and reply to reply) using stratified sampling methods. Therefore, the constituent types of the records (ie, thread, reply, and reply to reply) in the sample data set were consistent with the composition of the whole data set.
The researchers applied the elaboration likelihood model (ELM). The model, originally developed by Petty and Cacioppo [ 40 ] to explain attitude change, has been used extensively in advertising to try to influence consumers.
Overall, 4 types of misinformation were identified through their coding analysis, and the model correctly detected about 85% of the health misinformation. Their results also indicated that behavioral features were more informative than linguistic features in detecting misinformation. The authors concluded that their results not only demonstrated the efficacy of behavioral features in health misinformation detection but also offered both methodological and theoretical contributions to misinformation detection by integrating the features of messages as well as the features of message creators. Others have also highlighted the problems posed by misleading visual information [ 41 ].
It is worth noting that during the pandemic, the UK National Health Service (NHS) began using Twitter to promote provaccine messaging, which closely follows a combination of the features suggested by Zhao et al [ 3 ]. When users searched for the term “vaccine” or related terms, the top post was a message prominently displaying the NHS logo, identifying it as reputable and trustworthy. The tweets contained links to NHS websites providing information about vaccines and COVID-19. The posts differed in linguistic content and visual design. For example, one featured only written text on a white background and stated in bold, “Know the facts.” Another featured a large image of a happy minority ethnic family, washing dishes together, with the message that the COVID-19 vaccine decreases household transmission by up to half. The contrasting designs suggest that the message was targeted specifically to users’ timelines. It was also apparent that elements of ELM were being applied, combining the features identified by Zhao et al [ 3 ] in different ways.
Weinzierl and Harabagiu [ 39 ] adopted a different method than Zhao et al [ 3 ], reversing the more commonly used classification approach. The authors of each study claimed strong results in identifying health misinformation on social media platforms. However, Nabożny et al [ 42 ] argued that the current automatic systems for assessing the credibility of health information are not sufficiently precise to be used without supervision by human medical expert annotators.
Barve and Saini [ 43 ] have reported on their use of automated fact-checking using a coded content similarity measure (CSM). In this approach, the CSM showed improved accuracy (91.06%) compared to the accuracy of the Jaccard similarity measure (74.26%). Further, the algorithmic approach outperformed the feature-based method.
Neither Zhao et al [ 3 ] nor Weinzierl and Harabagiu [ 39 ] recorded what happens when misinformation is detected. Research from Broniatowksi et al [ 44 ] suggested that once detected, steps taken by social media platforms such as content removal or deplatforming may not be effective in stemming the spread of misinformation and may even be counterproductive. Social media platforms use a combination of “hard” and “soft” content remedies to reduce the spread of health misinformation. Soft remedies include warning labels attached to content and downranking of some content in web searches, whereas hard remedies include content removal and deplatforming of accounts. Hard remedies are controversial and have given rise to accusations of censorship. For the authors, short-term evidence for the effectiveness of hard remedies is in any case mixed, and long-term evidence is yet to be examined. Their study focused on Facebook and found that while hard remedies did reduce the number of antivaccine posts, they also produced unintended consequences. Provaccine content was removed, and engagement with the remaining antivaccine content repeatedly recovered to prepolicy levels. Worryingly, this content became more misinformative, more politically polarized, and more likely to be seen in users’ news feeds. The authors explain these results as a product of Facebook’s architecture, which is designed to promote community formation. Members of communities dedicated to vaccine refusal seek out misinformation. To meet this demand, and to circumvent content moderation efforts, antivaccine content producers post links to external sources of misinformative content, such as Bitchute, Rumble, Gab, and Telegram, in lieu of more mainstream platforms that had implemented similar content removal policies (eg, YouTube and Twitter). Broniatowski et al [ 44 ] argued that Facebook’s policy reduced the number of posts in antivaccine venues but was not successful in inducing a sustained reduction in engagement with antivaccine content, including misinformation. The authors noted that alternative platforms often host politically extreme right-wing content. Therefore, they argued that Facebook’s content removal policies may have the unintended consequence of radicalizing their audiences, and their findings suggested the need to address how social media platform architecture enables community formation and mobilization around misinformative topics when managing the spread of online content.
These studies advocate for the automatic detection of health misinformation. However, work that calls into question the ability of automatic detection to operate without human intervention has also been discussed. In addition, there are questions raised in the literature about what should be done when misinformation is detected and concerns about whether content removal or deplatforming of accounts are the most effective ways to reduce the spread of health misinformation or may even be counterproductive.
The Roles of Health Practitioners
The discussion so far has highlighted the complex and multifaceted dimensions of the context of online health misinformation in which health practitioners must operate. As noted in our introduction, a study of health practitioners in North Carolina found that nearly 95% had encountered patient health misinformation within the previous year [ 10 ]. There is very little research on the amount or effectiveness of training received by health professionals to prepare them for engaging with patients about health misinformation. Wood et al [ 10 ] found that most respondents had not received relevant training despite overwhelmingly reporting encountering health misinformation.
Nevertheless, within the literature, there is no shortage of advice from researchers and health professionals addressed to health practitioners on how to approach and correct health misinformation. This advice stems from both original research studies and reviews of best practices featured in peer-reviewed medical and health journals. Such advice centers on the need for health practitioners to understand misinformation and how to address it. Health practitioners are advised of the need to be aware of health myths and urged to dismantle them in providing accurate health guidance [ 45 , 46 ]. Practitioners are further advised that misinformation and pseudoscience are appealing to those seeking certainty because they present information in absolutes, whereas medical science is often ambiguous and contingent. Health practitioners are also encouraged to learn how to message more clearly and to mimic the strategies of misinformation [ 45 ]. One study recommends that “practitioners familiarize themselves with the tools of scientific enquiry and consider the pros and cons of various conspiracy evaluation guidelines” [ 47 ]. Thompson [ 48 ] reports on the activity of health professional influencers and pedagogues in combating misinformation. However, the effectiveness of such social media influencers who are also health professionals remains unclear. At the same time, there is some acknowledgment in this body of literature that misinformation cannot simply be offset with facts, confirming the challenges, discussed earlier, of simply engaging in online refutation. Addressing misinformation also depends on meeting patients’ emotional needs [ 45 , 49 ].
In this context, the one-to-one patient-provider relationship in the practice setting is perceived as paramount [ 45 ]. As suggested by much of the research, source credibility, or trust, is understood to be the strongest driver of effective correction strategies [ 50 ]. It is argued that health care practitioners have the unique opportunity to guide patients toward high-quality, evidence-based medical information [ 10 ]. However, it is also noted that practitioners will need patience in their efforts to persuade patients to abandon strongly held self-beliefs, however harmful. Doing so may mean patients relinquishing membership of online communities that have become integral in their lives and even their identities. As noted earlier, belief in misinformation is often persistent in the face of evidence. Success is more likely when individuals are encouraged to reexamine their information sources, alongside new information providing additional context, rather than simply characterizing the individual’s beliefs as wrong [ 51 ]. Kyabaggu et al [ 5 ] commented that good health communication needs to be tailored to the underlying cause of the misinformation problem, and efforts should be made to take on board inequalities within populations to create accurate, low-barrier, targeted health risk messaging. Skafle et al [ 24 ] contended that to challenge misconceptions, false claims need to be openly addressed and discussed with both cultural and religious awareness in mind. Guidance for practitioners noted that while responding to patient questions about alternative or unproven therapies may become laborious, a strong bond of trust between health practitioner and patient gives a patient a feeling of being supported and increases their adherence to treatment [ 52 ]. Rather than waiting for patients to raise misinformation issues, health care practitioners are advised to anticipate and proactively address potential misinformation and myths with patients. For example, the mortality rate for pediatric cancer has risen during the COVID-19 pandemic because of delayed access to medical care, but misinformation related to COVID-19 may also be a contributing factor [ 53 ]. The literature highlights the challenge of navigating the information and misinformation and the need for health practitioners to communicate with their patients more effectively. However, such efforts are not always successful. Some of the factors that may prevent effective communication of good health information have already been raised in this paper. They are revisited and discussed in the next section, along with other stressors for health practitioners.
Stressors for Health Practitioners
Challenges for health practitioners include time pressures and the additional burdens placed on them during the COVID-19 pandemic. These additional pressures add to the issues health practitioners face in trying to mitigate the impact of misinformation. The following is a brief overview of these issues.
On the one hand, administrative burdens placed on practitioners frequently deny them time for dialogue with their patients [ 52 ]. On the other, in different contexts, practitioners may be coping with a lack of proper facilities; poor infrastructure for patient care; insufficient or ineffective personal protective equipment; lack of awareness among the general population; poor compliance with preventive methods; and the fear of being infected with the virus, as they too are exposed to misinformation. During the COVID-19 pandemic, health practitioners were considered more vulnerable than other workers to developing psychological problems and other stress-related disorders, as they treated patients confirmed with COVID-19 while also dealing with misinformation [ 54 ].
As noted above, practitioners are recommended to invest in developing high levels of patient trust and to proactively correct health misinformation. However, recommendations presuppose that health practitioners necessarily have the resources to do these things well. Some of the materials produced to educate patients are not always reliable or evidence based, resulting ultimately in a loss of trust on the part of patients [ 52 ]. In addition, as noted previously, health practitioners themselves are not necessarily immune from accepting health misinformation as credible. Evidence about the level of knowledge and understanding of COVID-19 among practitioners reveals its unevenness. A study of dentists and oral health practitioners’ knowledge about COVID-19 suggested that their knowledge was at a relatively high level [ 55 ]. By contrast, a study of 310 eye care professionals in Nepal revealed some knowledge but also some acceptance of misinformation. Symptoms of COVID-19 were known to 94% of participants, but only 49% of participants were aware of how the disease is transmitted. More significantly, 41% of participants believed that the consumption of hot drinks helps to destroy the virus, in contradiction to World Health Organization information. The mean overall “knowledge” performance score, as measured by the benchmarks set by the researchers, was 69.65% [ 56 ].
A qualitative study to investigate primary health care practitioners’ perceptions and understanding of the COVID-19 pandemic was conducted in KwaZulu-Natal, South Africa. The study collected data from 15 participants at 2 different clinics situated in rural KwaZulu-Natal. Participants comprised nurses, physiotherapists, pharmacists, community caregivers, social workers, and clinical associates. Data were collected through individual, in-depth face-to-face interviews using a semistructured interview guide. The participants reported prepandemic and pandemic experiences of fear or denial. There was a perception of poor preparation for the COVID-19 outbreak. The findings also revealed participants’ misperceptions regarding the nature of the COVID-19 pandemic. Researchers concluded that respondents’ misunderstandings regarding the pandemic were primarily a result of misinformation found on social media [ 57 ].
The discussion in this section so far has highlighted the significant potential of health practitioners in mitigating the impact of online health misinformation. However, it has also underlined factors that may militate against health practitioners’ ability to do so effectively. Not least of these is the issue of health practitioners’ own knowledge, which coexists with other stressors for health practitioners in combating misinformation. The discussion will now consider health information management (HIM) as a tool for supporting health practitioners’ knowledge base as one element in a multifaceted strategy for combating misinformation on the web.
HIM as a Mitigation Strategy
We have seen there is a need for health practitioners to be supported with evidence-based knowledge that they can share with patients. Kyabaggu et al [ 5 ] argued that the COVID-19 pandemic has demonstrated that in an infectious health crisis, the gathering of accurate and reliable data to assist with the public health response is essential. They highlighted the importance of HIM professionals in supporting contact tracing and syndromic surveillance, as well as in mapping and forecasting health data. They noted that the generation of health information supports the continuum of care and the setting of targets and indicators and aids the planning, monitoring, and evaluation of health programs locally and globally. The health information produced also underpins the development of equitable, efficient, and accessible health care systems, contributing to improving public health initiatives and outcomes. Kyabaggu et al [ 5 ] emphasized the importance of an area of HIM, currently in its early stages, that deals with gathering and identifying evidence about the structural inequalities that underlie the disparities in vulnerability to health misinformation discussed in this paper. The collection of rich, high-quality information, including patient-reported experience, outcome measures, and culturally appropriate identity data, can enable health practitioners and public health advisers serving the most disadvantaged and underrepresented communities to use more tools of advocacy for patients.
The authors noted that advances in technology, including artificial intelligence, have the potential to relieve some of the pressures and constraints on health practitioners working on the front line during crises such as the COVID-19 pandemic, allowing more time for one-to-one engagement with patients. Kyabaggu et al [ 5 ] advocated for the content expertise of health information managers to serve health practitioners by delivering patient-facing information triaging services; constructing user-friendly knowledge representations, such as data visualizations; and developing information interpretation tools, such as decision aids, plain language summaries, and supplementary explanatory information and metadata. Kyabaggu et al [ 5 ] identified the interdisciplinary underpinnings of HIM as essential in contributing to the educational, informational, and decision-making support for addressing current and future infodemic management crises.
Summary of Results
Within the literature, there is a consensus that there exists a significant problem of online health misinformation disseminated via the internet on social network platforms, often by online health communities. It is apparent that while users seek trustworthy sources of health information, they are unequally equipped to assess its credibility. This is partly because some groups lack sufficient levels of health and digital literacies, which may be exacerbated by concomitant social and economic inequalities. Reception of, and response to, online health misinformation is also shaped by users’ cultural contexts, values, and experiences, which may hinder trust in scientific institutions and governments. Evidence suggests that some demographics are more vulnerable to accepting health misinformation as credible and that health practitioners are unevenly prepared in the context of new global health crises, such as the COVID-19 pandemic. Furthermore, the evidence of disparities in positive and negative attitudes toward vaccination highlights a need to pay specific attention to regional and national settings, even in the current global context. Preexisting levels of local trust in vaccine providers may be a significant factor to consider. While the validity and reliability of YouGov polls are limited, nevertheless, the data from an admittedly narrow range of sources suggests that vaccine confidence may have become more fluctuating and potentially vulnerable to destabilization in the digital era.
While online mitigation strategies such as user correction and automatic detection may have their uses, their effectiveness is contested, and some studies suggest they may even be counterproductive. Our analysis of the available literature indicates that the effectiveness of these strategies varies and needs further evaluation [ 42 , 58 ]. The issue of online health misinformation is further complicated by the operation of malicious actors and politicization of the issue, particularly during the COVID-19 pandemic, militating against the equitable and trusted dissemination of evidence-based knowledge. The role of health practitioners in this context is a challenging one. Research suggests that on the one hand, they are still best placed, at the front line of care, to combat health misinformation with science-based knowledge and advice. On the other hand, the stressors identified in this review create barriers to their abilities to do this well. Constraints of time and lack of supporting infrastructure add to the knowledge deficit noted earlier. Our review underlines the complexity of the environment in which health practitioners operate and calls for greater support and resources to enable effective mitigation of health misinformation [ 59 ]. Investment in HIM at local and global levels could address all 3 deficits, creating the potential for health practitioners to enhance their capacity to build trust via knowledgeable one-to-one communication with patients.
Limitations
The limitations of this study are the following: First, the constraints of time and space have necessarily limited the scale and scope of the survey. Second, the study of online health misinformation is a growing field, and inevitably, the nature of the issue means that new evidence is emerging at a rapid rate. In particular, new knowledge and further reflection in the wake of the COVID-19 pandemic will continue to shed new light on the subject. Our study acknowledges these limitations and emphasizes the dynamic nature of the field.
Conclusions
Our survey of the literature on online health misinformation has revealed a complex and multifaceted context in which health practitioners must operate. As the world renormalizes following the pandemic, a collaborative global interdisciplinary effort to provide equitable access to timely, accurate, and complete health information will be needed to support health practitioners in combating the impact of online health misinformation. Academic research will need to be disseminated into the public domain in a way that is accessible to the public to counter misinformation and educate populations concerning how science is carried out. Our conclusions drawn from this review stress the urgency of effective strategies and collaborative efforts to mitigate the prevalence and impact of health misinformation on a global scale. Without strategies for equipping populations with the health and digital literacies required to interpret and use information appropriately, the prevalence of online health misinformation will continue to pose a threat to global public health efforts, disproportionately affecting vulnerable and resource-limited populations. Although social media platforms have a responsibility to correct misinformation, governments will need to engage in evidence-informed decision-making and invest in HIM to support frontline health practitioners in their work, enhance population health literacy, and strengthen evidence-informed decision-making at all levels.
Several issues for further investigation arise from the findings of this review. These include the following:
- The long-term impact of COVID-19 vaccine hesitancy
- Whether the COVID-19 pandemic has intensified or diminished information literacy, and the related question of whether the pandemic will incentivize health information literacy
- The effects of social and cultural differences on the long-term traction of future health misinformation
- Whether social and economic inequalities will become less or more pronounced in the face of a global pandemic
- The comparative effectiveness of strategies to enhance populations’ media and digital literacies to facilitate the mitigation of health misinformation and its effects
- The influence of state actors on the propagation of health misinformation on the web
- The extent to which academic research has been disseminated into the public domain in a way that is accessible to the public, and the effectiveness of strategies to do so to counter misinformation and educate populations concerning how science is carried out
Acknowledgments
This research was funded by the School of Computing and Communications at the Open University. It allowed researchers across several faculties to collaborate and build a research team that focused on the experience of health practitioners with misinformation and its impact on their job practice. The authors would also like to thank Tracie Farrell and Nashwa Ismail for their invaluable suggestions and recommendations, as well as their assistance in the article screening process.
Data Availability
The data analyzed in this study are derived from published articles available on Google Scholar. All articles included in the review are cited in the reference list. No additional data or code were collected or generated as part of this study.
Authors' Contributions
The study was conceptualized by DK; funding acquisition was managed by DK; data were curated by DK, AK, MM, and IK; formal analysis was conducted by DK and MM; the investigation was carried out by AK and MM; the methodology was designed by DK and MM; project administration was overseen by DK; resources were provided by DK; supervision was carried out by DK; validation was conducted by DK, AK, MM, and IK; visualization was handled by DK and MM; writing (original draft preparation) was done by DK; and writing (review and editing) was carried out by DK, AK, and MM. All authors reviewed and approved the final version.
Conflicts of Interest
None declared.
Detailed search strategy.
- Ismail N, Kbaier D, Farrell T, Kane A. The experience of health professionals with misinformation and its impact on their job practice: qualitative interview study. JMIR Form Res. Nov 02, 2022;6(11):e38794. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Tully M, Bode L, Vraga EK. Mobilizing users: does exposure to misinformation and its correction affect users’ responses to a health misinformation post? Soc Media Soc. Dec 10, 2020;6(4):205630512097837. [ CrossRef ]
- Zhao Y, Da J, Yan J. Detecting health misinformation in online health communities: Incorporating behavioral features into machine learning based approaches. Inf Process Manage. Jan 2021;58(1):102390. [ CrossRef ]
- Wang Y, McKee M, Torbica A, Stuckler D. Systematic literature review on the spread of health-related misinformation on social media. Soc Sci Med. Nov 2019;240:112552. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Kyabaggu R, Marshall D, Ebuwei P, Ikenyei U. Health literacy, equity, and communication in the COVID-19 era of misinformation: emergence of health information professionals in infodemic management. JMIR Infodemiology. 2022;2(1):e35014. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Sutton J. Health communication trolls and bots versus public health agencies' trusted voices. Am J Public Health. Oct 2018;108(10):1281-1282. [ CrossRef ] [ Medline ]
- Kim S, Capasso A, Ali SH, Headley T, DiClemente RJ, Tozan Y. What predicts people's belief in COVID-19 misinformation? A retrospective study using a nationwide online survey among adults residing in the United States. BMC Public Health. Nov 18, 2022;22(1):2114. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Morgan JC, Cappella JN. The effect of repetition on the perceived truth of tobacco-related health misinformation among U.S. adults. J Health Commun. Mar 04, 2023;28(3):182-189. [ CrossRef ] [ Medline ]
- Nan X, Wang Y, Thier K. Why do people believe health misinformation and who is at risk? A systematic review of individual differences in susceptibility to health misinformation. Soc Sci Med. Dec 2022;314:115398. [ CrossRef ] [ Medline ]
- Wood JL, Lee GY, Stinnett SS, Southwell BG. A pilot study of medical misinformation perceptions and training among practitioners in North Carolina (USA). Inquiry. 2021;58:469580211035742. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Broniatowski DA, Jamison AM, Qi S, AlKulaib L, Chen T, Benton A, et al. Weaponized health communication: Twitter bots and Russian trolls amplify the vaccine debate. Am J Public Health. Oct 2018;108(10):1378-1384. [ CrossRef ] [ Medline ]
- Mokhtari H, Mirzaei A. The tsunami of misinformation on COVID-19 challenged the health information literacy of the general public and the readability of educational material: a commentary. Public Health. Oct 2020;187:109-110. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Schmid P, Altay S, Scherer LD. The psychological impacts and message features of health misinformation - a systematic review of randomized controlled trials. Eur Psychol. Jul 2023;28(3):162-172. [ CrossRef ]
- Southwell BG, Otero Machuca J, Cherry ST, Burnside M, Barrett NJ. Health misinformation exposure and health disparities: observations and opportunities. Annu Rev Public Health. Apr 03, 2023;44(1):113-130. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Westberry C, Palmer XL, Potter L. Social media and health misinformation: a literature review. In: Arai K, editor. Proceedings of the Future Technologies Conference (FTC) 2023, Volume 3. FTC 2023. Lecture Notes in Networks and Systems, vol 815. Cham, Switzerland. Springer; 2023.
- Suarez-Lledo V, Alvarez-Galvez J. Prevalence of health misinformation on social media: systematic review. J Med Internet Res. Jan 20, 2021;23(1):e17187. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Borges do Nascimento IJ, Pizarro AB, Almeida J, Azzopardi-Muscat N, Gonçalves MA, Björklund M, et al. Infodemics and health misinformation: a systematic review of reviews. Bull World Health Organ. Sep 01, 2022;100(9):544-561. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Lee JJ, Kang K, Wang MP, Zhao SZ, Wong JYH, O'Connor S, et al. Associations between COVID-19 misinformation exposure and belief with COVID-19 knowledge and preventive behaviors: cross-sectional online study. J Med Internet Res. Nov 13, 2020;22(11):e22205. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Larson HJ, Broniatowski DA. Why debunking misinformation is not enough to change people's minds about vaccines. Am J Public Health. Jun 2021;111(6):1058-1060. [ CrossRef ] [ Medline ]
- Bapaye JA, Bapaye HA. Demographic factors influencing the impact of coronavirus-related misinformation on WhatsApp: cross-sectional questionnaire study. JMIR Public Health Surveill. Jan 30, 2021;7(1):e19858. [ FREE Full text ] [ CrossRef ] [ Medline ]
- McKernon E. Fake news and the public. Harper's. Oct 1925. URL: https://harpers.org/archive/1925/10/fake-news-and-the-public/ [accessed 2024-07-30]
- Hotez P. The physician-scientist: defending vaccines and combating antiscience. J Clin Invest. Apr 29, 2019;129(6):2169-2171. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Dyer C. Lancet retracts Wakefield's MMR paper. BMJ. Mar 02, 2010;340:c696. [ CrossRef ] [ Medline ]
- Skafle I, Nordahl-Hansen A, Quintana DS, Wynn R, Gabarron E. Misinformation about COVID-19 vaccines on social media: rapid review. J Med Internet Res. Aug 04, 2022;24(8):e37367. [ FREE Full text ] [ CrossRef ] [ Medline ]
- New Yahoo News/YouGov coronavirus poll: almost 1 in 5 say they won't get vaccinated. Yahoo News. URL: https://www.yahoo.com/news/new-yahoo-news-you-gov-coronavirus-poll-almost-one-in-five-say-they-wont-get-vaccinated-143852222.html [accessed 2024-08-06]
- Peretti-Watel P, Verger P, Raude J, Constant A, Gautier A, Jestin C, et al. Dramatic change in public attitudes towards vaccination during the 2009 influenza A(H1N1) pandemic in France. Euro Surveill. Oct 31, 2013;18(44):20623. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Reuters. ‘They’re killing people’: Biden slams Facebook for Covid disinformation. The Guardian. Jul 21, 2021. URL: https://www.theguardian.com/media/2021/jul/17/theyre-killing-people-biden-slams-facebook-for-covid-misinformation [accessed 2024-07-30]
- Britain has had enough of experts, says Gove. Financial Times. URL: https://www.ft.com/content/3be49734-29cb-11e6-83e4-abc22d5d108c [accessed 2024-07-30]
- US news roundup: 19-25 August. Research Professional News. Aug 25, 2022. URL: https://www.researchprofessionalnews.com/rr-news-usa-2022-8-us-news-roundup-19-25-august/ [accessed 2024-07-30]
- Gruzd A, Mai P, Soares FB. How coordinated link sharing behavior and partisans' narrative framing fan the spread of COVID-19 misinformation and conspiracy theories. Soc Netw Anal Min. 2022;12(1):118. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Vosoughi S, Roy D, Aral S. The spread of true and false news online. Science. Mar 09, 2018;359(6380):1146-1151. [ CrossRef ] [ Medline ]
- Wang Y. Systematic review on the social mechanism of health misinformation dissemination in the internet era. Eur J Public Health. Nov 2018;28(suppl_4):cky213.194. [ CrossRef ]
- Framework for information literacy for higher education. American Library Association. 2016. URL: http://www.ala.org/acrl/sites/ala.org.acrl/files/content/issues/infolit/framework1.pdf [accessed 2024-07-30]
- Quraishi Z. Addressing mental health, misinformation, and religious tensions among South Asian students across California higher education during the COVID-19 pandemic: A qualitative research study. Heliyon. Jun 2023;9(6):e16396. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Zhou J, Xiang H, Xie B. Better safe than sorry: a study on older adults' credibility judgments and spreading of health misinformation. Univers Access Inf Soc. Aug 04, 2022;22(3):1-10. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Goldenberg MJ. Vaccine Hesitancy: Public Trust, Expertise, and the War on Science. Pittsburgh, PA. University of Pittsburgh Press; 2021.
- Ittefaq M. "It frustrates me beyond words that I can't fix that": health misinformation correction on Facebook during COVID-19. Health Commun. Nov 12, 2023;12:1-11. [ CrossRef ] [ Medline ]
- Mourali M, Drake C. The challenge of debunking health misinformation in dynamic social media conversations: online randomized study of public masking during COVID-19. J Med Internet Res. Mar 02, 2022;24(3):e34831. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Weinzierl MA, Harabagiu SM. Automatic detection of COVID-19 vaccine misinformation with graph link prediction. J Biomed Inform. Dec 2021;124:103955. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Petty RE, Cacioppo JT. Elaboration likelihood model of persuasion. In: Communication and Persuasion. Springer Series in Social Psychology. New York, NY. Springer; 1986.
- Cowles K, Miller R, Suppok R. When seeing isn't believing: navigating visual health misinformation through library instruction. Med Ref Serv Q. 2024;43(1):44-58. [ CrossRef ] [ Medline ]
- Nabożny A, Balcerzak B, Morzy M, Wierzbicki A, Savov P, Warpechowski K. Improving medical experts' efficiency of misinformation detection: an exploratory study. World Wide Web. 2023;26(2):773-798. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Barve Y, Saini JR. Detecting and classifying online health misinformation with 'Content Similarity Measure (CSM)' algorithm: an automated fact-checking-based approach. J Supercomput. 2023;79(8):9127-9156. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Broniatowski D, Gu J, Jamison AM, Simons JR. Facebook's architecture undermines vaccine misinformation removal efforts. arXiv. Preprint posted online Feb 4, 2022. [ FREE Full text ] [ CrossRef ]
- Russell N. Misinformation during COVID: how should nurse practitioners respond? J Nurse Pract. Jun 2021;17(6):763-764. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Wilner T, Holton A. Breast cancer prevention and treatment: misinformation on Pinterest, 2018. Am J Public Health. Oct 2020;110(S3):S300-S304. [ CrossRef ] [ Medline ]
- MacFarlane D, Hurlstone MJ, Ecker UK. Protecting consumers from fraudulent health claims: A taxonomy of psychological drivers, interventions, barriers, and treatments. Soc Sci Med. Aug 2020;259:112790. [ CrossRef ] [ Medline ]
- Thompson JD. Public health pedagogy and digital misinformation: health professional influencers and the politics of expertise. J Sociol. Sep 28, 2022;59(3):646-663. [ CrossRef ]
- Gunter J. Medical misinformation and the internet: a call to arms. Lancet. Jun 08, 2019;393(10188):2294-2295. [ CrossRef ] [ Medline ]
- Sui Y, Zhang B. Determinants of the perceived credibility of rebuttals concerning health misinformation. Int J Environ Res Public Health. Mar 02, 2021;18(3):1345. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Collier R. Containing health myths in the age of viral misinformation. CMAJ. May 14, 2018;190(19):E578. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Peterson JS, Swire-Thompson B, Johnson SB. What is the alternative? Responding strategically to cancer misinformation. Future Oncol. Sep 2020;16(25):1883-1888. [ CrossRef ] [ Medline ]
- Guidry JP, Miller CA, Ksinan AJ, Rohan JM, Winter MA, Carlyle KE, et al. COVID-19-related misinformation among parents of patients with pediatric cancer. Emerg Infect Dis. Mar 2021;27(2):650-652. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Ali S, Khalid A, Zahid E. Is COVID-19 immune to misinformation? A brief overview. Asian Bioeth Rev. Jun 2021;13(2):255-277. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Jafari A, Mohammadpour M, Ghanbarzadegan A, Rossi-Fedele G, Bastani P. Oral health practitioners' knowledge, attitude, and awareness about coronavirus: A systematic review and meta-analysis. J Educ Health Promot. 2021;10:39. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Sanyam SD, Sah SK, Chaudhary P, Burton MJ, Hoffman JJ. Knowledge and awareness-based survey of COVID-19 within the eye care profession in Nepal: Misinformation is hiding the truth. PLoS One. 2021;16(7):e0254761. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Nxumalo CT, Mchunu GG. A qualitative study to explore primary health care practitioners' perceptions and understanding regarding the COVID-19 pandemic in KwaZulu-Natal, South Africa. Afr J Prim Health Care Fam Med. Nov 26, 2021;13(1):e1-e11. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Abbasi K. Where now in the danse macabre of COVID-19 and misinformation? BMJ. Aug 17, 2023;382:1884. [ CrossRef ]
- Pesko MF, Cummings KM, Douglas CE, Foulds J, Miller T, Rigotti NA, et al. United States public health officials need to correct e-cigarette health misinformation. Addiction. May 2023;118(5):785-788. [ CrossRef ] [ Medline ]
Abbreviations
| content similarity measure |
| elaboration likelihood model |
| health information management |
| National Health Service |
Edited by G Eysenbach, T Leung; submitted 15.04.22; peer-reviewed by G Nneji, S-F Tsao; comments to author 07.06.22; revised version received 29.09.22; accepted 12.07.24; published 19.08.24.
©Dhouha Kbaier, Annemarie Kane, Mark McJury, Ian Kenny. Originally published in the Journal of Medical Internet Research (https://www.jmir.org), 19.08.2024.
This is an open-access article distributed under the terms of the Creative Commons Attribution License (https://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work, first published in the Journal of Medical Internet Research (ISSN 1438-8871), is properly cited. The complete bibliographic information, a link to the original publication on https://www.jmir.org/, as well as this copyright and license information must be included.
- Systematic Review
- Open access
- Published: 17 August 2024
Direct and indirect effects of economic sanctions on health: a systematic narrative literature review
- Vahid Yazdi-Feyzabadi 1 ,
- Atefeh Zolfagharnasab 2 ,
- Soheila Naghavi 3 ,
- Anahita Behzadi 1 ,
- Maysam Yousefi 4 &
- Mohammad Bazyar ORCID: orcid.org/0000-0003-2543-1862 5
BMC Public Health volume 24 , Article number: 2242 ( 2024 ) Cite this article
209 Accesses
1 Altmetric
Metrics details
Economic sanctions are defined as restrictions imposed by other countries against individuals, groups, or governments of other countries. These sanctions have a detrimental impact on the economies of countries and can also limit access to healthcare services for people as a secondary consequence. This study aims to systematically review the literature to examine the direct and indirect effects of economic sanctions on health through a narrative synthesis.
This systematic literature review was limited to papers published between January 1990 and July 2023. Relevant documents published in English and Persian were searched for in databases including Cochrane Library, PubMed, Embase, Scopus, Web of Science, SID, Magiran, and Irandoc. The direct and indirect effects of sanctions on health were classified using two frameworks proposed by the World Health Organization (WHO): the Health System Building Blocks and “Social Determinants of Health”.
Out of a total of 18,219 articles, 59 were selected based on inclusion criteria. The effects of sanctions were divided into direct and indirect groups. Direct effects encompassed seven main themes: access to essential medicine, medical products, vaccines and technologies; financing; health workforce; service delivery; research and health information systems; health outcomes; and financial risk protection. Indirect effects also were classified into six main themes: socioeconomic status; food and agricultural products; stress; early life conditions; high-risk behaviors and addiction; and transport. Most studies focused on the access to medicines, food, economic and social status.
Conclusions
Economic sanctions have had profoundly negative impacts on all aspects of the healthcare system. The international community must address these effects on health and take necessary measures to prevent or mitigate them, particularly in ensuring the provision of basic and essential healthcare needs for individuals and communities.
Peer Review reports
Sanctions are purposeful and determined restrictions imposed by one or more countries against another individual, group or countries’ government. Sanctions are usually imposed by international organizations as a pressure tool for responding to the course of actions of any country that opposes them [ 1 ].
Economic sanctions are the most common type of these restrictions. The two main types of these sanctions are trade and financial restrictions. Trade sanctions restrict imports to and exports from the countries under sanctions while financial sanctions are closely related to economic ones, but their focus is on banning the money flows and financial resources into or out of the country. These sanctions can include blocking government assets, restricting access to financial markets, loans and credits limitations, restricting international financial exchange, and also sales and trade abroad [ 2 ].
Economic sanctions reduce people’s access to basic necessities of life by debilitating the economic situation, decreasing welfare and weakening the functions of the target country’s social systems. One of the most important areas affected through these boycotts is health. Due to the expansion of health scope, these limitations affect different parts of health system itself and as a result endanger people’s life [ 3 , 4 ].
Studies in various countries, including Iran, Iraq, Cuba, Yugoslavia and Haiti, discussed the effects of sanctions on health. In Haiti, economic sanctions have reduced incomes, increased unemployment and poverty along with mortality by 1 to 4 years, and destroyed families [ 5 ]. In Iran, especially in healthcare area, sanctions have resulted in increasing the cost of essential procedures and drugs such as diagnostic procedures for cancers and chemotherapy drugs. The difficulties in getting required licenses for financial transactions and transportation insurance due to sanctions has left the country with a shortage of drugs and health equipment [ 6 ].
Sanctions have devastating effects on the health of vulnerable patients or health systems customers too. Patients who are suffering from diseases such as asthma, thalassemia, hemophilia, chronic diseases, blood disorders, multiple sclerosis and HIV/AIDS have limited access to drugs [ 7 ]. While comparing, in developed countries mortality rates decreased using appropriate drugs [ 8 , 9 ].
Different countries may use broad policies to prevent or adjust the negative effects of economic problems on health systems, although these policies may not be successful in ensuring continued access to health services [ 10 , 11 ].
Although sanctions may be designed for excluding medical products from the list, they can still have an inevitable impact on access to health services. Thus, the imposition of economic sanctions can threaten public health directly [ 12 ].
Furthermore, economic sanctions suppress the health indirectly by adversely impacting on other related parts known as social determinants of health (SDH) and Sustainable Development Goals (SDGs). Economic sanctions impact all aspects of the social determinants of health (SDH) framework, leading to negative effects on health equity and well-being. Sanctions can alter social and political systems, such as governance, labor markets, education, trade, housing, and redistributive policies, influencing people’s health. Structural determinants like income, education, and occupation are affected by sanctions, changing health opportunities and status, especially for the economically disadvantaged. Intermediary determinants, including material and psychosocial circumstances, are also influenced negatively by sanctions. For instance, housing quality declines post-sanctions due to increased costs of land and materials, while food consumption patterns shift towards cheaper, less nutritious options. Sanctions create psychosocial stressors like job insecurity and uncertainty, leading to frustration and stress [ 13 , 14 , 15 , 16 ].
Continued sanctions may hinder countries’ progress towards achieving Sustainable Development Goals (SDGs), particularly SDG-3 for healthy lives and well-being. Economic stability is crucial for meeting health-related SDGs, and any failures in this regard would disproportionately impact citizens in targeted countries. In the context of developing countries, where progress toward SDGs is often hindered by limited resources and systemic disparities, the impact of economic sanctions on health systems and overall well-being is profound. SDGs, with their emphasis on health (Goal 3) and the overarching aim of leaving no one behind, seek to address disparities and ensure equitable access to healthcare services. Economic sanctions, however, disrupt this delicate balance, exacerbating existing inequalities and impeding the ability of nations to meet the health-related targets outlined in the SDGs [ 13 ].
Given that, the effects of sanctions depend on the situation of countries and vary from one to another, there is no complete evidence of a comprehensive impact of sanctions on different part of society’s system especially in health despite of its importance. To comprehensively address these issues, a rigorous examination of evidence through narrative systematic reviews becomes imperative. This study aims to provide a detailed narrative synthesis of the direct and indirect effects of economic sanctions on health system building blocks and public health focusing on social determinants of health, thereby contributing to a better understanding of the broader consequences of such measures.
The following steps were taken to review literature systematically [ 17 , 18 ].
Research question
The main question that we wanted to answer in this study was to investigate and categorize the effects that economic sanctions impose on health directly and indirectly.
Search strategy and identifying literature
This systematic review was carried out according to the latest version of PRISMA guidelines [ 19 , 20 ]. For the purposes of the study, following databases were searched by one of the authors experienced in systematic research: Cochrane Library, PubMed, Embase, Scopus, Web of Science, SID, Magiran, Irandoc. The search strategy (see Additional file 1 for an example) was first devised for use in PubMed and subsequently adapted for the other databases. The search was limited to papers published between January 1990 and July 2023 and to studies involving economic sanctions independently as a hard power exercise. Other hard power exercises to achieve foreign policy goals such as war and conflicts were excluded. We selected the appropriate keywords from studying similar studies, discussion among research team and intended frameworks for extracting the data. The search term “sanctions” and “public health” were used for PubMed; terms associated with “economic sanctions” and “public health” were used for the title or abstract in the other databases if required (MeSH term; major focus and/or exploded depending on the database). In brief the following terms were searched using Boolean operators: sanction, embargo, health, human resource, medical instrument, medicine, pharmaceutics, disease, mortality, medical equipment, medical devices, drug, health care, Taskforce, health personnel, health workers, morbidity, illness, and food.
Screening and article selection criteria
Duplicate results were removed after searching the databases using Endnote software version X8. After removing the duplications, a screening of publications, based on titles and abstracts was performed by two researchers independently. In second screening, then, the suspected documents were re-examined by a third person from the research team to decide whether to enter or not.
As the final step of screening, the full texts of the remaining publications were independently assessed for inclusion by pairs of reviewers once more and any potential disagreements were resolved through consensus and if necessary by the third opinion from the research team.
The articles not meeting the below criteria were excluded:
Articles published in languages other than English and Persian.
Articles available in preprint servers.
Articles did not match the question and objectives of the research like those related to the effects of wars and conflict on health.
Conference abstracts, books, reports and dissertations.
Records not in line with the quantitative, qualitative and mixed-method original articles including letter to Editor, commentary, opinion/viewpoint/perspective.
Articles published before 1990.
After reaching the final list of studies to be reviewed thoroughly, we supplemented our database search by screening bibliographic of chosen articles to identify any additional relevant publications. The bibliographic of other relevant systematic articles were also searched actively for retrieving other missing articles.
Data extraction
After finalizing the final list of articles, the full text of the selected articles were studied precisely and required information was extracted. In order to capture the maximum available evidence regarding the effects of economic sanctions, no quality assessment was employed in our systematic literature review. This approach allowed us to include a wide range of studies, regardless of their methodological quality, thus providing a comprehensive overview of the existing literature. This method is consistent with approaches used in narrative synthesis where the primary aim is to summarize broad evidence on a topic rather than critically appraise each study’s quality. The extracted information was divided into two sections. The first one, consisting the bibliographic information included the title of article, the year of publication, the first author, and the title of the journal and the second section reports the frequency of articles according to the main topics addressed in their results.
Data analysis and presenting results
For identifying key concepts and main themes, each of selected articles studied carefully. After completing the data extraction table, the researchers shared the concepts with other members of the research team, and agreement was reached. As many other factors outside the borders of health system affects the health, generally known as social determinants of health (SDH), we applied two common popular frameworks to categorize the direct and indirect effects impacts of sanctions on health system and public health. To address the direct impact of sanctions on health, Health System Building Blocks framework proposed by World Health Organization (WHO) was proposed which consists of six key components including “service delivery”, “health workforce”, “health information systems”, “access to essential medicines”, “financing” and “government/ leadership”. This framework also covers intermediate (e.g. access, coverage, quality and safety) and four final goals including Improved health (level and equity), Responsiveness, Social and financial risk protection, and Improved efficiency [ 21 , 22 ].
To cover other effects of sanctions occurring in other sections beyond the health system but affecting health indirectly, the approach of “Social Determinants of Health” was applied which comprises of the following 10 elements, “The social gradient”, “Stress”, “Early life conditions”, “Social exclusion”, “Work”, “Unemployment”, “Social support”, “Addiction”, “Food”, and “Transport“ [ 23 ].
Search process
A total number of 18,219 articles were identified, which after removing the overlaps, 12,838 articles remained. Following the initial review of the title and abstract of all retrieved articles, a further 12,439 articles were excluded. Out of 399 records, the full text of 390 articles were retrieved and evaluated for eligibility.
After a final review, 331 articles were excluded due to not intended study design or not addressing the question and aims of the current research. Finally 59 research articles were included in the study (Fig. 1 ). A summary of included studies’ features is reported in Table 1 .

The PRISMA algorithm of study selection process
Study features
The study information collected from 11 countries which included Iran, Iraq, Cuba, Syria, Haiti, Yugoslavia, Lebanon, Serbia, Nicaragua, Sri Lanka, Russia and South Africa. Iraq [ 4 , 24 , 25 , 26 , 27 , 28 , 29 , 30 , 31 , 32 , 33 , 34 , 35 ] and Iran [ 36 , 37 , 38 , 39 , 40 , 41 , 42 , 43 , 44 , 45 ] had the maximum number of studies. Most of the studies were descriptive or analytical. Four were qualitative and also three studies were designed as a mix-method. The share of different regions from economic sanctions studies is shown in Fig. 2 .

The different regions share of economic sanctions studies
Study areas
Included studies have examined the impact of sanctions in various areas. The amount of available and accessible information about the effect of sanctions varied from one area to another. Most studies addressed the impact of economic sanctions on access to medicine or food and also socioeconomic status.
Almost half of studies mentioned the effect of sanctions on access to drugs, these studies covered approximately all countries targeted by sanctions. More than a quarter, discussed the socioeconomic situation. Food access and malnutrition were also explained in about another quarter of the articles. According to studies, the vulnerable groups which affected most by sanctions were the poor, patients, women and children. The proportion of different parts of health system and different social health determinants affected by economic sanctions is reported in Table 2 ; Fig. 3 .

The proportion of different parts of health system and social determinants of health mentioned in retrieved studies which are affected by economic sanctions
The Table 2 provides an overview of the frequency of direct and indirect effects of sanctions on health, based on findings from 59 selected articles. The data is categorized into direct effects on the health system and indirect effects on population/public health, highlighting both the immediate and broader consequences of sanctions. The most frequently mentioned direct effect was the impact on access to essential medicine, medical products, vaccines, and technologies, with 22 documents, accounting for 37.3% of the papers. On the other hand, the most frequently cited indirect effect was on the socioeconomic situation, mentioned in 9 documents (15.2%).
Themes and sub-themes
The effects of sanctions on health were categorized into two broad direct and indirect groups. Following the WHO’ Health System Building Blocks, direct effects include 7 main themes as followed: access to essential medicine, medical products, vaccines and technologies; financing; health workforce; service delivery; research and health information systems; health outcomes; and financial risk protection (Table 3 ). Indirect effects also were summarized in 6 main themes consisting: socioeconomic status; food and agricultural products; stress; early life conditions; high-risk behaviors and addiction; and transportation (Table 4 ).
Direct effects
Access to medicines, medical products, vaccines, and technologies.
Access to medicine is one of the main goals of health systems. Numerous studies have been reported on drug shortages and public concerns about patients’ difficulties for getting their essential’s [ 46 ]. The findings related to access to medicine were divided further into three sub-themes: reduced access to imported raw materials, decreased access to imported or foreign drugs, and increased drug prices.
There are some findings indicated that sanctions prevent the import of essential medical supplies [ 29 , 36 , 44 , 47 , 48 ]. Therefore, the manufacture of local drugs is affected and access to them is reduced.
For example, Iran experienced a significant decrease in access to asthma drugs which produced locally in Iran, because of local producers relied on imported raw materials [ 36 ]. In Yugoslavia, as a result of imposing restrictions on pharmaceutical industry, the available essential drugs decreased by more than 50% [ 47 ]. Syria also faced a shortage of raw materials for producing domestic drugs for heart disease, cancer and diabetes [ 48 ]. In a similar way, in Iraq, the provision of laboratory services reduced because of raw chemicals shortage [ 29 ].
Limited access to imported drugs was another direct effect [ 49 ]. The shortage of essential medicines in countries suffering from sanctions was a main concern and access to such medicines including chemotherapy, chronically illness treatments, psychiatric services, MS and antiepileptic drugs was limited considerably [ 29 , 31 , 36 , 37 , 40 , 42 , 44 , 47 , 50 ]. Access to hemophilia and thalassemia drugs was severely affected too [ 39 ]. Problems caused by economic sanctions also affected the pharmaceutical market which as a result, lead to an sharp increase in the prices [ 5 , 42 , 51 ].
Studies showed that economic sanctions reduced the import of and access to medical equipment to great extent [ 3 , 24 , 29 , 52 ]. In Cuba, the number of X-rays decreased by 75% [ 3 ]. Many American companies refused to sell drugs or medical equipment assigned for Nicaragua. Severe shortage of medical products in health system became apparent in 1985 and worsened in 1986 [ 24 ].
Also, studies revealed that economic sanctions have reduced access to vaccines and caused less immunization against infectious diseases [ 25 , 53 ].
In case of Cuba, the country’s ability to produce chlorine decreased and the number of populations with no access to safe drinking water increased, therefore population covered by chlorine water systems decreased from 98% in 1988 to 26% in 1994 [ 3 ].
Health financing
Health financing counts as essential ability of health systems to maintain and improve the community well-being. The economic crisis is affecting the financial capacity of health care system and has hampered the financial support for providing health services [ 52 , 54 ]. During the economic sanctions, budget constraints also prevented some health care programs from being fully implemented [ 31 ].
Health workforce
A study done in Iraq showed that economic sanctions resulted in widespread expulsions of health care professionals, while many of them were belong to foreign nationals. Also, physicians had to do a lot of extra work, along with increasing pressures which caused them.
leave their jobs behind [ 29 , 31 ].
Health services delivery
The imposition of economic sanctions, resulted in labor shortages, limited access to medical equipment, affecting the process of providing health services and made it worse. This imposed much more pressure on the ability of health system as whole particularly during crises like the COVID-19 pandemic [ 55 ]. Meanwhile various studies showed a reduction in quantity and quality of provided services too [ 5 , 29 , 31 , 52 , 56 , 57 ]. A study in Iran showed that due to economic sanctions, from 18 brachytherapy centers in 2018, only two centers were usable since 2015 and also the gap between Iran’s available facilities for radiation therapy and international standards deepened [ 58 ]. According to the Program of Action for Cancer Therapy, sanctions have disrupted Iran’s National Cancer Control Program (NCCP) as they have influenced all phases of treatment from prevention, to diagnosis/treatment, palliative care, monitoring, and also technology and drug availability [ 59 ].
Research and health information systems
The effects of economic sanctions on research and health information systems were divided into three sub-themes: reduced access to scientific resources and virtual sites, disruption of international interactions and conferences, and restricted research activities. Sanctions also limited access to scientific magazines and books [ 29 , 52 ]. Specialists were unable to get visas and travel abroad to attend international conferences, which reduced scientific exchanges [ 52 ].
The severe financial pressure of sanctions intensified restrictions of scientific travels and communications with the outside world led to a lack of access to educational materials and global medical advances [ 31 ].
Economic sanctions also had negative effects on both research and science production activities, including smaller scientific communication, difficulties in research processes, and consequently, decline in the quality along with quantity of research and science development activities [ 14 , 45 , 60 ].
Health outcomes and financing risk protection
International evidence about the UN sanctions indicates that they reduces life expectancy by about 1.2–1.4 years on average. It was also shown that this reduction is much more severe in vulnerable groups of society like women. This lower life expectancy in the studied countries occurred to great extent due to higher child mortality and Cholera deaths and also spending less amount of public budget on health care [ 61 , 62 ]. Studies from Iran show that multiple sclerosis patients faced higher out-of-pocket payments, catastrophic health expenditures and the poverty index [ 63 ]. Similarly, studies from other countries show higher mortality rate from infectious diseases and more difficulties for optic and neuropathic patients [ 64 , 65 ]. Physical rehabilitation experts in Iran also concern about high price that people with physical problems have to pay for prostheses which in turn have negative consequences for practitioners themselves [ 66 ].
Indirect effects
The effects of economic sanctions are not targeted and they also influence sectors other than health which can affect general health indirectly. These effects can be categorized under a general concept as social determinants of health (SDH). The main SDHs extracted from the retrieved studies are as follows:
Economic and social status
The main target of economic sanctions is the economy and money flows of countries which had negative consequences for countries’ economy themselves and other related areas [ 67 ]. The indirect outcomes in the area of Economic and Social Status were categorized into 6 sub-themes including: rising unemployment, decreasing income, declining welfare, increasing poverty, trade barriers, rising prices and decreasing purchasing power.
Majority of studies in Iran, Iraq, Cuba, Haiti, Syria, South Africa addressed the effects of sanctions on the socioeconomic situation [ 4 , 5 , 29 , 44 , 47 , 48 , 52 , 68 ]. These sanctions banned and reduced the exports of products which in turn caused unemployment among those who relied on importing such products to make money. Unemployment rose sharply in Haiti with the cessation of mango exports, on which many poor people depended [ 47 ]. Also, in this country some of factories such as clothing, sports and assembly, reduced the number of workers, which was accompanied by rising the rate of job loss [ 5 ].
Continuing this situation, economic problems became more and more prevalent. In Haiti, many people lost their main source of income [ 5 ]. In Iraq, wage fell and there was hardly enough to buy the necessities of daily life [ 29 ]. A review of studies during this period revealed that the reason of increasing social problems and the disintegration of many family structures was the fall in incomes [ 5 , 44 ].
On the other hand, poverty increased as soon as economic problems intensified. Some of the middle classes’ families were forced to sell their houses and apartments [ 29 ]. Also, school enrollment declined due to the poverty [ 5 ].
Another important effect was trade barriers so that reduced the rate of investment and the number of foreign companies. The number of active American companies in South Africa fell from 267 in 1986 to 104 in 1991 [ 47 ]. Loss of markets, credits, and favorable trade conditions, devaluation of the national currency against the US dollar, the oil exports stoppage, alongside the reduction of basic goods imports were among the other effects [ 29 , 47 , 48 ]. On the other hand, prices increased while purchasing power decreased [ 4 , 5 , 48 , 52 ].
Food and agriculture
Numerous studies in Iran, Cuba, Iraq, and Haiti have shown that economic sanctions reduced food imports while increased their prices, and restricted proper diet 41) [ 3 , 5 , 24 , 29 , 47 ]. In Cuba, food imports decreased by almost 50% from 1989 to 1993 as a result of falling rate of imports while shifting to low-quality protein products which posed serious threats on population’s health. In Haiti, staple food prices increased fivefold from 1991 to 1993 [ 47 ]. Likewise, the prices of all food groups increased significantly in Iran in 2018 due to the limitations in international financial exchanges, right after the re-imposition of sanctions. The price increase was higher in vegetable, meat, and fruit groups which made it nearly impossible to follow a healthy diet [ 69 ].
Prices of basic commodities such as wheat, rice and sugar rose in Iraq, too [ 29 ]. On the other hand, the lack of foods containing B vitamins group in Cuba led to the epidemic of neuropathy [ 47 ]. Poor nutrition among pregnant women in Iraq increased anemia [ 24 ]. Meal and per capita protein intake decreased [ 3 , 5 ]. At the same time malnutrition also increased during restrictions [ 5 , 35 , 47 , 70 ] and furthermore caused reduction in crop production and agricultural support [ 5 , 71 ]. Other studies also revealed that availability and stability were the most affected dimensions of food security following imposing economic sanctions [ 72 ]. A study about the impact of the UN and US economic sanctions on the environment in Iran found that while these sanctions initially improved Iran’s environment in the short term, they had long-term damaging effects [ 73 ].
Economic sanctions exacerbate stressful conditions. According to studies, increased fear and uncertainty, and increased mental health problems are among the negative effects of sanctions in this category [ 5 , 31 , 48 , 53 , 74 ].
Early life conditions
A good start in life means supporting mothers and young children. A study found the exposure to adverse economic conditions in infancy and early childhood was effective in long-term negative health outcomes [ 75 ].
High-risk and addictive behaviors
People turning to high-risk behaviors and addiction along with their consumption patterns can be affected and intensified by economic and social conditions. According to the findings, the effects of economic sanctions in case of risky and addictive behavior were categorized into two sub-groups consist of increasing high-risk behaviors and addiction.
As evidences revealed, economic sanctions increased suicide and violence. Studies shown that the rate of deaths caused by violence and suicides have increased in Yugoslavia and Cuba during limitation periods [ 3 , 47 ]. In Haiti, charges against children, criminal conspiracy, robbery, and drug use were much more serious [ 5 ] and this happened along with another important result which was changing in drug use patterns and increased drug abuse problems.
The common use of syringes for drug injection has increased, posing a risk to abusers. Due to economic problems, people entered mass drug distribution networks and drug trafficking to make money; tried steal or other illegal ways to earn money for buying or supplying drugs. Rising drug prices have led to the neglect family economic basket and reduced attention to the factors such as education and health care, which have resulted in low quality of life for consumers and their families [ 41 ].
According to the studies, economic sanctions in different countries affected communities’ health in different ways. Economic sanctions are supposed to force a country’s government to reconsider its policies by putting and imposing economic pressure. Although they should not target humanitarian goods, studies in various countries have revealed their direct and indirect effects on community’s health and threats for people’s right to health. The most important effects were found in the access to medicine and change in socio-economic conditions, while ensuring access to medicines for people who needed them, is one of the most emphasized goals of health systems all around the world [ 76 ]. Clearly economic sanctions suppress economic growth of the targeted countries in different ways and the lower economic situation can influence all aspects of the whole community and people’ life including their health status directly and indirectly. The World Bank data confirm that sanctions reduced Iran’s economic growth by 38% within three years, as GDP per capita dropped from US$ 7833 in 2012 to US$ 4862 in 2015. Moreover, unemployment increased from 10.4% in 2013 to 13.1% in 2017, and the economic inequality in household expenditure, measured by Gini coefficient, increased from 37 to 41%, since 2012, due to economic sanction. Clearly this economic inequality can lead to health inequity in population [ 77 ]. When the economic situation worsens in general, the financial capacity of health system and also the financial power of people will be affected. Evidence from different studies proved that the general budget of health decreased and out-of-pocket payments increased especially for those patients who depend on foreign and imported drugs [ 54 , 63 ].
In the present study, surveys in different countries showed that economic sanctions through devaluing the national currency, affected access to health goods and services, including drugs and medical equipment. Countries depending on drug technology, requiring the imported raw materials, experienced a severe restriction for accessing to medicine and drugs. On the other hand, these limitations caused a sudden increase or inflation in the prices of medicine and equipment. This effect would be worse for people who suffer from chronic diseases and are unable to purchase or use health care services [ 16 ]. For example, sanctions in 2011 caused a 14 times increase in the price of formula in Iran for infants suffering from food allergies. Besides that, uncertainty about the availability of drugs following sanctions also changes the behavior of people as the stored formula for infants not needing a specific formula which was enough for 2 months was distributed only within 4 days in September, 2018 [ 78 ].
This is while the economic sanctions reducing the power of supporting health services by limiting budgets and funds. Health financing is essential for the ability of health systems to maintain and improve human health through keeping them capable to fund and provide health services. Without the necessary funding, no health workers will be hired, no medication will be available, and as the same way, no health promotion or prevention will take place [ 23 ]. As a result, considering the negative impact of sanctions, the financing system faces serious problems in three main functions of resource collection, pooling, and purchasing. The ability of countries to achieve health system’s goals largely depends on the knowledge, skills, motivation and deployment of individuals to organize and provide health services [ 23 ]. Numerous studies showed evidence of a direct relationship between health human resource and population outcomes [ 79 , 80 ].
Sanctions made it impossible to strengthen service delivery for achieving the Millennium Development Goals (MDGs) related to health by reducing the rate of occupied health workforce and forcing them to migrate. Studies assessed the impact of economic crises shown that these restrictions affected the health sector by increasing public vulnerability as same as the inability to meet public needs and expectations due to limited resources [ 81 , 82 , 83 ]. The findings from Iran show that sanctions can influence health care delivery adversely during health pandemics like COVID-19 disease in various direct and indirect ways [ 55 ]. Therefore, if sanctions continue, the reduction of inputs will hinder the improvement of service delivery and access to them. On the other hand, they disrupt access to health services even though with minimum quality standards.
About the research, sanctions limited and disqualified research activities by banning the access to most scientific and valid resources and disrupting international interactions and conferences. The small and isolated scientific communication has slowed down the health promotion progresses and limited the access to standards and protocols for promoting public health based on scientific evidence [ 31 , 45 ].
At the same time, economic sanctions affected on social determinants of health in various dimensions. Loss of markets, credits and favorable trading conditions reduces the value of the national currency and the ability to import goods. While, the cost of basic goods is strongly affected and prices increased [ 47 , 48 ]. Thus, sanctions forced severe negative effects on people’s health status by reduction of income, welfare, along with increasing unemployment and poverty [ 5 , 29 , 84 ]. This negative impact is more evident on the poor. These people cannot access or buy high or even sometimes low quality health care services.
Another effect of sanctions is reducing access to the food. Sanctions will restrict access to enough food for countries which import their agricultural products. Countries producing their own food products have better resilience. Limitation on access to basic material and food, as well as the economic pressures and declining incomes, affect the pattern of food consumption. Increasing the price of all kinds of food, turning to poor quality and unhealthy foods, as well as buying cheaper, low-nutrient ones, exacerbate malnutrition and make following a healthy diet impossible [ 69 , 70 , 85 ]. It should be noted that imposing sanctions are not always bad and sometimes they force countries to redesign their internal processes. The experience of Russian shows that although sanctions adversely influence agriculture to some extent but instead they played as the new momentum and help its dairy and milk sector to devise positive changes and increase the volume of inter-regional trade in milk and dairy products [ 86 ].
From a psychological point of view, the poor and fragile economic situation reduces the value of assets as same as the loss of purchasing power, which leads to increased frustration and stress in people. Frustration and despair cause and exacerbate various diseases [ 87 ]. Stressful situations also make people feel anxious, worried and unable to cope with. Psychosocial risks accumulate throughout life and increase the likelihood of poor mental health and premature death [ 23 ]. Findings from Iran proved that sanctions also affect mental health adversely. According to the WHO’ data, sanctions led to an increase in death due to self-harm and interpersonal violence in Iran (from 5.9 to 6.1 and from an average of 2.0 to 2.7 per 100,000 persons respectively) during the 2011–2014 period. Interestingly the self-harm related death reduced again in 2016, a year after lifting the sanctions [ 77 ].
Risky behaviors and addiction are taking as new behaviors patterns as a result of economic hardships and raised prices. Drug abuse has devastating effects on human health, while increase the rates of crime and mortality [ 88 ]. The highest incidence rate of HIV is among drug abusers and their sexual partners [ 89 ]. Thus, sanctions intensify these behaviors and patterns with a growing trend, which counts as a great threat to society and especially health system. A review of literature provides many evidence of sanctions effects on health while evidence was provided for most affected areas.
Many studies looked at the effects on access to medicines and medical equipment, research and health information systems, the socioeconomic situation, food and agriculture, and provided a clear picture of consequences. Although some others, focused on one specific area, the others discussed about the issues such as government or leadership, early life conditions, social isolation, social support, transportation which were less in number with no complete and clear evidence that needs further investigation. The most studies in our review examined the effects of sanctions using data and their analysis, or the pre- and post-sanctions situation. Therefore, according to our methodology and included studies, the extracted evidence is very valuable and reliable.
Understanding the impact of economic sanctions on health systems and social determinants of health is crucial for policymakers, highlighting the importance of collaborative global health governance. To address these challenges, a comprehensive approach is needed to minimize harm to vulnerable populations and promote a more equitable and resilient global health environment. Policymakers must reevaluate the effectiveness and unintended consequences of sanctions on health systems, prioritizing humanitarian concerns and ensuring that public health is not disproportionately affected. It is essential to explore alternative diplomatic strategies that allow for humanitarian exemptions within sanctions to guarantee the continued access to essential medical supplies for affected populations. Global health diplomacy should be leveraged to advocate for the removal or modification of sanctions hindering progress towards health-related Sustainable Development Goals (SDGs). Dialogue and negotiation should be prioritized to address underlying tensions while safeguarding the health and well-being of impacted communities. Establishing robust monitoring systems to track the impact of sanctions on health outcomes and social determinants is crucial. Strengthening multilateral collaborations and partnerships to address the health effects of sanctions is imperative, with international organizations like the World Health Organization (WHO) and United Nations (UN) playing a pivotal role in promoting global cooperation and finding solutions.
Strengths and limitations of the study
One of our limitations was the lack of access to the full text of some articles due to their publication time. Other studies may have been published in other languages about sanctions are excluded because of inclusion criteria. Other limitations may include losing articles about the impact of sanctions on various aspects of the health system that have lost their chance to be published due to political reasons.
Although the present study examined the impact of sanctions on the health system based on the Health System Building Blocks framework of the World Health Organization and using the approach of European SDH, it seems that in some areas the effects are not clear and further studies need to be done. However, given that the impact of sanctions varies from one country to another, the study has provided comprehensive evidence of the impacts along with consequences on health. The present evidence provides guide and helps with the adoption of international policies considering the goals of the WHO and the promotion of peace all around the world.
The results showed that economic sanctions imposed on different countries, directly and indirectly have strong negative impacts on health. Escalation of sanctions will be a severe threat and barrier for achieving the goal of global health coverage for everyone and everywhere. The international communities must work and focus on reducing the negative effects of these restrictions. They must anticipate the human effects and use whatever means are needed to prevent them. Some of these negative effects like disability and death, are irreversible. Therefore, it seems better for decision makers to recommend an international prescriptive to prevent such irreparable effects on the population of target countries before imposing sanctions.
Data availability
All data generated during the current study would be available from the corresponding author on reasonable request.
Abbreviations
Social Determinants of Health
Sustainable Development Goals
World Health Organization
Davis L, Engerman S. History lessons sanctions: neither war nor peace. J Economic Perspect. 2003;17(2):187–97.
Article Google Scholar
M E. Effect of Economic Security sanctions on the Organization United Nations in the enjoyment of human rights. Q J Foreign Policy. 2012;21(1).
Garfield R, Santana S. The impact of the economic crisis and the US embargo on health in Cuba. Am J Public Health. 1997;87(1):15–20.
Article CAS PubMed PubMed Central Google Scholar
Peksen D. Economic sanctions and human security: the public health effect of economic sanctions. Foreign Policy Anal. 2011;7(3):237–51.
Gibbons E, Garfield R. The impact of economic sanctions on health and human rights in Haiti, 1991–1994. Am J Public Health. 1999;89(10):1499–504.
Hassani M. Impact of sanctions on cancer care in Iran. Archives Bone Joint Surg. 2018;6(4):248.
Google Scholar
Gorji A. Sanctions against Iran: the impact on health services. 2014.
Shen J, Oraka E. Complementary and alternative medicine (CAM) use among children with current asthma. Prev Med. 2012;54(1):27–31.
Article PubMed Google Scholar
Adams R, Smith B, Ruffin R. Factors associated with hospital admissions and repeat emergency department visits for adults with asthma. Thorax. 2000;55(7):566.
Kheirandish M, Rashidian A, Kebriaeezade A, Cheraghali AM, Soleymani F. A review of pharmaceutical policies in response to economic crises and sanctions. J Res Pharm Pract. 2015;4(3):115.
Article PubMed PubMed Central Google Scholar
Vogler S, Zimmermann N, Leopold C, de Joncheere K. Pharmaceutical policies in European countries in response to the global financial crisis. South med Rev. 2011;4(2):69.
Ahmadi AM, Meskarpour_amiri M. The public health effects of economic sanctions as a global concern in 21th century: why the economic sanctions is a cruel strategy. J Health Policy Sustainable Health. 2015;2(1).
Lim S. The paradox of unsustainability in UN Sustainable Development Goals (SDGs): the North Korean case in the context of accountability and the fragile states under sanctions. J Peace Unification. 2021;11(1):55–78.
Kokabisaghi F, Miller AC, Bashar FR, Salesi M, Zarchi AA, Keramatfar A et al. Impact of United States political sanctions on international collaborations and research in Iran. BMJ Global Health. 2019;4(5).
Solar O, Irwin A. A conceptual framework for action on the social determinants of health. WHO Document Production Services; 2010.
Yazdi-Feyzabadi V, Amini-Rarani M, Delavari S. The health consequences of economic sanctions: call for health diplomacy and international collaboration. Arch Iran Med. 2020;23(pecial):S51.
Khan KS, Kunz R, Kleijnen J, Antes G. Five steps to conducting a systematic review. J R Soc Med. 2003;96(3):118–21.
Dehkordi AH, Mazaheri E, Ibrahim HA, Dalvand S, Gheshlagh RG. How to write a systematic review: a narrative review. Int J Prev Med. 2021;12.
Moher D, Liberati A, Tetzlaff J, Altman DG, Group* P. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Ann Intern Med. 2009;151(4):264–9.
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372.
Manyazewal T. Using the World Health Organization health system building blocks through survey of healthcare professionals to determine the performance of public healthcare facilities. Archives Public Health. 2017;75(1):1–8.
Organization WH. Everybody’s business–strengthening health systems to improve health outcomes: WHO’s framework for action. 2007.
Wilkinson RG, Marmot M. Social determinants of health: the solid facts. World Health Organization; 2003.
Abbas WAK, Azar NG, Haddad LG, Umlauf MG. Preconception health status of Iraqi women after trade embargo. Public Health Nurs. 2008;25(4):295–303.
Ali H. Hepatitis B infection among Iraqi children: the impact of sanctions. EMHJ-Eastern Mediterranean Health Journal, 10 (1–2), 6–11, 2004. 2004.
Al-Ani ZR, Al-Hiali SJ, Al-Farraji HH. Secular trend of infant mortality rate during wars and sanctions in Western Iraq. Saudi Med J. 2011;32(12):1267–73.
PubMed Google Scholar
Daponte BO, Garfield R. The effect of economic sanctions on the mortality of Iraqi children prior to the 1991 Persian Gulf War. Am J Public Health. 2000;90(4):546.
Ali MM, Shah IH. Sanctions and childhood mortality in Iraq. Lancet. 2000;355(9218):1851–7.
Article CAS PubMed Google Scholar
Akunjee M, Ali A. Healthcare under sanctions in Iraq: an elective experience. Med Confl Survival. 2002;18(3):249–57.
Ascherio A, Chase R, Cote T, Dehaes G, Hoskins E, Laaouej J, et al. Effect of the Gulf War on infant and child mortality in Iraq. N Engl J Med. 1992;327(13):931–6.
Younis MS, Aswad AM. The impact of war and economic sanctions on the mental health system in Iraq from 1990 to 2003: a preliminary report. Intervention J Mental Health Psychosocial Support Confl Affected Areas. 2018;16(1):54–8.
Al-Taee IKS, Al-Shamaa I. Long term follow-up of renal transplant patients-A single center experience in Iraq. Saudi J Kidney Dis Transplantation. 2005;16(1):40–5.
Garfield R, Leu C-S. A multivariate method for estimating mortality rates among children under 5 years from health and social indicators in Iraq. Int J Epidemiol. 2000;29(3):510–5.
Dewachi O, Rizk A, Singh NV. (Dis) connectivities in wartime: the therapeutic geographies of Iraqi healthcare–seeking in Lebanon. Glob Public Health. 2018;13(3):288–97.
Awqati NA, Ali MM, Al-Ward NJ, Majeed FA, Salman K, Al-Alak M, et al. Causes and differentials of childhood mortality in Iraq. BMC Pediatr. 2009;9:1–9.
Ghiasi G, Rashidian A, Kebriaeezadeh A, Salamzadeh J. The impact of the sanctions made against Iran on availability to asthma medicines in Tehran. Iran J Pharm Research: IJPR. 2016;15(3):567.
PubMed PubMed Central Google Scholar
Kheirandish M, Rashidian A, Bigdeli M. A news media analysis of economic sanction effects on access to medicine in Iran. J Res Pharm Pract. 2015;4(4):199.
Rad EH, Delavari S, Aeenparast A, Afkar A, Farzadi F, Maftoon F. Does economic instability affect healthcare provision? Evidence based on the urban family physician program in Iran. Korean J Family Med. 2017;38(5):296.
Karimi M, Haghpanah S. The effects of economic sanctions on disease specific clinical outcomes of patients with thalassemia and hemophilia in Iran. Health Policy. 2015;119(2):239–43.
Kheirandish M, Varahrami V, Kebriaeezade A, Cheraghali AM. Impact of economic sanctions on access to noncommunicable diseases medicines in the Islamic Republic of Iran. East Mediterr Health J. 2018;24(1):42–51.
Deilamizade A, Esmizade S. Economic sanctions against Iran, and drug use in Tehran, Iran: a 2013 pilot study. Subst Use Misuse. 2015;50(7):859–68.
Asadi-Pooya AA, Tavana B, Tavana B, Emami M. Drug adherence of patients with epilepsy in Iran: the effects of the international economic sanctions. Acta Neurol Belgica. 2016;116:151–5.
Asadi-Pooya AA, Azizimalamiri R, Badv RS, Yarali B, Asadollahi M, Homayoun M, et al. Impacts of the international economic sanctions on Iranian patients with epilepsy. Epilepsy Behav. 2019;95:166–8.
Hosseini S, Rashtchi V, Kamali K, Moghimi M. Epidemiology and outcome of 2,590 burned patients in Northwest Iran. Annals Burns fire Disasters. 2017;30(2):85.
CAS Google Scholar
Almasi K, Jamali Mahmouie H, Yousefi A. Analysis of Razi Vaccin and Serum Scientific Institute re-earchers’ viewpoint on impact of Foreign Sanctions on Scientific Communications and Research activities. Scientometrics Res J. 2016;2(1):27–42.
Setayesh S, Mackey TK. Addressing the impact of economic sanctions on Iranian drug shortages in the joint comprehensive plan of action: promoting access to medicines and health diplomacy. Globalization Health. 2016;12(1):1–14.
Garfield R, Devin J, Fausey J. The health impact of economic sanctions. Bull N Y Acad Med. 1995;72(2):454.
CAS PubMed PubMed Central Google Scholar
Sen K, Al-Faisal W, AlSaleh Y. Syria: effects of conflict and sanctions on public health. J Public Health. 2013;35(2):195–9.
Moret ES. Humanitarian impacts of economic sanctions on Iran and Syria. Eur Secur. 2015;24(1):120–40.
Sahraian MA, Moghadasi AN, Eskandarieh S. Economic sanctions against Iran as an important factor in threatening the health of patients with multiple sclerosis. Curr J Neurol. 2021;20(1):15.
Bastani P, Dehghan Z, Kashfi SM, Dorosti H, Mohammadpour M, Mehralian G. Challenge of politico-economic sanctions on pharmaceutical procurement in Iran: a qualitative study. Iran J Med Sci. 2022;47(2):152.
Nayeri K, López-Pardo CM. Economic crisis and access to care: Cuba’s health care system since the collapse of the Soviet Union. Int J Health Serv. 2005;35(4):797–816.
Allen SH, Lektzian DJ. Economic sanctions: a blunt instrument? J Peace Res. 2013;50(1):121–35.
Faraji Dizaji S, Ghadamgahi ZS. The impact of smart and non-smart sanctions on government health expenditures: evidence from developing resource-based countries. 2021.
Abdoli A. Iran, sanctions, and the COVID-19 crisis. J Med Econ. 2020;23(12):1461–5.
Kim Y. Economic sanctions and child HIV. Int J Health Plann Manag. 2019;34(2):693–700.
Whitehall J. Snake bites in north east Sri Lanka. Rural Remote Health. 2007;7(4):1–6.
Ameri A, Barzegartahamtan M, Ghavamnasiri M, Mohammadpour R, Dehghan H, Sebzari A, et al. Current and future challenges of radiation oncology in Iran: a report from the Iranian society of clinical oncology. Clin Oncol. 2018;30(4):262–8.
Article CAS Google Scholar
Shahabi S, Fazlalizadeh H, Stedman J, Chuang L, Shariftabrizi A, Ram R. The impact of international economic sanctions on Iranian cancer healthcare. Health Policy. 2015;119(10):1309–18.
Bezuidenhout L, Karrar O, Lezaun J, Nobes A. Economic sanctions and academia: overlooked impact and long-term consequences. PLoS ONE. 2019;14(10):e0222669.
Ha LT, Nam PX. An investigation of relationship between global economic sanction and life expectancy: do financial and institutional system matter? Dev Stud Res. 2022;9(1):48–66.
Gutmann J, Neuenkirch M, Neumeier F. Sanctioned to death? The impact of economic sanctions on life expectancy and its gender gap. J Dev Stud. 2021;57(1):139–62.
Gharibi F, Imani A, Haghi M, Dalal K. Relationship between political-economic sanctions and catastrophic health costs in multiple sclerosis patients in Iran. Iran J War Public Health. 2022;14(4):455–64.
Vlajinac HD, Marinković J, Kocev NI, Adanja BJ, Pekmezović T, Sipetić S, et al. Infectious diseases mortality in central Serbia. J Epidemiol Commun Health. 1997;51(2):172.
Hedges TR III, Hirano M, Tucker K, Caballero B. Epidemic optic and peripheral neuropathy in Cuba: a unique geopolitical public health problem. Surv Ophthalmol. 1997;41(4):341–53.
Shahabi S, Teymourlouy AA, Shabaninejad H, Kamali M, Lankarani KB, Mojgani P. Physical rehabilitation in Iran after international sanctions: explored findings from a qualitative study. Globalization Health. 2020;16(1):1–10.
Afesorgbor SK, Mahadevan R. The impact of economic sanctions on income inequality of target states. World Dev. 2016;83:1–11.
De Vos P, García-Fariñas A, Álvarez‐Pérez A, Rodríguez‐Salvá A, Bonet‐Gorbea M, Van der Stuyft P. Public health services, an essential determinant of health during crisis. Lessons from Cuba, 1989–2000. Tropical Med Int Health. 2012;17(4):469–79.
Hejazi J, Emamgholipour S. The effects of the re-imposition of US sanctions on food security in Iran. Int J Health Policy Manage. 2022;11(5):651.
Reid BC, Psoter WJ, Gebrian B, Wang MQ. The effect of an international embargo on malnutrition and childhood mortality in rural Haiti. Int J Health Serv. 2007;37(3):501–13.
Lv Z, Xu T. Do economic sanctions affect protectionism? Evidence from agricultural support. Econ Politics. 2019;31(1):27–42.
Afesorgbor SK. 23. Sanctioned to starve? The impact of economic sanctions on food security in targeted states. Research Handbook on Economic Sanctions. 2021:438.
Fotourehchi Z, Are. UN and US economic sanctions a cause or cure for the environment: empirical evidence from Iran. Environ Dev Sustain. 2020;22:5483–501.
Mladenovich D, Langeggen I. The impact of war and economic sanction on the incidence of retinopathy of prematurity in Serbia. J Visual Impairment Blindness. 2009;103(3):162–72.
van der Werff SD, Polman K, Ponce MC, Twisk JW, Díaz RJ, Gorbea MB, et al. Childhood atopic diseases and early life circumstances: an ecological study in Cuba. PLoS ONE. 2012;7(6):e39892.
Organization WH. Health and the millennium development goals. World Health Organization; 2005.
Aloosh M, Salavati A, Aloosh A. Economic sanctions threaten population health: the case of Iran. Public Health. 2019;169:10–3.
Danaei G, Harirchi I, Sajadi HS, Yahyaei F, Majdzadeh R. The harsh effects of sanctions on Iranian health. Lancet. 2019;394(10197):468–9.
Anand S, Bärnighausen T. Health workers and vaccination coverage in developing countries: an econometric analysis. Lancet. 2007;369(9569):1277–85.
Speybroeck N, Kinfu Y, Dal Poz MR, Evans DB. Reassessing the relationship between human resources for health, intervention coverage and health outcomes. Geneva: World Health Organization. 2006:1–14.
Rechel B, Suhrcke M, Tsolova S, Suk JE, Desai M, McKee M, et al. Economic crisis and communicable disease control in Europe: a scoping study among national experts. Health Policy. 2011;103(2–3):168–75.
Karanikolos M, Mladovsky P, Cylus J, Thomson S, Basu S, Stuckler D, et al. Financial crisis, austerity, and health in Europe. Lancet. 2013;381(9874):1323–31.
Kastanioti C, Kontodimopoulos N, Stasinopoulos D, Kapetaneas N, Polyzos N. Public procurement of health technologies in Greece in an era of economic crisis. Health Policy. 2013;109(1):7–13.
Abhari B, Aleemran R, Aghajani H. The effect of sanctions on Iran’s health system using provincial data and spatial panel methods from 2009 to 2016. J Health Adm. 2020;23(1):58–73.
Gillespie S, van den Bold M. Agriculture, food systems, and nutrition: meeting the challenge. Global Challenges. 2017;1(3):1600002.
Krivko M, Smutka L. Trade sanctions and agriculture support in milk and dairy industry: case of Russia. Sustainability. 2020;12(24):10325.
Griggs S. Hope and mental health in young adult college students: an integrative review. J PsychoSoc Nurs Ment Health Serv. 2017;55(2):28–35.
Njuho P, Davids A. Extent and influence of recreational drug use on men and women aged 15 years and older in South Africa. Afr J Drug Alcohol Stud. 2010;9(1).
Ali F, Nooshin K, Kianoosh N, Hengameh S, Abbas G. Modelling of HIV/AIDS in Iran up to 2014. J AIDS HIV Res Vol. 2011;3(12):231–9.
Download references
Acknowledgements
We are thankful to Kerman University of medical Sciences for preparing the required fund to do the study.
This study was supported financially by Institute for Futures Studies in Health, affiliated with Vice-Chancellery for Research and Technology of Kerman University of Medical Sciences.
Author information
Authors and affiliations.
Health Services Management Research Center, Institute for Futures Studies in Health, Kerman University of Medical Sciences, Kerman City, Iran
Vahid Yazdi-Feyzabadi & Anahita Behzadi
Faculty of Management and Medical Information Sciences, Kerman University of Medical Sciences, Kerman City, Iran
Atefeh Zolfagharnasab
Soheila Naghavi
Research Center of Tropical and Infectious Diseases, Kerman University of medical sciences, Kerman, Iran
Maysam Yousefi
Faculty of Health, Health Management and Economics Department, Ilam University of Medical Sciences, Ilam City, Iran
Mohammad Bazyar
You can also search for this author in PubMed Google Scholar
Contributions
VYF proposed the topic, VYF and MB designed the study; AZ did the search strategy and identified articles. MB and SN screened the articles and extracted and classified the data; AB and MY supervised and contributed in classifications of findings. VYF and AB supervised the whole process of study from literature review to data extraction. MB and AB prepared and finalized the manuscript. All authors read and approved the manuscript for submission.
Corresponding author
Correspondence to Mohammad Bazyar .
Ethics declarations
Ethics approval and consent to participate.
The registration number of proposal is 97001030 and this study was approved by the ethics committee of Kerman University of Medical Sciences with the code of ethics IR.KMU.REC.1397.564.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplementary Material 1
Rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ .
Reprints and permissions
About this article
Cite this article.
Yazdi-Feyzabadi, V., Zolfagharnasab, A., Naghavi, S. et al. Direct and indirect effects of economic sanctions on health: a systematic narrative literature review. BMC Public Health 24 , 2242 (2024). https://doi.org/10.1186/s12889-024-19750-w
Download citation
Received : 22 February 2024
Accepted : 09 August 2024
Published : 17 August 2024
DOI : https://doi.org/10.1186/s12889-024-19750-w
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Economic sanctions
- Social determinants of health
- Health system
- Systematic review
BMC Public Health
ISSN: 1471-2458
- General enquiries: [email protected]
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- My Bibliography
- Collections
- Citation manager
Save citation to file
Email citation, add to collections.
- Create a new collection
- Add to an existing collection
Add to My Bibliography
Your saved search, create a file for external citation management software, your rss feed.
- Search in PubMed
- Search in NLM Catalog
- Add to Search
Metastasis of head and neck carcinoma to the site of percutaneous endoscopic gastrostomy: case report and literature review
Affiliation.
- 1 Division of Gastroenterology and Hepatology, Mayo Clinic, Jacksonville, Florida 32224, USA.
- PMID: 11531220
- DOI: 10.1177/0148607101025005282
Background: Patients with head and neck cancer often need a percutaneous endoscopic gastrostomy to provide adequate nutrition because of inability to swallow after tumor radiation therapy. However, metastasis of the original tumor to the gastrostomy exit site may occur.
Methods: We describe the case of a 61-year-old man with stage III (T2 N1) squamous cell carcinoma of the tongue in whom a PEG tube was placed to circumvent anticipated difficulties in swallowing after radiation therapy. We also compare this case with similar cases in the literature.
Results: Soreness and erythema near the gastrostomy site reported by the patient were diagnosed as cellulitis, and two courses of antibiotic treatment were prescribed. However, a biopsy showed that the original squamous cell carcinoma had metastasized to the gastrostomy exit site. The "pull" method of tube placement had been used in this patient and in all 19 cases of metastasis reported in the literature.
Conclusions: Metastatic cancer should be considered in patients with head and neck cancer who have unexplained skin changes at the gastrostomy site. Our experience with this case and review of the literature indicate that, in patients with head and neck cancer, "pull" procedures for placement of gastrostomy tubes may induce metastasis by direct implantation of tumor cells because of contact between the gastrostomy tube and tumor cells. Methods of tube insertion that avoid such contact are preferred.
PubMed Disclaimer
Similar articles
- Metastatic head and neck carcinoma to a percutaneous endoscopic gastrostomy site. Adelson RT, Ducic Y. Adelson RT, et al. Head Neck. 2005 Apr;27(4):339-43. doi: 10.1002/hed.20159. Head Neck. 2005. PMID: 15712297 Review.
- Seeding of the percutaneous endoscopic gastrostomy site from head and neck carcinoma: case report and review of the literature. Sinapi I, Navez B, Hamoir M, Schmitz S, Machiels JP, Deprez PH, Van den Eynde M. Sinapi I, et al. Head Neck. 2013 Jul;35(7):E209-12. doi: 10.1002/hed.23015. Epub 2012 Jun 19. Head Neck. 2013. PMID: 22711678 Review.
- Metastatic head and neck cancer to the percutaneous endoscopic gastrostomy exit site: a case report and review of the literature. Schneider AM, Loggie BW. Schneider AM, et al. Am Surg. 1997 Jun;63(6):481-6. Am Surg. 1997. PMID: 9168757 Review.
- Metastatic spread to a percutaneous gastrostomy site from head and neck cancer: case report and literature review. Mincheff TV. Mincheff TV. JSLS. 2005 Oct-Dec;9(4):466-71. JSLS. 2005. PMID: 16381369 Free PMC article. Review.
- Stomal seeding of head and neck cancer by percutaneous endoscopic gastrostomy tube placement. Lee DS, Mohit-Tabatabai MA, Rush BF Jr, Levine C. Lee DS, et al. Ann Surg Oncol. 1995 Mar;2(2):170-3. doi: 10.1007/BF02303634. Ann Surg Oncol. 1995. PMID: 7728572 Review.
- Nutritional Management of Patients with Head and Neck Cancer-A Comprehensive Review. Martinovic D, Tokic D, Puizina Mladinic E, Usljebrka M, Kadic S, Lesin A, Vilovic M, Lupi-Ferandin S, Ercegovic S, Kumric M, Bukic J, Bozic J. Martinovic D, et al. Nutrients. 2023 Apr 13;15(8):1864. doi: 10.3390/nu15081864. Nutrients. 2023. PMID: 37111081 Free PMC article. Review.
- Squamous cell carcinoma implantation in gastrostomy orifice. Case report. Querichelli AFA, Faria FL, Martinez LF, Campos Junior E. Querichelli AFA, et al. Einstein (Sao Paulo). 2020 Nov 6;18:eRC5409. doi: 10.31744/einstein_journal/2020RC5409. eCollection 2020. Einstein (Sao Paulo). 2020. PMID: 33174970 Free PMC article.
- Oligometastatic recurrence of an oesophageal adenocarcinoma at a chest drain site following radical treatment: palliative treatment or resection? Wen D, Collantes E, Sgromo B. Wen D, et al. Clin J Gastroenterol. 2018 Dec;11(6):470-475. doi: 10.1007/s12328-018-0890-0. Epub 2018 Aug 25. Clin J Gastroenterol. 2018. PMID: 30145768 Free PMC article.
- Push versus pull gastrostomy in cancer patients: A single center retrospective analysis of complications and technical success rates. Currie BM, Getrajdman GI, Covey AM, Alago W Jr, Erinjeri JP, Maybody M, Boas FE. Currie BM, et al. Diagn Interv Imaging. 2018 Sep;99(9):547-553. doi: 10.1016/j.diii.2018.04.005. Epub 2018 Apr 30. Diagn Interv Imaging. 2018. PMID: 29716845 Free PMC article.
- Percutaneous endoscopic gastrostomy: indications, technique, complications and management. Rahnemai-Azar AA, Rahnemaiazar AA, Naghshizadian R, Kurtz A, Farkas DT. Rahnemai-Azar AA, et al. World J Gastroenterol. 2014 Jun 28;20(24):7739-51. doi: 10.3748/wjg.v20.i24.7739. World J Gastroenterol. 2014. PMID: 24976711 Free PMC article. Review.
Publication types
- Search in MeSH
Related information
- Cited in Books
LinkOut - more resources
Full text sources.
- Ovid Technologies, Inc.
- MedlinePlus Health Information

- Citation Manager
NCBI Literature Resources
MeSH PMC Bookshelf Disclaimer
The PubMed wordmark and PubMed logo are registered trademarks of the U.S. Department of Health and Human Services (HHS). Unauthorized use of these marks is strictly prohibited.
Subscribe to the PwC Newsletter
Join the community, edit social preview.

Add a new code entry for this paper
Remove a code repository from this paper, mark the official implementation from paper authors, add a new evaluation result row.
| TASK | DATASET | MODEL | METRIC NAME | METRIC VALUE | GLOBAL RANK | REMOVE |
|---|
- EXPLAINABLE ARTIFICIAL INTELLIGENCE
Remove a task
Add a method, remove a method, edit datasets, the literature review network: an explainable artificial intelligence for systematic literature reviews, meta-analyses, and method development.
5 Aug 2024 · Joshua Morriss , Tod Brindle , Jessica Bah Rösman , Daniel Reibsamen , Andreas Enz · Edit social preview
Systematic literature reviews are the highest quality of evidence in research. However, the review process is hindered by significant resource and data constraints. The Literature Review Network (LRN) is the first of its kind explainable AI platform adhering to PRISMA 2020 standards, designed to automate the entire literature review process. LRN was evaluated in the domain of surgical glove practices using 3 search strings developed by experts to query PubMed. A non-expert trained all LRN models. Performance was benchmarked against an expert manual review. Explainability and performance metrics assessed LRN's ability to replicate the experts' review. Concordance was measured with the Jaccard index and confusion matrices. Researchers were blinded to the other's results until study completion. Overlapping studies were integrated into an LRN-generated systematic review. LRN models demonstrated superior classification accuracy without expert training, achieving 84.78% and 85.71% accuracy. The highest performance model achieved high interrater reliability (k = 0.4953) and explainability metrics, linking 'reduce', 'accident', and 'sharp' with 'double-gloving'. Another LRN model covered 91.51% of the relevant literature despite diverging from the non-expert's judgments (k = 0.2174), with the terms 'latex', 'double' (gloves), and 'indication'. LRN outperformed the manual review (19,920 minutes over 11 months), reducing the entire process to 288.6 minutes over 5 days. This study demonstrates that explainable AI does not require expert training to successfully conduct PRISMA-compliant systematic literature reviews like an expert. LRN summarized the results of surgical glove studies and identified themes that were nearly identical to the clinical researchers' findings. Explainable AI can accurately expedite our understanding of clinical practices, potentially revolutionizing healthcare research.
Code Edit Add Remove Mark official
Tasks edit add remove, datasets edit, results from the paper edit add remove, methods edit add remove.
- Open access
- Published: 17 August 2024
Emergency robotic surgery: the experience of a single center and review of the literature
- Graziano Ceccarelli 1 ,
- Fausto Catena 2 ,
- Pasquale Avella 3 , 4 ,
- Brian WCA Tian 5 ,
- Fabio Rondelli 1 ,
- Germano Guerra 4 ,
- Michele De Rosa 1 &
- Aldo Rocca 3 , 4
World Journal of Emergency Surgery volume 19 , Article number: 28 ( 2024 ) Cite this article
95 Accesses
1 Altmetric
Metrics details
Backgrounds
Laparoscopic surgery is widely used in abdominal emergency surgery (AES), and the possibility of extending this approach to the more recent robotic surgery (RS) arouses great interest. The slow diffusion of robotic technology mainly due to high costs and the longer RS operative time when compared to laparoscopy may represent disincentives, especially in AES. This study aims to report our experience in the use of RS in AES assessing its safety and feasibility, with particular focus on intra- and post-operative complications, conversion rate, and surgical learning curve. Our data were also compared to other experiences though an extensive literature review.
We retrospectively analysed a single surgeon series of the last 10 years. From January 2014 to December 2023, 36 patients underwent urgent or emergency RS. The robotic devices used were Da Vinci Si (15 cases) and Xi (21 cases).
36 (4.3%) out of 834 robotic procedures were included in our analysis: 20 (56.56%) females. The mean age was 63 years and 30% of patients were ≥ 70 years. 2 (5.55%) procedures were performed at night. No conversions to open were reported in this series. According to the Clavien-Dindo classification, 2 (5.5%) major complications were collected. Intraoperative and 30-day mortality were 0%.
Conclusions
Our study demonstrates that RS may be a useful and reliable approach also to AES and intraoperative laparoscopic complications when performed in selected hemodynamically stable patients in very well-trained robotic centers. The technology may increase the minimally invasive use and conversion rate in emergent settings in a completely robotic or hybrid approach.
Introduction
Abdominal Emergency Surgery (AES) can be defined as a procedure requiring to deal with an acute threat to life, organ, trauma, acute disease process, acute exacerbation of a chronic disease process, or complication of a surgical or other interventional procedure, normally within hours of decision to operate [ 1 , 2 ].
Further, “expedited surgery” refers to the clinical situation exemplified by a patient in need of prompt treatment but not in imminent danger to life or organ survival; this procedure often takes place a few days after the decision to operate [ 3 ].
Nowadays, minimally invasive laparoscopic approach to urgent abdominal surgery (cholecystitis, acute appendicectomies, bowel perforation or obstruction, etc.) represents the standard of care in many cases and recent guidelines recommend it [ 4 , 5 , 6 , 7 ].
Nevertheless, after more than 20 years from clinical introduction, Robotic Surgery (RS) represents the most important technological evolution and a revolutionary concept of computer-assisted technology in minimally invasive surgery [ 8 ]. It allows to overcome many limits of conventional laparoscopy and to expand the use of minimally invasive approaches.
Its peculiar features include a three-dimensional high-definition view, articulated instruments, tremor eradication, and improved ergonomics for surgeons, enable the performance of extremely accurate procedures (micro-sutures, fine dissections, etc.) with consequently lowering conversion rates and postoperative complications, particularly in case of challenging surgical procedures [ 9 , 10 , 11 ]. In addition, compared to traditional laparoscopic surgery, RS demonstrated shorter learning curves for several complex procedures [ 12 , 13 ]. On the other hand, the main drawbacks of robotic technology are linked to its limited diffusion also due to expensive costs [ 14 , 15 , 16 , 17 , 18 , 19 , 20 ].
Nevertheless, robotic surgical technologies have expanded and evolved over the past 20 years, bringing new devices, and improving the most established ones [ 21 , 22 ].
The spreading of robotic platforms and their easier management led to increased RS applications in all abdominal surgical specialities including upper gastrointestinal surgery [ 15 , 23 , 24 , 25 ], colorectal surgery [ 26 , 27 , 28 ], HBP surgery [ 14 , 18 , 29 , 30 , 31 ], abdominal wall surgery and many others [ 7 ].
Despite the huge diffusion of RS in all surgical fields, its application in urgent scenarios has never been investigated representing a new field of interest, with limited literature experiences [ 32 ].
So considering that our experience in RS has been implemented since 2002 and it raised from general to major complex surgery [ 33 , 34 , 35 , 36 , 37 , 38 ], we aim to set the state of art of Robotic Emergency Surgery sharing our experience through the analysis of our peri-operative outcomes and indications in RS. Furthermore, due to the limited evidence available, we have as a secondary endpoint an extensive analysis of previous literature experiences.
Study design and patient selection
We retrospectively reviewed a prospectively collected database of patients undergoing RS at General and Robotic Surgery Unit of San Giovanni Battista Hospital (Foligno, Italy) and General Surgery Unit of San Donato Hospital (Arezzo, Italy) from January 2014 to December 2023.
The patients’ data were analyzed according to Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) [ 39 ]. All patients signed an informed consent allowing the anonymous scientific use of clinical data and images. The study was carried out according to the Declaration of Helsinki guidelines and was approved by the Institutional Review Board of the University of Molise (protocol number 10/21, approved date: May 12, 2021).
In all participating centres, data were prospectively collected from electronic patient records.
We selected 834 consecutive robotic procedures for abdominal surgery performed by both centres. Patients were divided into two cohorts: elective surgery and urgent or emergency surgery groups.
Urgent surgery was defined as a condition requiring surgery within 72 h in stable patients, but not suitable for discharge. Moreover, emergency surgery was defined as a clinical scenario requiring within 24 h in stable patients, with a low risk of deterioration. All patients < 18 years old and affected by hemodynamical instability were excluded.
Criteria adopted to assess baseline characteristics of patients, surgical issues and technologies that allow to benefit of RS in urgent and emergency settings are summarized in Table 1 .
Furthermore, to analyze the diagnosis and intraoperative data we carried out a specialities classification as reported in Table 2 .
Implementation of the robotic surgery program and learning curve completion
Our experience with RS started in September 2002 with the da Vinci S ® platform (Intuitive Surgical, Sunnyvale, California, USA), and over time, its application in abdominal surgery grew as well as platform technologies. During the study period, the da Vinci Si ® platform (Intuitive Surgical, Sunnyvale, California, USA) and, since 2017, da Vinci Xi ® (Intuitive Surgical, Sunnyvale, California, USA) were available at our institutions.
Beginning from colorectal surgery, hiatal hernia repairs and cholecystectomies, our surgical team have gradually selected more challenging procedures by carrying out liver and pancreatic resections, oesophageal benign and malignant disorders, bariatric surgery, abdominal wall hernia repairs and nephrectomies [ 14 , 15 , 25 , 40 , 41 , 42 , 43 , 44 , 45 , 46 , 47 ].
All procedures were performed by a well-trained surgeon in minimally invasive surgery (G.C.) with 10 years of previous experience in RS.
36 (4.3%) out of 834 robotic procedures were included in our analysis and treated as urgent or emergent procedures.
All patients signed an informed consent allowing the anonymous scientific use of clinical data and images. The study was carried out according to the Declaration of Helsinki guidelines and was approved by the Institutional Review Board of the University of Molise (protocol number 10/21, approved date: 12 May 2021).
The collected data included demographic characteristics such as age, sex, and preoperative comorbidities classified according to the Charlson comorbidity Index (CCI) [ 48 ]. The anesthetic risk assessment was performed thanks to the American Society of Anesthesiologists (ASA) score [ 49 ].
We reviewed pre-operative diagnosis, main and associated surgical procedures, operative time and intraoperative complications, and conversion to open rate. Postoperative complications were stratified according to the Clavien-Dindo classification [ 50 ] and were considered severe when ≥ 3. Patients were monitored until their 30th postoperative day.
Categorical variables were expressed as frequencies and percentages, while quantitative data were collected as means or medians and interquartile ranges.
Literature review
We performed literature research on the PubMed Dataset (US National Library of Medicine, http://www.ncbi.nlm.nih.gov/PubMed ), using the subsequent keywords: “robotic surgery”, “urgent surgery”, and “emergency surgery”. We selected only English studies. Original articles, case reports and case series were included, while editorials, letters, and reviews were excluded. Number of treated patients does not represent an exclusion criterion. Articles were first evaluated by title and abstract examination, then a full-text read was performed. More than 50 studies described RS in AES. An extensive analysis was performed to summarize similarities and differences among RS approaches according to abdominal surgery specialities.
Pre-, intra- e post-operative outcomes
36 (4.3%) out of 834 robotic procedures were included in our analysis. Baseline characteristics of patients are listed in Table 3 .
According to surgical procedures, Fig. 1 shows AES performed thanks to RS compared to elective surgery.
Over the cohort of 36 patients treated, 16 (44.44%) were males while 20 (56.56%) were females. The mean age was 63.20 years (range: 43–88 years): 30.55% [ 11 ] of patients were ≥ 70 years. The mean Body Mass Index was 26.68 kg/m 2 (range: 23–42). According to the ASA score, 8 (22.22%) patients were classified as ASA 3. No ASA 4 was treated. Patients’ CCI are listed in Table 3 . The da Vinci Si platform was used for the first 15 (41.67%) cases, while Xi for the last 21 (58.33%). 2 (5.55%) procedures were performed at night. No conversions to open were reported in this series. According to Clavien-Dindo grade, 2 (5.55%) major complication was collected: 1 after urgent surgery and 1 after emergency setting. Two minor complications requiring conservative treatments were observed: both complications were related to primary disorders and not to RS. Intraoperative and 30-day mortality were 0%. The mean length of stay was 4.92 days (range: 1–21). The mean follow-up was 26.53 months (range: 7–68).
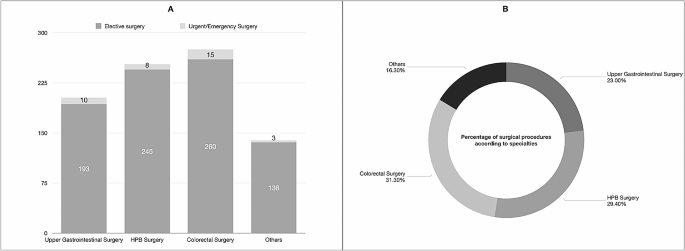
Number of elective and urgent/emergency procedures ( A ) and percentage of overall surgical procedures performed in emergency settings ( B ) according to abdominal surgery specialities. Abbreviations: HPB, Hepatopancreatic and Biliary Surgery;
Our experience demonstrates the safety and feasibility of RS also in urgent and emergency abdominal settings in patients not affected by hemodynamic instability. To date, the minimally invasive approaches in emergency scenarios are mainly validated for laparoscopy, as reported by several literature experiences included in the last WSES review [ 51 ]. Despite the diagnostic role of MIS, authors demonstrated several benefits of laparoscopic approaches in hemodynamically stable patients undergone AES, including trauma. However, patient selection, surgeons’ expertise as well as specific surgical training represent crucial key points [ 51 ].
In literature, RS in AES studies is related to high-volume centres, and well-trained surgeons’ experiences and their optimal outcomes should encourage further applications and Randomized Clinical Trials [ 32 , 52 ]. We further analyzed short- and long-term outcomes of RS in AES according to specialties (Table 4 ).
Robotic surgery in emergency setting
In the literature, RS in the emergency setting is reported by a limited number of experiences, especially case reports and case series.
The urologist experience described by Capibaribe et al. [ 53 ] demonstrated the safety and efficacy of robotic treatment in the case of vesicourethral anastomotic stenosis after open radical prostatectomy, providing better continence results, without pubectomy.
Globally, the major barrier to RS adoption is due to limited device access resulting from a shared use policy by several surgical teams (gynaecologists, general surgeons, thoracic surgeons, and urologists). Furthermore, the lack of dedicated teams (surgeons, nurses, and anaesthesiologists) during the night shift might further limit RS.
On the other hand, in emergency settings, the “time-sparing” concept is largely known. Commonly, to avoid useless costs due to waste disposable instruments, a hybrid approach should be discussed by the whole surgical team: before robotic docking, a laparoscopic exploration could be the first surgical step to verify clinical environments for doing RS.
A crucial issue is represented by frequent operating table position changes, especially during explorative steps (tilting, Trendelenburg, or reverse-Trendelenburg positions) and rapid conversion to open surgery when necessary [ 54 ]. It could be underlined that quick and safe docking and undocking are performed by skilled teams and well-trained surgeons in elective procedures [ 54 , 55 ].
In the last years, the RS technologies have also impacted operative time [ 56 ]: The Xi robot represents a radical evolution from the Si robot. Literature experiences demonstrated better docking ability during Da Vinci Xi surgery when compared to previous robotic systems (Da Vinci S, Si, X) [ 57 , 58 ]. These features were due to laser targeting and improved cannula mounts that resulted in a simplified “linear” port configuration and an abbreviated docking time.
Besides, the ability to exchange the robotic camera from port-to-port increased versatility for multi-quadrant surgeries thanks to the smaller 8 mm camera [ 59 , 60 ]. The multi-quadrant operations represent challenges due to the axis of visualization shift up to 360°. This procedure requires undocking the robot and rotating it on the axis. It is crucial for many colorectal surgeries that require access to the entire abdomen such as subtotal colectomy and total proctocolectomy.
Furthermore, it was reported that the Xi system’s better fluency is also due to thinner robotic arms that reduce their collisions during surgery and synchronous movements with the operating Table [ 56 ]. In addition, Da Vinci Xi integrates the Indocyanine-Green technology that could be easily used to better identify bile duct during cholecystectomy in patients affected by acute cholecystitis, to assess organ vascularization during their resections and anastomosis, as reported in our experience.
Bianchi et al. [ 61 ] performed an extensive comparison of Da Vinci Si and Xi systems to define their advantages and disadvantages. 89 patients (64 in the Si system vs. 25 in the Xi system group) who underwent liver surgery were included. The Si system group experienced a greater total incisional length (+ 8.99 mm; p < 0.0001) due to a higher number of robotic/laparoscopic ports. Nevertheless, no differences were described regarding operative time, conversion rate, estimated blood loss, postoperative complications, mortality, use of analgesics, and costs. The authors concluded that da Vinci Xi represents an effective technological advancement.
Hill et al. [ 62 ] hypothesized that Da Vinci Xi will allow for greater efficiency and result in shorter operative times if compared to Da Vinci Si. To validate their hypothesis, the authors performed a retrospective review of patients undergoing sigmoid colon resection or Low Anterior Rectal resection. A total of 93 patients underwent sigmoid resection thanks to RS (Si, n = 52 vs. Xi, n = 41). The Xi group had significantly shorter surgical times for Low Anterior Rectal and sigmoid resection (162 vs. 238 min, p = 0.0001). Nowadays, no data are available on the Da Vinci Si and Xi comparison in AES.
However, according to the type of procedures, the mean operative times of Da Vinci Xi were superimposable to the Si group in our experience.
The robotic technology in hemodynamically stable patients could potentially reduce the conversion to open rate (0% in our short series), thanks to high-definition view and accuracy of dissection and fine micro-sutures.
In 2022, the World Society of Emergency Surgery (WSES) published a position paper on RS in AES after the literature evaluation by a steering committee and an international expert panel [ 32 ]. Ten studies (3 case reports, 3 case series, and 4 retrospective comparative cohort articles) were found and 6 statements were proposed. Experts concluded that RS can be considered safe, and feasible in selected cases represented by hemodynamically stable patients. It should be emphasized that the WSES team reported some RS drawbacks: it is mandatory to perform dedicated surgical training, RS showed longer operative times, higher costs and difficult availability and accessibility represent the main issues during night shifts [ 32 ].
These aspects probably may change in the future with RS diffusion and new robotic devices in the health market.
In our experience, the mean age of patients was 63 years. Therefore, more than 30% of patients were older than 70 years (range: 43–88 years) and it is in line with RS literature experiences that showed good outcomes also in the elderly population [ 28 , 41 ]. Nevertheless, operative time represents a crucial point in this frail cohort. Despite RS showing longer operative time when compared to open and laparoscopic surgery, this disadvantage may be offset by lower postoperative complication rates, shorter hospital stays, and lower conversion rates [ 28 , 41 , 63 , 64 , 65 ].
Another key aspect is represented by enhanced vision through near-infrared imaging. It may be useful in AES in case of tissue perfusion evaluations or biliary tree identification in challenging procedures. This feature is not routinely available in laparoscopic surgery [ 66 , 67 ].
Figure 2 shows an emergency scenario due to splenic artery aneurysm repair thanks to RS.
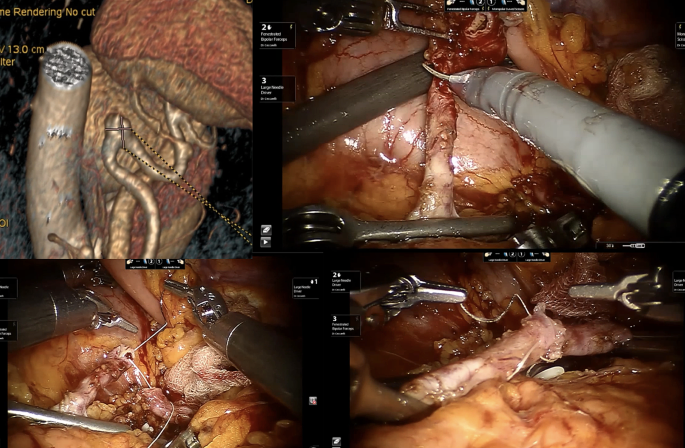
The robotic approach during Emergency Setting for patients affected by splenic artery aneurysms using a vessel resection and end-to-end vascular anastomosis
Robotics in emergency upper-GI and bariatric surgery
One of the earliest studies on RS in AES was published in 2012 [ [ 68 ]]: Sudan et al. experience in complex bariatric surgery involved 2 patients affected by a stomach stricture and an acute abdomen due to perforation with biliary peritonitis after biliopancreatic diversion, respectively. The perforation was treated through an initial laparoscopic investigation followed by a handsewn robotic stitch reparation of duodenal stump dehiscence.
In 2020, Cubas et al. [ 69 ] presented an RS procedure for incarcerated Morgagni Hernia in a 29-year-old male. The hernia defect (reported as 10 × 7 cm) was corrected via mesh placement. Patient discharge was possible on POD 5. No recurrence was detected at 1-year follow-up.
During the same year, Ceccarelli et al. [ 45 ] published a series of 5 patients affected by strangulated Giant Hiatal Hernia: 3 (60%) patients experienced RS while 2 (40%) laparoscopic approach. The authors described an easier incarcerated stomach management thanks to RS, maybe due to better surgeon ergonomic position and more accurate dissection preserving pleural integrity and vagus nerve.
Kim et al. [ 70 ] reported a case of robotic transthoracic repair of a right-sided traumatic diaphragmatic rupture in a 45-year-old male with a history of chronic obstructive pulmonary disease presented as a restrained driver in a low-speed motor vehicle collision. The patient was effectively operated after a 48-hour observation.
In 2021, 300 USA hospitals were involved in retrospective data collection of adult patients affected by Hiatal Hernia and treated in elective and urgent/emergency scenarios from 2015 to 2017 [ 71 ]. Data analysis revealed that laparoscopy (64%) was the most frequent approach used during AES, followed by open surgery (30%). A limited number of patients (6%) experienced RS. After cost evaluations and outcomes analysis, authors declared the technical feasibility of minimally invasive approaches when compared to open surgery due to lower cost, lower length of hospital stay, complications, and mortality.
Robinson et al. [ 72 ], in 2021, performed a statistical analysis of “in-room-to-surgery-start time” in a retrospective cohort study of 44 patients affected by emergent perforated gastrojejunal ulcers. The comparison between RS and laparoscopic (24 and 20 cases respectively) showed encouraging results for RS (25 versus 31 min, p = 0.01). Furthermore, no statistical differences were observed in terms of intra- and post-operative outcomes (operative time, complication rate, complication severity, hospital length of stay, discharge to home, and 30-day readmission). Despite RS showing higher surgical costs, authors concluded that emergency gastric perforation could be safely approached thanks to RS.
No complications were reported in all studies reported in our review [ 69 , 70 , 71 , 72 ].
Robotics in emergency colorectal surgery and appendectomies
Nowadays, emergency laparoscopy represents a safe and valid approach to colorectal disorders such as perforated diverticulitis with generalized peritonitis [ 73 ], iatrogenic colonoscopy perforations [ 74 ], bowel obstructions and anastomotic leaks management [ 75 , 76 , 77 ].
In 2012, Pedraza et al. [ 78 ] showed successful robotic colectomy due to iatrogenic colon perforation following colonoscopy.
Two years later, Felli et al. [ 79 ] described a case of an 86-year-old woman admitted to the emergency unit for massive intestinal bleeding due to ascending colon cancer. After patient resuscitation thanks to blood transfusions, surgeons carried out a robotic right colectomy. The postoperative period was uneventful.
Several series compared laparoscopic and robotic outcomes in patients who underwent elective colorectal surgery [ 80 , 81 , 82 ], suggesting the potential role of RS in this surgical field. Nevertheless, an interesting analysis was performed by Beltzer et al. [ 83 ] in 2019. 106 patients were treated for uncomplicated, complicated, or recurrent diverticulitis. The authors concluded that RS achieves better outcomes when compared to laparoscopic surgery in challenging cases (abscess or relapsing diverticulitis).
Three monocentric experiences reported by Kudsi et al. [ 84 , 85 , 86 ] showed the effectiveness of urgent RS for the treatment of obstructive transverse colon cancer, bleeding sigmoid diverticulosis and caecal volvulus.
However, RS could represent a crucial approach also in colorectal autoimmune diseases. Concerning this field, Anderson et al. [ 87 ] in 2020 reported a matched case-control study of 6 patients treated by urgent subtotal colectomy for ulcerative colitis using the robotic platform. In addition, authors compared patients who underwent RS to laparoscopic urgent procedures (6 versus 13 cases) concluding that no differences in perioperative outcomes were observed.
According to Yang et al. [ 88 ] estimation, more than 17 millions of patients were affected by appendicitis in 2019, making it the most common surgical emergency worldwide. Nevertheless, regarding urgent robotic appendectomies, only 5 literature experiences reported robotic approaches [ 89 , 90 , 91 , 92 , 93 ]. A total of 11 patients were collected and 3 (27.27%) required an appendix stump suture. No complications or conversions were reported. Moreover, Hüttenbrink et al. [ 94 ] described incidental appendicectomy during robotic prostatectomy.
Figure 3 shows our experience during RS for complicated sigmoid diverticulitis with sigmoid-bladder fistula.
Lunardi et al. [ 95 ] presented an interesting analysis of temporal trends in the use of minimally invasive surgery in Abdominal Emergency and Urgent Settings. The authors compared 89,098 emergency colectomies performed between 2013 and 2021. The increase per year for robotic colectomy was 0.9% (from 1.4% of total procedures in 2013 to 8.8% in 2021). As a result of this increase, a 0.7% decrease was registered for the open approach. Furthermore, patients who underwent RS were older, had more comorbidities and had higher BMI when compared to laparoscopic and open groups. Intraoperative outcomes were encouraging for RS: after Propensity Score Matching, a conversion rate of 25.5% (860/3,375 patients) was registered during laparoscopic surgery, while in 11.2% (379/3,375 patients) of RS cases, a conversion to open was required ( p < 0.001). After Propensity Score Marching of patients underwent Emergency surgery only, RS demonstrated advantages in terms of conversion to open (27.5% vs. 12% in laparoscopic and robotic groups respectively, p < 0.001) and post-operative LOS (7.12 vs. 6.85 days respectively, p = 0.001).
In conclusion, conventional open surgery should be recommended for unstable and frail patients who require time-critical surgery. Nevertheless, it could be underlined that stable and frail patients may benefit from an enhanced recovery after surgery associated with RS in the acute setting when compared to open surgery.
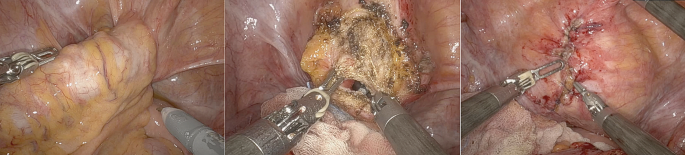
Robotic approach during emergency setting for patients affected by complicated sigmoid diverticulitis with sigmoid-bladder fistula. We performed a fistula resection and bladder suture in double-layer barbed suture
Robotics in acute cholecystitis and biliary tree diseases
Another interesting field of application in AES may be the biliary tree and gallbladder diseases including cholecystitis, Mirizzi syndromes, biliary fistulas, iatrogenic diseases and common bile duct stones.
In 2016, Kubat et al. [ 96 ] published a retrospective series of 150 consecutive robotic single-site cholecystectomies (74 versus 76 cases treated in emergency scenarios and elective settings respectively). The mean operative time for ES cohort was significantly longer (95.0 ± 4.4 versus 71.9 ± 2.6 min; p < 0.001). Both cohorts required 1 conversion to open (1.35% for the emergency group and 1.31% for the elective group). One bile duct injury (0.7%) was reported in patients treated in emergency conditions. The authors concluded that robotic single-site cholecystectomy can be performed safely and effectively in both elective and urgent scenarios with a learning curve of about 48 cases to reach acceptable perioperative outcomes.
Mirizzi syndrome represents one of the most challenging complications of cholelithiasis [ 97 , 98 , 99 ].
In 2014, Lee et al. [ 97 ] evaluated the outcomes of five patients treated by endoscopic biliary stent placement and subsequent robotic partial cholecystectomy due to Mirizzi syndrome. No conversion to open was reported and all patients experienced an uneventful postoperative course.
In 2017 Magge et al. [ 98 ] reported a 6-patient series. All cases were treated performing a combined endoscopic and robotic approaches. In 3 cases (50%) a Roux-en-Y hepatico-jejunostomy was carried out. In these challenging scenarios, RS showed relevant benefits when compared to laparoscopy, facilitating complex dissections, and reducing conversion to open rate.
The most representative cohort of patients was described by Gangemi et al. [ 100 ] in 2017. Authors compared a large series of 676 patients receiving a robotic cholecystectomy with 284 treated by conventional laparoscopy: data analysis showed a significantly lower conversion to open in RS group, especially in patients affected by acute or gangrenous cholecystitis.
A 3-patient experience was described by Milone et al. [ 101 ] in 2019, achieving good perioperative outcomes in acute cholecystitis treatment.
Major bile duct injuries after cholecystectomy require complex surgical repairs that are usually performed with a conventional open approach [ 102 ]. This field may represent an interesting application of RS to safety perform biliary anastomosis. Cubisino et al. presented a systematic review of 13 literature experiences on minimally invasive biliary anastomosis after iatrogenic bile duct injury [ 103 ]. 198 patients were included. 135 patients (63.1%) underwent laparoscopic biliary anastomosis, while 73 (36.1%) received an analogue robotic procedure. According to Strasberg’s classification [ 104 ], all Bile Duct Injuries were types D and E (E1–E5). No conversions occurred in the RS series, while 4 patients required conversion to open surgery among the laparoscopic ones. Postoperative complications were superimposable (18.7% and 19.7% in laparoscopic and robotic approaches, respectively). Nevertheless, the overall reoperation rate was 4.4%, 5.5% in laparoscopic and 2.6% in robotic repairs.
During the follow-up period (median 24.6 months), 9 patients developed an anastomotic stricture: 5 (3.70%) in laparoscopic and 4 (5.48%) in robotic series that required a redo-anastomosis in 60% and 25% respectively.
When compared to open and laparoscopic cholecystectomy in AES, RS showed an increase of 0.7% per year in Lunardi et al. cohort of 793’800 cholecystectomies [ 95 ], ranging from 2.5 to 8.8% between 2013 and 2021. It could be underlined that conversion rate and LOS were statistically lower in RS group ( p < 0.001). Despite these findings, laparoscopic cholecystectomy yet represents the preferred approach in AES.
Robotics emergencies in hernia and abdominal wall surgery
Only a few studies analyzed urgent hernia operations treated using robotic surgery.
In 2020, Bou-Ayash et al. [ 105 ] published a retrospective series of 19 patients (including 23 surgical procedures) affected by inguinal hernia, treated from 2013 to 2020. The authors concluded that the robotic approach represents a safe procedure in selected patients, with a short length of stay and a low complication rate compared to open and laparoscopic surgery.
In 2021, Kudsi et al. [ 106 ] described perioperative outcomes of RS in a 34-patient cohort treated between 2013 and 2019. All patients experienced robotic ventral and incisional hernia repair in an emergency setting. 20% of patients were classified as Clavien-Dindo I or II, while about 11% Clavien-Dindo III and IV. Only 3% of the population experienced a recurrence.
Muysoms et al. [ 107 ] performed an extensive analysis of robotic cost. They retrospective evaluate laparoscopic (272 procedures of which 6 were emergency cases) and robotic (404 procedures of which 8 were emergency cases) inguinal hernia repairs. As reported in other literature experiences, authors concluded that Robotic inguinal hernia repair was significantly ( p < 0.001) more expensive if compared to laparoscopic surgery (mean cost €2612 versus €1963, respectively). Nevertheless, in the robotic group, a larger number of patients were treated as outpatients with lower postoperative complications.
Regarding inguinal and ventral hernia repair, the analysis conducted by Lunardi et al. [ 95 ] showed encouraging data for RS approach: from 2013 to 2021 RS increased of 1.9% per year and 1.1% per year respectively. After propensity score matching, authors reported superimposable data in terms of CCI and BMI, comparing laparoscopic and robotic approaches. Nonetheless, RS showed benefits also in these fields: lower conversion rates were reported both in inguinal hernia repairs (18.1% vs. 3.8%, p < 0.001) and in ventral hernia repair (16.2% vs. 4.8%, p < 0.001). In addition, a statistically significant shorter postoperative LOS was registered in the RS group (the mean LOS in the inguinal hernia group was 3.34 vs. 3 days in laparoscopic and robotic approaches respectively, and the mean LOS in the ventral hernia group was 3.87 vs. 3.73 days, respectively).
Other abdominal emergency surgery and future perspectives
A rare indication for urgent RS was post-traumatic splenic bleeding reported by Giulianotti et al. [ 108 ].
Until now, no reports of RS in adhesive intestinal obstruction have been published.
A possible and useful application of RS is represented by telementoring and telesurgery [ 32 , 109 , 110 , 111 ]. The original aim of RS and the recent COVID-19 pandemic gave an important incentive in these directions. The advantage of telementoring and telepresence of an expert surgeon in a virtual way is nowadays possible and may be improved thanks to the modern and future highspeed internet connection (5G networks) as well as the telesurgery in ultra-remote countries, in low-volume centers and in an emergent civil or battlefield surgical scenarios [ 112 , 113 , 114 ].
The development of new modular robotic platforms may contribute to increase RS applications in emergency settings. Nowadays, several different robotic platforms are approved for human use, such as CMR Versius (Cambridge Medical Robotics, Cambridge, UK), Distalmotion Dexter (Distalmotion, Epalinges, Switzerland) and Medtronic Hugo (Medtronic Inc., Minneapolis, USA). Most of them share the opportunity of switching from a conventional laparoscopic setting to a robot-assisted one.
Limitations
The main bias of our study was represented by hospital organisations: RS devices are available in the same building as the General Surgery Unit at San Donato Hospital (Arezzo, Italy) facilitating emergency surgical procedures. On the other hand, Da Vinci Xi is situated in a separate building specifically dedicated to RS at the General and Robotic Surgery Unit of San Giovanni Battista Hospital (Foligno, Italy).
Furthermore, these findings represented a limit when the surgeons’ team wanted to perform a laparoscopic exploration to validate a minimally invasive robotic approach in emergency scenarios.
In our experience, it should also underline that the COVID-19 era has contributed to limiting RS adoption.
Future shreds of evidence from randomized clinical trials with long-term follow-up are required to define the potential role of RS in AES. Nevertheless, the unavailable data on the cost-effectiveness of RS in AES are linked to lower use of robotic devices if compared to laparoscopic approaches. Our experience suggested that RS costs are superimposable to laparoscopic surgery if we analyse LOS and conversion rate data. To optimize the delivery of robotic technology in AES, a well-coordinated effort among health systems, clinicians, payers, and policymakers and dedicated training program for robotic teams are imperative.
Our study demonstrates that RS may be an useful and reliable approach also to emergency surgical procedures, especially when performed in selected patients in very well trained robotic centers allowing a safe managing of surgical challenging procedures as main indications for this technology, reducing the conversion rate when compared to laparoscopy.
As for laparoscopy the patient selection for robotic approach need hemodinamically stable condition and require a sharing of the surgical strategy by all the team: surgeons, nurses and anaesthesiologists. All the staff need to be trained in laparoscopic and robotic elective surgery, including technology functioning. The hybrid use of robotic/laparoscopic technology may be taken into consideration (a laparoscopic exploration may be the first step) to decide the following approach. The robotic approach may be reserved to challenging steps of the operation (suture/microsuture/dissections).
The availability of the device is the sine qua non condition for emergent and of course urgent use. The current organization in which the platform is shared by different teams, represent for the diffusion of its use in the emergent setting.
The cost reduction of platforms and instruments, together with new robotic devices in the health market, may represent a future perspective for emergencies use of robotic technology. So, the robotic technology may be one of the tools available in every operating theatre, to use in selected cases according to patient condition and surgical team experience.
Data availability
No datasets were generated or analysed during the current study.
Surlin V. Emergency and trauma surgery. Chirurgia (Bucur). 2021;116:643–4.
Article PubMed Google Scholar
E. U. o. M. S. S. o. S. a. E. B. o. Surgery. (2024), vol. 2024.
De Simone B, et al. The new timing in acute care surgery (new TACS) classification: a WSES Delphi consensus study. World J Emerg Surg. 2023;18:32.
Article PubMed PubMed Central Google Scholar
Crepaz L, et al. Minimally invasive approach to incisional hernia in elective and emergency surgery: a SICE (Italian Society of endoscopic surgery and new technologies) and ISHAWS (Italian society of hernia and abdominal wall surgery) online survey. Updates Surg. 2023;75:1671–80.
Coletta D, Patriti A. in Updates Surg . Italy. 2023;75:2047–2048.
Wakabayashi G, et al. Tokyo guidelines 2018: surgical management of acute cholecystitis: safe steps in laparoscopic cholecystectomy for acute cholecystitis (with videos). J Hepatobiliary Pancreat Sci. 2018;25:73–86.
Gorter RR, et al. Diagnosis and management of acute appendicitis. Surg Endosc. 2016;30:4668–90. EAES consensus development conference 2015.
Jara RD, Guerrón AD, Portenier D. Complications of robotic surgery. Surg Clin North Am. 2020;100:461–8.
Rocca A, et al. Robotic surgery for colorectal liver metastases resection: a systematic review. Int J Med Robot. 2021;17:e2330.
Martins RS, et al. Quality of life after robotic versus conventional minimally invasive cancer surgery: a systematic review and meta-analysis. J Robot Surg. 2024;18:171.
Gomez Ruiz M, et al. Robotic surgery for locally advanced T4 rectal cancer: feasibility and oncological quality. Updates Surg. 2023;75:589–97.
Chatterjee S, Das S, Ganguly K, Mandal D. Advancements in robotic surgery: innovations, challenges and future prospects. J Robot Surg. 2024;18:28.
Minamimura K, et al. Current status of robotic gastrointestinal surgery. J Nippon Med Sch. 2023;90:308–15.
Rocca A, et al. Robotic versus open resection for colorectal liver metastases in a referral centre Hub&Spoke learning program. A multicenter propensity score matching analysis of perioperative outcomes. Heliyon. 2024;10:e24800.
Ceccarelli G, et al. Robotic revision surgery after failed Nissen anti-reflux surgery: a single center experience and a literature review. J Robot Surg. 2023;17:1517–24.
Knitter S, et al. Robotic versus laparoscopic versus open major hepatectomy - an analysis of costs and postoperative outcomes in a single-center setting. Langenbecks Arch Surg. 2023;408:214.
Liu R, Liu Q, Wang Z. Worldwide diffusion of robotic approach in general surgery. Updates Surg. 2021;73:795–7.
Daskalaki D, et al. Financial impact of the robotic approach in liver surgery: a comparative study of clinical outcomes and costs between the robotic and open technique in a single institution. J Laparoendosc Adv Surg Tech A. 2017;27:375–82.
de’Angelis N, et al. Robotic versus laparoscopic gastric resection for primary gastrointestinal stromal tumors > 5 cm: a size-matched and location-matched comparison. Surg Laparosc Endosc Percutan Tech. 2017;27:65–71.
van Dam P et al. Are costs of robot-assisted surgery warranted for gynecological procedures? Obstet Gynecol Int. 2011;2011:973830.
Vicente E, Quijano Y, Ferri V, Caruso R. Robot-assisted cholecystectomy with the new HUGO™ robotic-assisted system: first worldwide report with system description, docking settings, and video. Updates Surg. 2023;75:2039–42.
Leal Ghezzi T, Campos Corleta O. 30 years of robotic surgery. World J Surg. 2016;40:2550–7.
Sarkaria IS et al. Early operative outcomes and learning curve of robotic assisted giant paraesophageal hernia repair. Int J Med Robot. 2017;13.
Felder SI, et al. Robotic gastrointestinal surgery. Curr Probl Surg. 2018;55:198–246.
Ceccarelli G et al. Minimally invasive approach to gastric GISTs: analysis of a multicenter robotic and laparoscopic experience with literature review. Cancers (Basel). 2021;13.
Antoniou SA, Antoniou GA, Koch OO, Pointner R, Granderath FA. Robot-assisted laparoscopic surgery of the colon and rectum. Surg Endosc. 2012;26:1–11.
Yeo HL, Isaacs AJ, Abelson JS, Milsom JW, Sedrakyan A. Comparison of open, laparoscopic, and robotic colectomies using a large national database: outcomes and trends related to surgery center volume. Dis Colon Rectum. 2016;59:535–42.
de’Angelis N, et al. Robotic versus laparoscopic colorectal cancer surgery in elderly patients: a propensity score match analysis. J Laparoendosc Adv Surg Tech A. 2018;28:1334–45.
Cheung TT, et al. Robotic versus laparoscopic liver resection for huge (≥ 10 cm) liver tumors: an international multicenter propensity-score matched cohort study of 799 cases. Hepatobiliary Surg Nutr. 2023;12:205–15.
Cillo U, D’Amico FE, Furlanetto A, Perin L, Gringeri E. Robotic hepatectomy and biliary reconstruction for perihilar cholangiocarcinoma: a pioneer western case series. Updates Surg. 2021;73:999–1006.
Giulianotti PC, et al. Robotics in general surgery: personal experience in a large community hospital. Arch Surg. 2003;138:777–84.
de’Angelis N, et al. Robotic surgery in emergency setting: 2021 WSES position paper. World J Emerg Surg. 2022;17:4.
Solaini L, et al. Open versus laparoscopic versus robotic gastric gastrointestinal stromal tumour resections: a multicentre cohort study. Int J Med Robot. 2021;17:e2198.
Wei D, Johnston S, Goldstein L, Nagle D. Minimally invasive colectomy is associated with reduced risk of anastomotic leak and other major perioperative complications and reduced hospital resource utilization as compared with open surgery: a retrospective population-based study of comparative effectiveness and trends of surgical approach. Surg Endosc. 2020;34:610–21.
Giovannetti A, et al. Laparoendoscopic single-site (LESS) versus robotic redo hiatal hernia repair with fundoplication: which approach is better? Am Surg. 2019;85:978–84.
Colvin J, et al. A comparison of robotic versus laparoscopic adrenalectomy in patients with primary hyperaldosteronism. Surg Laparosc Endosc Percutan Tech. 2017;27:391–3.
Tolboom RC, Draaisma WA, Broeders IA. Evaluation of conventional laparoscopic versus robot-assisted laparoscopic redo hiatal hernia and antireflux surgery: a cohort study. J Robot Surg. 2016;10:33–9.
Kim HI, et al. Multicenter prospective comparative study of robotic versus laparoscopic gastrectomy for gastric adenocarcinoma. Ann Surg. 2016;263:103–9.
Vandenbroucke JP, et al. Strengthening the reporting of observational studies in epidemiology (STROBE): explanation and elaboration. Int J Surg. 2014;12:1500–24.
Ceccarelli G, et al. Intraoperative and postoperative outcome of robot-assisted and traditional laparoscopic Nissen fundoplication. Eur Surg Res. 2009;43:198–203.
Article CAS PubMed Google Scholar
Ceccarelli G, et al. Robot-assisted surgery in elderly and very elderly population: our experience in oncologic and general surgery with literature review. Aging Clin Exp Res. 2017;29:55–63.
Ceccarelli G, et al. A new robot-assisted Billroth-I reconstruction: details of the technique and early results. Surg Laparosc Endosc Percutan Tech. 2018;28:e33–9.
Ceccarelli G, et al. Robot-assisted liver surgery in a general surgery unit with a referral centre hub&spoke learning program. Early outcomes after our first 70 consecutive patients. Minerva Chir. 2018;73:460–8.
Ceccarelli G, et al. Robot-assisted Toupet fundoplication and associated cholecystectomy in symptomatic giant hiatal hernia with situs viscerum inversus-A case report and literature review. Int J Surg Case Rep. 2019;60:371–5.
Ceccarelli G, et al. Minimally invasive laparoscopic and robot-assisted emergency treatment of strangulated giant hiatal hernias: report of five cases and literature review. World J Emerg Surg. 2020;15:37.
Ceccarelli G, et al. Minimally invasive robotic-assisted combined colorectal and liver excision surgery: feasibility, safety and surgical technique in a pilot series. Updates Surg. 2021;73:1015–22.
Costa G, et al. Clinico-pathological features of colon cancer patients undergoing emergency surgery: a comparison between elderly and non-elderly patients. Open Med (Wars). 2019;14:726–34.
Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40:373–83.
Owens WD, Felts JA, Spitznagel EL Jr. ASA physical status classifications: a study of consistency of ratings. Anesthesiology. 1978;49:239–43.
Dindo D, Demartines N, Clavien PA. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg. 2004;240:205–13.
Sermonesi G, et al. Cesena guidelines: WSES consensus statement on laparoscopic-first approach to general surgery emergencies and abdominal trauma. World J Emerg Surg. 2023;18:57.
Reinisch A, Liese J, Padberg W, Ulrich F. Robotic operations in urgent general surgery: a systematic review. J Robot Surg. 2023;17:275–90.
Capibaribe DM, Avilez ND, Sacomani CAR, Lucena A, Reis LO. Robotic approach to vesicourethral anastomotic stenosis and resection of remaining prostate after radical prostatectomy. Int Braz J Urol. 2023;49:158–60.
Huser AS, et al. Simulated life-threatening emergency during robot-assisted surgery. J Endourol. 2014;28:717–21.
Ballas DA, Cesta M, Gothard D, Ahmed R. Emergency undocking curriculum in robotic surgery. Cureus. 2019;11:e4321.
PubMed PubMed Central Google Scholar
van der Schans EM, Hiep MAJ, Consten ECJ, Broeders I. From Da Vinci Si to Da Vinci Xi: realistic times in draping and docking the robot. J Robot Surg. 2020;14:835–9.
Alfieri S, et al. Short-term and long-term outcomes after robot-assisted versus laparoscopic distal pancreatectomy for pancreatic neuroendocrine tumors (pNETs): a multicenter comparative study. Langenbecks Arch Surg. 2019;404:459–68.
Abdel Raheem A, et al. Da Vinci Xi and Si platforms have equivalent perioperative outcomes during robot-assisted partial nephrectomy: preliminary experience. J Robot Surg. 2017;11:53–61.
Yuh B, et al. Use of a mobile tower-based robot–the initial Xi robot experience in surgical oncology. J Surg Oncol. 2016;113:5–7.
Hollandsworth HM, et al. Multiquadrant surgery in the robotic era: a technical description and outcomes for Da Vinci Xi robotic subtotal colectomy and total proctocolectomy. Surg Endosc. 2020;34:5153–9.
Bianchi G, et al. Short-term outcomes of Da Vinci Xi versus Si robotic systems for minor hepatectomies. Acta Biomed. 2022;93:e2022223.
Hill A, McCormick J. In experienced hands, does the robotic platform impact operative efficiency? Comparison of the Da Vinci Si versus Xi robot in colorectal surgery. J Robot Surg. 2020;14:789–92.
Oldani A, Bellora P, Monni M, Amato B, Gentilli S. Colorectal surgery in elderly patients: our experience with DaVinci Xi ® system. Aging Clin Exp Res. 2017;29:91–9.
Gallotta V, et al. Robotic surgery in elderly and very elderly gynecologic cancer patients. J Minim Invasive Gynecol. 2018;25:872–7.
Buchs NC, et al. Safety of robotic general surgery in elderly patients. J Robot Surg. 2010;4:91–8.
Barberio M, et al. Quantitative fluorescence angiography versus hyperspectral imaging to assess bowel ischemia: a comparative study in enhanced reality. Surgery. 2020;168:178–84.
Liot E, et al. Does near-infrared (NIR) fluorescence angiography modify operative strategy during emergency procedures? Surg Endosc. 2018;32:4351–6.
Sudan R, Desai SS. Emergency and weekend robotic surgery are feasible. J Robot Surg. 2012;6:263–6.
Cubas R, Garcia M, Mukherjee K. Robotic repair of incarcerated morgagni hernia in an adult on the acute care surgery service. Rev Fac Cien Med Univ Nac Cordoba. 2021;78:91–4.
Kim JK, Desai A, Kunac A, Merchant AM, Lovoulos C. Robotic Transthoracic Repair of a Right-Sided Traumatic Diaphragmatic Rupture. Surg J (N Y). 2020;6(3):e164–e166.
Hosein S, Carlson T, Flores L, Armijo PR, Oleynikov D. Minimally invasive approach to hiatal hernia repair is superior to open, even in the emergent setting: a large national database analysis. Surg Endosc. 2021;35:423–8.
Robinson TD, et al. Emergent robotic versus laparoscopic surgery for perforated gastrojejunal ulcers: a retrospective cohort study of 44 patients. Surg Endosc. 2022;36:1573–7.
Sartelli M, et al. 2020 update of the WSES guidelines for the management of acute colonic diverticulitis in the emergency setting. World J Emerg Surg. 2020;15:32.
de’Angelis N, et al. 2017 WSES guidelines for the management of iatrogenic colonoscopy perforation. World J Emerg Surg. 2018;13:5.
Marano A, Giuffrida MC, Giraudo G, Pellegrino L, Borghi F. Management of peritonitis after minimally invasive colorectal surgery: can we stick to laparoscopy? J Laparoendosc Adv Surg Tech A. 2017;27:342–7.
Wind J, et al. Laparoscopic reintervention for anastomotic leakage after primary laparoscopic colorectal surgery. Br J Surg. 2007;94:1562–6.
Vennix S, et al. Emergency laparoscopic sigmoidectomy for perforated diverticulitis with generalised peritonitis: a systematic review. Dig Surg. 2016;33:1–7.
Pedraza R, Ragupathi M, Martinez T, Haas EM. Robotic-assisted laparoscopic primary repair of acute iatrogenic colonic perforation: case report. Int J Med Robot. 2012;8:375–8.
Felli E, et al. Robotic right colectomy for hemorrhagic right colon cancer: a case report and review of the literature of minimally invasive urgent colectomy. World J Emerg Surg. 2014;9:32.
Chen ZL, Du QL, Zhu YB, Wang HF. A systematic review and meta-analysis of short-term outcomes comparing the efficacy of robotic versus laparoscopic colorectal surgery in obese patients. J Robot Surg. 2024;18:167.
Alkhamis A, et al. Outcomes in robotic-assisted compared to laparoscopic-assisted colorectal surgery in a newly established colorectal tertiary center: a retrospective comparative cohort study. J Robot Surg. 2024;18:152.
de Almeida Leite RM et al. Surgical and medical outcomes in robotic compared to laparoscopic colectomy global prospective cohort from the American college of surgeons national surgical quality improvement program. Surg Endosc. 2024.
Beltzer C, et al. Robotic versus laparoscopic sigmoid resection for diverticular disease: a single-center experience of 106 cases. J Laparoendosc Adv Surg Tech A. 2019;29:1451–5.
Kudsi OY, Gokcal F. Urgent robotic mesocolic excision for obstructing proximal transverse colon cancer - a video vignette. Colorectal Dis. 2019;21:1093–4.
Kudsi OY, Bou-Ayash N. Bleeding sigmoid diverticulosis - urgent stapleless totally robotic sigmoidectomy-a video vignette. Colorectal Dis. 2020;22:1205.
Kudsi OY, Bou-Ayash N. Caecal volvulus - urgent totally robotic right colectomy - a video vignette. Colorectal Dis. 2020;22:1448–9.
Anderson M, et al. Early experience with urgent robotic subtotal colectomy for severe acute ulcerative colitis has comparable perioperative outcomes to laparoscopic surgery. J Robot Surg. 2020;14:249–53.
Yang Y, et al. The global burden of appendicitis in 204 countries and territories from 1990 to 2019. Clin Epidemiol. 2022;14:1487–99.
Cadière GB, et al. Feasibility of robotic laparoscopic surgery: 146 cases. World J Surg. 2001;25:1467–77.
Kelkar D, Borse MA, Godbole GP, Kurlekar U, Slack M. Interim safety analysis of the first-in-human clinical trial of the versius surgical system, a new robot-assisted device for use in minimal access surgery. Surg Endosc. 2021;35:5193–202.
Kibar Y, Yalcin S, Kopru B, Kaya E, Topuz B, Ebiloglu T. Robot-Assisted Laparoscopic Repair of Spontaneous Appendicovesical Fistula. J Endourol Case Rep. 2016;2(1):111–3.
Yi B, et al. The first clinical use of domestically produced Chinese minimally invasive surgical robot system micro hand S. Surg Endosc. 2016;30:2649–55.
Yi B, et al. Domestically produced Chinese minimally invasive surgical robot system micro hand S is applied to clinical surgery preliminarily in China. Surg Endosc. 2017;31:487–93.
Hüttenbrink C, et al. Incidental appendectomy during robotic laparoscopic prostatectomy-safe and worth to perform? Langenbecks Arch Surg. 2018;403:265–9.
PubMed Google Scholar
Lunardi N, et al. Robotic technology in emergency general surgery cases in the era of minimally invasive surgery. JAMA Surg. 2024;159:493–9.
Kubat E, Hansen N, Nguyen H, Wren SM, Eisenberg D. Urgent and elective robotic single-site cholecystectomy: analysis and learning curve of 150 consecutive cases. J Laparoendosc Adv Surg Tech A. 2016;26:185–91.
Lee KF, et al. A minimally invasive strategy for Mirizzi syndrome: the combined endoscopic and robotic approach. Surg Endosc. 2014;28:2690–4.
Magge D, et al. Performing the difficult cholecystectomy using combined endoscopic and robotic techniques: how I do it. J Gastrointest Surg. 2017;21:583–9.
Valderrama-Treviño AI, et al. Updates in Mirizzi syndrome. Hepatobiliary Surg Nutr. 2017;6:170–8.
Gangemi A, Danilkowicz R, Bianco F, Masrur M, Giulianotti PC. Risk factors for open conversion in minimally invasive cholecystectomy. Jsls. 2017;21.
Milone M, et al. Robotic cholecystectomy for acute cholecystitis: three case reports. Med (Baltim). 2019;98:e16010.
Article CAS Google Scholar
Giuliante F, et al. Bile duct injury after cholecystectomy: timing of surgical repair should be based on clinical presentation. The experience of a tertiary referral center with Hepp-Couinaud hepatico-jejunostomy. Updates Surg. 2023;75:1509–17.
Cubisino A, Dreifuss NH, Cassese G, Bianco FM, Panaro F. Minimally invasive biliary anastomosis after iatrogenic bile duct injury: a systematic review. Updates Surg. 2023;75:31–9.
Strasberg SM, Hertl M, Soper NJ. An analysis of the problem of biliary injury during laparoscopic cholecystectomy. J Am Coll Surg. 1995;180:101–25.
CAS PubMed Google Scholar
Bou-Ayash N, Gokcal F, Kudsi OY. Robotic inguinal hernia repair for incarcerated hernias. J Laparoendosc Adv Surg Tech A. 2021;31:926–30.
Kudsi OY, Bou-Ayash N, Chang K, Gokcal F. Perioperative and midterm outcomes of emergent robotic repair of incarcerated ventral and incisional hernia. J Robot Surg. 2021;15:473–81.
Muysoms F et al. Economic assessment of starting robot-assisted laparoscopic inguinal hernia repair in a single-centre retrospective comparative study: the EASTER study. BJS Open. 2021;5.
Giulianotti PC, et al. Robot-assisted treatment of splenic artery aneurysms. Ann Vasc Surg. 2011;25:377–83.
Smith AL, et al. Dual-console robotic surgery: a new teaching paradigm. J Robot Surg. 2013;7:113–8.
Thomas A, et al. Effective implementation and adaptation of structured robotic colorectal programme in a busy tertiary unit. J Robot Surg. 2021;15:731–9.
Panteleimonitis S, et al. Implementation of robotic rectal surgery training programme: importance of standardisation and structured training. Langenbecks Arch Surg. 2018;403:749–60.
Zheng J, et al. 5G ultra-remote robot-assisted laparoscopic surgery in China. Surg Endosc. 2020;34:5172–80.
Mohan A, Wara UU, Arshad Shaikh MT, Rahman RM, Zaidi ZA. Telesurgery and robotics: an improved and efficient era. Cureus. 2021;13:e14124.
Anvari M, Manoharan B, Barlow K. From telementorship to automation. J Surg Oncol. 2021;124:246–9.
Giulianotti PC, Quadri P, Durgam S, Bianco FM. Reconstruction/repair of iatrogenic biliary injuries: is the robot offering a new option? Short clinical report. Ann Surg. 2018;267:e7–9.
Cuendis-Velázquez A, et al. A new era of bile duct repair: robotic-assisted versus laparoscopic hepaticojejunostomy. J Gastrointest Surg. 2019;23:451–9.
Marino MV, Mirabella A, Guarrasi D, Lupo M, Komorowski AL. Robotic-assisted repair of iatrogenic common bile duct injury after laparoscopic cholecystectomy: surgical technique and outcomes. Int J Med Robot. 2019;15:e1992.
Sucandy I, et al. Robotic versus open extrahepatic biliary reconstruction for iatrogenic bile duct injury. Am Surg. 2022;88:345–7.
D’Hondt M, Wicherts DA. Robotic biliary surgery for benign and malignant bile duct obstruction: a case series. J Robot Surg. 2023;17:55–62.
Download references
This research received no specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and affiliations.
Department of General Surgery, “San Giovanni Battista” Hospital, USL Umbria 2, Foligno, Perugia, Italy
Graziano Ceccarelli, Fabio Rondelli & Michele De Rosa
Division of General Surgery, Bufalini Hospital, Cesena, Italy
Fausto Catena
Department of General Surgery and Hepatobiliary and Pancreatic Surgery Unit, Pineta Grande Hospital, Castel Volturno, Caserta, Italy
Pasquale Avella & Aldo Rocca
Department of Medicine and Health Science “V. Tiberio”, University of Molise, Campobasso, Italy
Pasquale Avella, Germano Guerra & Aldo Rocca
Department of General Surgery, Singapore General Hospital, Singapore, Singapore
Brian WCA Tian
You can also search for this author in PubMed Google Scholar
Contributions
G.C.: study conception and design, literature search, data acquisition, interpretation and analysis; drafting and critically revising the article for important intellectual content; final approval of the version to be published. P.A.: literature search, data acquisition, interpretation and analysis; drafting and critically revising the article for important intellectual content; final approval of the version to be published. F.C.: drafting and critically revising the article for important intellectual content; final approval of the version to be published. B.W.T.: data acquisition, interpretation and analysis; final approval of the version to be published. F.R.: study conception and design, literature search, data acquisition, interpretation and analysis; final approval of the version to be published. All authors: data acquisition, interpretation, and analysis; final approval of the version to be published. A.R.: supervision, drafted and critically revised the article for important intellectual content; final approval of the version to be published.
Corresponding author
Correspondence to Pasquale Avella .
Ethics declarations
Human ethics and consent to participate.
The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. An informed consent for treating personal and sensible data was obtained from all patients before the data collection and evaluation. The study was conducted according to the guidelines of the Declaration of Helsinki and approved by the Institutional Review Board of the University of Molise (protocol number 10/21, approved date: May 12, 2021).
Consent to publish
Patients signed informed consent regarding publishing their data and photographs.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Ceccarelli, G., Catena, F., Avella, P. et al. Emergency robotic surgery: the experience of a single center and review of the literature. World J Emerg Surg 19 , 28 (2024). https://doi.org/10.1186/s13017-024-00555-6
Download citation
Received : 14 May 2024
Accepted : 22 July 2024
Published : 17 August 2024
DOI : https://doi.org/10.1186/s13017-024-00555-6
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Abdominal emergency surgery
- Urgent robotic surgery
- Minimally invasive surgery
- Learning curve
- Complicated diverticulitis
- Emergency setting
World Journal of Emergency Surgery
ISSN: 1749-7922
- Submission enquiries: [email protected]
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Perspect Med Educ
- v.7(1); 2018 Feb

Writing an effective literature review
Lorelei lingard.
Schulich School of Medicine & Dentistry, Health Sciences Addition, Western University, London, Ontario Canada
In the Writer’s Craft section we offer simple tips to improve your writing in one of three areas: Energy, Clarity and Persuasiveness. Each entry focuses on a key writing feature or strategy, illustrates how it commonly goes wrong, teaches the grammatical underpinnings necessary to understand it and offers suggestions to wield it effectively. We encourage readers to share comments on or suggestions for this section on Twitter, using the hashtag: #how’syourwriting?
This Writer’s Craft instalment is the first in a two-part series that offers strategies for effectively presenting the literature review section of a research manuscript. This piece alerts writers to the importance of not only summarizing what is known but also identifying precisely what is not, in order to explicitly signal the relevance of their research. In this instalment, I will introduce readers to the mapping the gap metaphor, the knowledge claims heuristic, and the need to characterize the gap.
Mapping the gap
The purpose of the literature review section of a manuscript is not to report what is known about your topic. The purpose is to identify what remains unknown— what academic writing scholar Janet Giltrow has called the ‘knowledge deficit’ — thus establishing the need for your research study [ 1 ]. In an earlier Writer’s Craft instalment, the Problem-Gap-Hook heuristic was introduced as a way of opening your paper with a clear statement of the problem that your work grapples with, the gap in our current knowledge about that problem, and the reason the gap matters [ 2 ]. This article explains how to use the literature review section of your paper to build and characterize the Gap claim in your Problem-Gap-Hook. The metaphor of ‘mapping the gap’ is a way of thinking about how to select and arrange your review of the existing literature so that readers can recognize why your research needed to be done, and why its results constitute a meaningful advance on what was already known about the topic.
Many writers have learned that the literature review should describe what is known. The trouble with this approach is that it can produce a laundry list of facts-in-the-world that does not persuade the reader that the current study is a necessary next step. Instead, think of your literature review as painting in a map of your research domain: as you review existing knowledge, you are painting in sections of the map, but your goal is not to end with the whole map fully painted. That would mean there is nothing more we need to know about the topic, and that leaves no room for your research. What you want to end up with is a map in which painted sections surround and emphasize a white space, a gap in what is known that matters. Conceptualizing your literature review this way helps to ensure that it achieves its dual goal: of presenting what is known and pointing out what is not—the latter of these goals is necessary for your literature review to establish the necessity and importance of the research you are about to describe in the methods section which will immediately follow the literature review.
To a novice researcher or graduate student, this may seem counterintuitive. Hopefully you have invested significant time in reading the existing literature, and you are understandably keen to demonstrate that you’ve read everything ever published about your topic! Be careful, though, not to use the literature review section to regurgitate all of your reading in manuscript form. For one thing, it creates a laundry list of facts that makes for horrible reading. But there are three other reasons for avoiding this approach. First, you don’t have the space. In published medical education research papers, the literature review is quite short, ranging from a few paragraphs to a few pages, so you can’t summarize everything you’ve read. Second, you’re preaching to the converted. If you approach your paper as a contribution to an ongoing scholarly conversation,[ 2 ] then your literature review should summarize just the aspects of that conversation that are required to situate your conversational turn as informed and relevant. Third, the key to relevance is to point to a gap in what is known. To do so, you summarize what is known for the express purpose of identifying what is not known . Seen this way, the literature review should exert a gravitational pull on the reader, leading them inexorably to the white space on the map of knowledge you’ve painted for them. That white space is the space that your research fills.
Knowledge claims
To help writers move beyond the laundry list, the notion of ‘knowledge claims’ can be useful. A knowledge claim is a way of presenting the growing understanding of the community of researchers who have been exploring your topic. These are not disembodied facts, but rather incremental insights that some in the field may agree with and some may not, depending on their different methodological and disciplinary approaches to the topic. Treating the literature review as a story of the knowledge claims being made by researchers in the field can help writers with one of the most sophisticated aspects of a literature review—locating the knowledge being reviewed. Where does it come from? What is debated? How do different methodologies influence the knowledge being accumulated? And so on.
Consider this example of the knowledge claims (KC), Gap and Hook for the literature review section of a research paper on distributed healthcare teamwork:
KC: We know that poor team communication can cause errors. KC: And we know that team training can be effective in improving team communication. KC: This knowledge has prompted a push to incorporate teamwork training principles into health professions education curricula. KC: However, most of what we know about team training research has come from research with co-located teams—i. e., teams whose members work together in time and space. Gap: Little is known about how teamwork training principles would apply in distributed teams, whose members work asynchronously and are spread across different locations. Hook: Given that much healthcare teamwork is distributed rather than co-located, our curricula will be severely lacking until we create refined teamwork training principles that reflect distributed as well as co-located work contexts.
The ‘We know that …’ structure illustrated in this example is a template for helping you draft and organize. In your final version, your knowledge claims will be expressed with more sophistication. For instance, ‘We know that poor team communication can cause errors’ will become something like ‘Over a decade of patient safety research has demonstrated that poor team communication is the dominant cause of medical errors.’ This simple template of knowledge claims, though, provides an outline for the paragraphs in your literature review, each of which will provide detailed evidence to illustrate a knowledge claim. Using this approach, the order of the paragraphs in the literature review is strategic and persuasive, leading the reader to the gap claim that positions the relevance of the current study. To expand your vocabulary for creating such knowledge claims, linking them logically and positioning yourself amid them, I highly recommend Graff and Birkenstein’s little handbook of ‘templates’ [ 3 ].
As you organize your knowledge claims, you will also want to consider whether you are trying to map the gap in a well-studied field, or a relatively understudied one. The rhetorical challenge is different in each case. In a well-studied field, like professionalism in medical education, you must make a strong, explicit case for the existence of a gap. Readers may come to your paper tired of hearing about this topic and tempted to think we can’t possibly need more knowledge about it. Listing the knowledge claims can help you organize them most effectively and determine which pieces of knowledge may be unnecessary to map the white space your research attempts to fill. This does not mean that you leave out relevant information: your literature review must still be accurate. But, since you will not be able to include everything, selecting carefully among the possible knowledge claims is essential to producing a coherent, well-argued literature review.
Characterizing the gap
Once you’ve identified the gap, your literature review must characterize it. What kind of gap have you found? There are many ways to characterize a gap, but some of the more common include:
- a pure knowledge deficit—‘no one has looked at the relationship between longitudinal integrated clerkships and medical student abuse’
- a shortcoming in the scholarship, often due to philosophical or methodological tendencies and oversights—‘scholars have interpreted x from a cognitivist perspective, but ignored the humanist perspective’ or ‘to date, we have surveyed the frequency of medical errors committed by residents, but we have not explored their subjective experience of such errors’
- a controversy—‘scholars disagree on the definition of professionalism in medicine …’
- a pervasive and unproven assumption—‘the theme of technological heroism—technology will solve what ails teamwork—is ubiquitous in the literature, but what is that belief based on?’
To characterize the kind of gap, you need to know the literature thoroughly. That means more than understanding each paper individually; you also need to be placing each paper in relation to others. This may require changing your note-taking technique while you’re reading; take notes on what each paper contributes to knowledge, but also on how it relates to other papers you’ve read, and what it suggests about the kind of gap that is emerging.
In summary, think of your literature review as mapping the gap rather than simply summarizing the known. And pay attention to characterizing the kind of gap you’ve mapped. This strategy can help to make your literature review into a compelling argument rather than a list of facts. It can remind you of the danger of describing so fully what is known that the reader is left with the sense that there is no pressing need to know more. And it can help you to establish a coherence between the kind of gap you’ve identified and the study methodology you will use to fill it.
Acknowledgements
Thanks to Mark Goldszmidt for his feedback on an early version of this manuscript.
PhD, is director of the Centre for Education Research & Innovation at Schulich School of Medicine & Dentistry, and professor for the Department of Medicine at Western University in London, Ontario, Canada.
Information
- Author Services
Initiatives
You are accessing a machine-readable page. In order to be human-readable, please install an RSS reader.
All articles published by MDPI are made immediately available worldwide under an open access license. No special permission is required to reuse all or part of the article published by MDPI, including figures and tables. For articles published under an open access Creative Common CC BY license, any part of the article may be reused without permission provided that the original article is clearly cited. For more information, please refer to https://www.mdpi.com/openaccess .
Feature papers represent the most advanced research with significant potential for high impact in the field. A Feature Paper should be a substantial original Article that involves several techniques or approaches, provides an outlook for future research directions and describes possible research applications.
Feature papers are submitted upon individual invitation or recommendation by the scientific editors and must receive positive feedback from the reviewers.
Editor’s Choice articles are based on recommendations by the scientific editors of MDPI journals from around the world. Editors select a small number of articles recently published in the journal that they believe will be particularly interesting to readers, or important in the respective research area. The aim is to provide a snapshot of some of the most exciting work published in the various research areas of the journal.
Original Submission Date Received: .
- Active Journals
- Find a Journal
- Proceedings Series
- For Authors
- For Reviewers
- For Editors
- For Librarians
- For Publishers
- For Societies
- For Conference Organizers
- Open Access Policy
- Institutional Open Access Program
- Special Issues Guidelines
- Editorial Process
- Research and Publication Ethics
- Article Processing Charges
- Testimonials
- Preprints.org
- SciProfiles
- Encyclopedia

Article Menu

- Subscribe SciFeed
- Recommended Articles
- Google Scholar
- on Google Scholar
- Table of Contents
Find support for a specific problem in the support section of our website.
Please let us know what you think of our products and services.
Visit our dedicated information section to learn more about MDPI.
JSmol Viewer
Strengthening akis for sustainable agricultural features: insights and innovations from the european union: a literature review.

1. Introduction
2. materials and methods, 2.1. data collection procedure, 2.2. identification criteria, 2.3. screening and selection criteria, 2.4. eligibility and inclusion criteria.
- The studies that were carried out or considered the 28 countries in the European Union (including the United Kingdom until 2019 and excluding Romania).
- Studies published in the English Language.
- Studies that were published within the past 11 years (the review covers the period from 2014 to 2024, a period in which the two previous Programming Periods of the Common Agricultural Policy were implemented).
- Studies covering the inclusion of a transparent description of the process of data acquisition and interpretation.
- Studies covering a primary or secondary class investigation on the subject matter.
- Studies showcasing the effects of AKISs and FASs on agricultural knowledge advancement.
- Studies published in a non-English language.
- Studies carried out outside the EU.
- Studies with unclear methodology of data collection and analysis.
- Studies lacking author names and affiliation.
- Studies not covering both the main issues of this review (i.e., AKIS and FAS).
4. Discussion
4.1. akis and fas in the foreground through the new cap, 4.2. improving the effectiveness of an akis, 5. conclusions, author contributions, institutional review board statement, data availability statement, conflicts of interest.
- Kuiper, D.; Roling, N.G. Proceedings of the European Seminar on Knowledge Management and Information Technology ; Wageningen Agricultural University: Wageningen, The Netherlands, 1991; pp. 8–20. [ Google Scholar ]
- Hermans, F.; Geerling-Eiff, F.; Potters, J.; Klerkx, L. Public-private partnerships as systemic agricultural innovation policy instruments—Assessing their contribution to innovation system function dynamics. NJAS Wagening. J. Life Sci. 2019 , 88 , 76–95. [ Google Scholar ] [ CrossRef ]
- European Union Standing Committee on Agricultural Research (EU SCAR). Agricultural Knowledge and Innovation Systems in Transition—A Reflection Paper ; European Commission: Brussels, Belgium, 2012. [ Google Scholar ]
- Labarthe, P.; Beck, M. CAP and Advisory Services: From Farm Advisory Systems to Innovation Support. EuroChoices 2022 , 21 , 5–14. [ Google Scholar ] [ CrossRef ]
- Kiraly, G.; Vago, S.; Bull, E.; Van der Cruyssen, L.; Arbour, T.; Spanoghe, P.; Van Dijk, L. Information behaviour of farmers, foresters, and advisors in the context of digitalisation in the EU. Stud. Agric. Econ. 2023 , 125 , 1–12. [ Google Scholar ] [ CrossRef ]
- Ingram, J.; Mills, J. Are advisory services “fit for purpose” to support sustainable soil management? An assessment of advice in Europe. Soil Use Manag. 2019 , 35 , 21–31. [ Google Scholar ] [ CrossRef ]
- Laurent, C.; Nguyen, G.; Triboulet, P.; Ansaloni, M.; Bechtet, N.; Labarthe, P. Institutional continuity and hidden changes in farm advisory services provision: Evidence from farmers’ microAKIS observations in France. J. Agric. Educ. Ext. 2021 , 28 , 601–624. [ Google Scholar ] [ CrossRef ]
- Madureira, L.; Labarthe, P.; Marues, C.S.; Santos, G. Exploring micro AKIS: Farmer-centric evidence on the role of advice in agricultural innovation in Europe. J. Agric. Educ. Ext. 2022 , 28 , 549–575. [ Google Scholar ] [ CrossRef ]
- Amerani, E.; Michailidis, A. The Agricultural Knowledge and Innovation System (AKIS) in a Changing Environment in Greece. In Proceedings of the 17th International Conference of the Hellenic Association of Agricultural Economists, Thessaloniki, Greece, 2–3 November 2023. [ Google Scholar ] [ CrossRef ]
- Kiljunen, J.; Jaakkola, D. AKIS and Advisory Services in Finland. Report for the AKIS Inventory (Task 1.2) of the i2connect Project. i2connect INTERACTIVE INNOVATION 2020. Available online: https://i2connect-h2020.eu/resources/akis-country-reports/ (accessed on 29 January 2024).
- Charatsari, C.; Michailidis, A.; Francescone, M.; De Rosa, M.; Aidonis, D.; Bartoli, L.; La Rocca, G.; Camanzi, L.; Lioutas, E.D. Do Agricultural Knowledge and Innovation Systems Have the Dynamic Capabilities to Guide the Digital Transition of Short Food Supply Chains? Information 2024 , 15 , 22. [ Google Scholar ] [ CrossRef ]
- Masi, M.; De Rosa, M.; Vecchio, Y.; Adinolfi, F. The long way to innovation adoption: Insights from precision agriculture. Agric. Food Econ. 2022 , 10 , 27. [ Google Scholar ] [ CrossRef ]
- Nordlund, I.; Norrby, T. AKIS and advisory services in Sweden. Report for the AKIS Inventory (Task 1.2) of the i2connect Project. i2connect INTERACTIVE INNOVATION 2021. Available online: https://i2connect-h2020.eu/resources/akis-country-reports/ (accessed on 5 February 2024).
- Sturel, S. AKIS and Advisory Services in France. Report for the AKIS Inventory (Task 1.2) of the i2connect Project. i2connect INTERACTIVE INNOVATION 2021. Available online: https://i2connect-h2020.eu/resources/akis-country-reports/ (accessed on 30 January 2024).
- Enfedaque Diaz, L.; Jimenez Gonzalez, A.; Pures Pato, M.A. AKIS and advisory services in Spain. Report for the AKIS inventory (Task 1.2) of the i2connect Project. i2connect INTERACTIVE INNOVATION 2020. Available online: https://i2connect-h2020.eu/resources/akis-country-reports/ (accessed on 5 February 2024).
- Almeida, R.; Viveiros, F. AKIS and Advisory Services in Portugal. Report for the AKIS Inventory (Task 1.2) of the i2connect Project. i2connect INTERACTIVE INNOVATION 2020. Available online: https://i2connect-h2020.eu/resources/akis-country-reports/ (accessed on 3 February 2024).
- Birke, F.; Bae, S.; Schober Gerster-Bentaya, M.; Knierim, A.; Asensio, P.; Kolbeck, M.; Ketelhodt, C. AKIS and Advisory Services in Germany. Report for the AKIS Inventory (Task 1.2) of the i2connect Project. i2connect INTERACTIVE INNOVATION 2021. Available online: https://i2connect-h2020.eu/resources/akis-country-reports/ (accessed on 30 January 2024).
- Jelakovic, K. AKIS and Advisory Services in Croatia. Report for the AKIS Inventory (Task 1.2) of the i2connect Project. i2connect INTERACTIVE INNOVATION 2021. Available online: https://i2connect-h2020.eu/resources/akis-country-reports/ (accessed on 28 January 2024).
- Stankovic, S. AKIS and Advisory Services in Serbia. Report for the AKIS Inventory (Task 1.2) of the i2connect Project. i2connect INTERACTIVE INNOVATION 2020. Available online: https://i2connect-h2020.eu/resources/akis-country-reports/ (accessed on 4 February 2024).
- Hrovatic, I. AKIS and Advisory Services in Slovenia. Report for the AKIS Inventory (Task 1.2) of the i2connect Project. i2connect INTERACTIVE INNOVATION 2020. Available online: https://i2connect-h2020.eu/resources/akis-country-reports/ (accessed on 4 February 2024).
- Bachev, H. Governance of Agricultural Knowledge and Innovation System (AKIS) in Bulgaria. SSRN Electron. J. 2022 . [ Google Scholar ] [ CrossRef ]
- Koutsouris, A.; Zarokosta, E.; Kanaki, V. AKIS and Advisory Services in Cyprus. Report for the AKIS inventory (Task 1.2) of the i2connect Project. i2connect INTERACTIVE INNOVATION 2020. Available online: https://i2connect-h2020.eu/resources/akis-country-reports/ (accessed on 28 January 2024).
- Knierim, A.; Kernecker, M.; Erdle, K.; Kraus, T.; Borges, F.; Wurbs, A. Smart farming technology innovations—Insights and reflections from the German Smart-AKIS hub. NJAS Wagening. J. Life Sci. 2019 , 90–91 , 1–10. [ Google Scholar ] [ CrossRef ]
- Koutsouris, A.; Zarokosta, E.; Pappa, E.; Kanaki, V. AKIS and Advisory Services in Greece. Report for the AKIS Inventory (Task 1.2) of the i2connect Project. i2connect INTERACTIVE INNOVATION 2020. Available online: https://i2connect-h2020.eu/resources/akis-country-reports/ (accessed on 30 January 2024).
- Coquil, X.; Cerf, M.; Auricoste, C.; Joannon, A.; Barcellini, F.; Cayre, P.; Chizallet, M.; Dedieu, B.; Hostiou, N.; Hellec, F.; et al. Questioning the work of farmers, advisors, teachers and researchers in agro-ecological transition. A review. Agron. Sustain. Dev. 2018 , 38 , 47. [ Google Scholar ] [ CrossRef ]
- Lybaert, C.; Debruyne, L. AKIS and Advisory Services in Belgium. Report for the AKIS Inventory (Task 1.2) of the i2connect Project. i2connect INTERACTIVE INNOVATION 2020. Available online: https://i2connect-h2020.eu/resources/akis-country-reports/ (accessed on 27 January 2024).
- Dortmans, E.; Van Geel, D.; Van der Velde, S. AKIS and Advisory Services in Netherlands. Report for the AKIS Inventory (Task 1.2) of the i2connect Project. i2connect INTERACTIVE INNOVATION 2020. Available online: https://i2connect-h2020.eu/resources/akis-country-reports/ (accessed on 2 February 2024).
- Gaborne, J.A.; Varga, Z.; Ver, A. AKIS and Advisory Services in Hungary. Report for the AKIS inventory (Task 1.2) of the i2connect Project. i2connect INTERACTIVE INNOVATION 2020. Available online: https://i2connect-h2020.eu/resources/akis-country-reports/ (accessed on 31 January 2024).
- de Foliveira, M.; Gomes da Silva, F.; Ferreira, S.; Teixeira, M.; Damαsio, H.; Ferreira, A.D.; Gonηalves, J.M. Innovations in Sustainable Agriculture: Case Study of Lis Valley Irrigation District, Portugal. Sustainability 2019 , 11 , 331. [ Google Scholar ] [ CrossRef ]
- Mirra, L.; Caputo, N.; Gandolfi, F.; Menna, C. The Agricultural Knowledge and Innovation System (AKIS) in Campania Region: The challenges facing the first implementation of experimental model. J. Agric. Policy 2020 , 3 , 35–44. [ Google Scholar ] [ CrossRef ]
- Cristiano, S.; Carta, V.; Sturla, V.; D’Oronzio, M.A.; Proietti, P. AKIS and Advisory Services in Italy. Report for the AKIS Inventory (Task 1.2) of the i2connect Project. i2connect INTERACTIVE INNOVATION 2020. Available online: https://i2connect-h2020.eu/resources/akis-country-reports/ (accessed on 31 January 2024).
- Todorova, I. AKIS and Advisory Services in Bulgaria. Report for the AKIS Inventory (Task 1.2) of the i2connect Project. i2connect INTERACTIVE INNOVATION 2021. Available online: https://i2connect-h2020.eu/resources/akis-country-reports/ (accessed on 27 January 2024).
- Dzelme, A.; Zurins, K. AKIS and Advisory Services in Latvia. Report for the AKIS inventory (Task 1.2) of the i2connect Project. i2connect INTERACTIVE INNOVATION 2021. Available online: https://i2connect-h2020.eu/resources/akis-country-reports/ (accessed on 1 February 2024).
- Matuseviciute, E.; Petraitis, R.; Sakickiene, A.; Titiskyte, L.; Urbanaviciene, S. AKIS and Advisory Services in Lithuania. Report for the AKIS Inventory (Task 1.2) of the i2connect Project. i2connect INTERACTIVE INNOVATION 2021. Available online: https://i2connect-h2020.eu/resources/akis-country-reports/ (accessed on 1 February 2024).
- Zimmer, S.; Stoll, E.; Leimbrock-Rosch, L. AKIS and Advisory Services in Luxembourg. Report for the AKIS Inventory (Task 1.2) of the i2connect Project. i2connect INTERACTIVE INNOVATION 2020. Available online: https://i2connect-h2020.eu/resources/akis-country-reports/ (accessed on 1 February 2024).
- Giagnocavo, C.; de Cara-Garcνa, M.; Gonzαlez, M.; Juan, M.; Marνn-Guirao, J.I.; Mehrabi, S.; Rodrνguez, E.; van der Blom, J.; Crisol-Martνnez, E. Reconnecting Farmers with Nature through Agroecological Transitions: Interacting Niches and Experimentation and the Role of Agricultural Knowledge and Innovation Systems. Agriculture 2022 , 12 , 137. [ Google Scholar ] [ CrossRef ]
- Klitgaard, K. AKIS and Advisory Services in Denmark. Report for the AKIS Inventory (Task 1.2) of the i2connect Project. i2connect INTERACTIVE INNOVATION 2019. Available online: https://i2connect-h2020.eu/resources/akis-country-reports/ (accessed on 29 January 2024).
- Cristiano, S.; Carta, V.; D’Oronzio MA Proietti, P.; Sturla, V. AKIS and Advisory Services in Malta. Report for the AKIS Inventory (Task 1.2) of the i2connect Project. i2connect INTERACTIVE INNOVATION 2020. Available online: https://i2connect-h2020.eu/resources/akis-country-reports/ (accessed on 2 February 2024).
- Knierim, A.; Boenning, K.; Caggiano, M.; Cristσvγo, A.; Dirimanova, V.; Koehnen, T.; Labarthe, P.; Prager, K. The AKIS Concept and its Relevance in Selected EU Member States. Outlook Agric. 2015 , 44 , 29–36. [ Google Scholar ] [ CrossRef ]
- Terziev, V.; Arabska, E. Enhancing Competitiveness and Sustainability of Agri-Food Sector through Market-Oriented Technology Development in Agricultural Knowledge and Innovation System in Bulgaria. In Proceedings of the III International Scientific Congress Agricultural Machinery, Varna, Bulgaria, 22–25 June 2015. [ Google Scholar ]
- Konecna, M.M. AKIS and Advisory Services in Czech Republic. Report for the AKIS inventory (Task 1.2) of the i2connect Project. i2connect INTERACTIVE INNOVATION 2020. Available online: https://i2connect-h2020.eu/resources/akis-country-reports/ (accessed on 28 January 2024).
- Kasdorferova, Z.; Palus, H.; Kadlecikova MSvikruhova, P. AKIS and Advisory Services in Slovak Republic. Report for the AKIS inventory (Task 1.2) of the i2connect Project. i2connect INTERACTIVE INNOVATION 2020. Available online: https://i2connect-h2020.eu/resources/akis-country-reports/ (accessed on 4 February 2024).
- Boczek, K.; Ambryszewska, K.; Dabrowski, J.; Ulicka, A. AKIS and Advisory Services in Poland. Report for the AKIS Inventory (Task 1.2) of the i2connect Project. i2connect INTERACTIVE INNOVATION 2020. Available online: https://i2connect-h2020.eu/resources/akis-country-reports/ (accessed on 3 February 2024).
- Ingram, J.; Mills, J.; Black, J.E.; Chivers, C.-A.; Aznar-Sαnchez, J.A.; Elsen, A.; Frac, M.; Lσpez-Felices, B.; Mayer-Gruner, P.; Skaalsveen, K.; et al. Do Agricultural Advisory Services in Europe Have the Capacity to Support the Transition to Healthy Soils? Land 2022 , 11 , 599. [ Google Scholar ] [ CrossRef ]
- Herzog, F.; Neubauer, E. AKIS and Advisory Services in Austria. Report for the AKIS Inventory (Task 1.2) of the i2connect Project. i2connect INTERACTIVE INNOVATION 2020. Available online: https://i2connect-h2020.eu/resources/akis-country-reports/ (accessed on 27 January 2024).
- Banninger, A. AKIS and Advisory Services in Switzerland. Report for the AKIS inventory (Task 1.2) of the i2connect Project. i2connect INTERACTIVE INNOVATION 2021. Available online: https://i2connect-h2020.eu/resources/akis-country-reports/ (accessed on 5 February 2024).
- Maher, P. AKIS and Advisory Services in Ireland. Report for the AKIS inventory (Task 1.2) of the i2connect Project. i2connect INTERACTIVE INNOVATION 2020. Available online: https://i2connect-h2020.eu/resources/akis-country-reports/ (accessed on 31 January 2024).
- Dunne, A.; Markey, A.; Kinsella, J. Examining the reach of public and private agricultural advisory services and farmers’ perceptions of their quality: The case of county Laois in Ireland. J. Agric. Educ. Ext. 2019 , 25 , 401–414. [ Google Scholar ] [ CrossRef ]
- Knuth, U.; Knierim, A. How to strengthen the link between advisors and research in a privatized advisory system?—The case of Brandenburg, Germany. In Proceedings of the 11th European Symposium, Berlin, Germany, 1–4 April 2014. [ Google Scholar ]
- Konecna, M.M. The role of the Institute of Agricultural Economics and Information in the Czech Agricultural Knowledge Information System. Rural Areas Dev. 2018 , 15 , 49–56. [ Google Scholar ]
- Klerkx, L.; Straete, E.P.; Kvam, G.T.; Ystad, E.; Harstad RM, B. Achieving best-fit configurations through advisory subsystems in AKIS: Case studies of advisory service provisioning for diverse types of farmers in Norway. J. Agric. Educ. Ext. 2017 , 23 , 213–229. [ Google Scholar ] [ CrossRef ]
- Tamsalu, H. AKIS and Advisory Services in Estonia. Report for the AKIS Inventory (Task 1.2) of the i2connect Project. i2connect INTERACTIVE INNOVATION 2021. Available online: https://i2connect-h2020.eu/resources/akis-country-reports/ (accessed on 29 January 2024).
- Kania, J.; Zmija, J. Changes in Agricultural Knowledge and Information Systems: Case Study of Poland. Visegrad J. Bioeconomy 2016 , 5 , 10–17. [ Google Scholar ] [ CrossRef ]
- Xieyang, C.; Tongsheng, l. Diffusion of Agricultural Technology Innovation: Research Progress of Innovation Diffusion in Chinese Agricultural Science and Technology Praks. Sustainability 2022 , 14 , 15008. [ Google Scholar ] [ CrossRef ]
Click here to enlarge figure
| Article ID | Country | Factor(s) Investigated | Key Results Obtained | Suggested Improvements |
|---|---|---|---|---|
| [ ] Kiraly et al. (2023). | European Union countries | Assessing the behavior of European farmers, foresters and advisors regarding the frequency of searching for information on digital transformation using the EU Farmbook application. | ||
| [ ] Ingram and Mills (2019). | European countries | Advisory services regarding sustainable soil management. | ||
| [ ] Laurent et al. (2021). | Southwestern France | Evaluation of the processes by which farmers combine different sources of agricultural advice (micro-AKIS) for three types of innovation. | ||
| [ ] Madureira et al. (2022). | Europe | The role of farm consultancy in agricultural innovation in relation to the microAKIS. | ||
| [ ] Amerani et Michailidis (2023). | Greece | Evaluation of the contribution of the Greek AKIS and its adaptation to modern requirements of Greek agriculture | ||
| [ ] Kiljunen et Jaakkola (2020). | Finland | AKIS and the Farm Advisory System in Finland. | ||
| [ ] Charatsari et al. (2023). | Greece, Italy | Investigation of the possibility of AKIS actors to develop dynamic capacities during the supply process of the food chain. | ||
| [ ] Masi et al. (2022). | Italy | Evaluation of precision agriculture tools as an innovation and the variables that facilitate or hinder their implementation in agricultural practice. | ||
| [ ] Nordlund and Norrby (2021). | Sweden | Detailed description of the Swedish agricultural advisory services. | ||
| [ ] Sturel (2021). | France | French AKIS and Farm Advisory System combined with the promotion of interactive innovation to support the transition in agriculture and forestry. | ||
| [ ] Enfedaque Diaz et al. (2020). | Spain | AKIS and Advisory Services in Spain. | ||
| [ ] Almeida et Viveiros (2020). | Portugal | Report of the AKIS in Portugal, with an emphasis on agricultural advisory services. | ||
| [ ] Birke et al. (2021). | Germany | Overview of the AKIS and the Forestry Knowledge and Innovation System (FKIS) in Germany. | ||
| [ ] Jelakovic (2021). | Croatia | Overview of the Croatian AKIS. | ||
| [ ] Stankovic (2020). | Serbia | Report of the Serbian AKIS and FAS. | ||
| [ ] Hrovatic (2020). | Slovenia | Description of the Slovenian AKIS and FAS. | ||
| [ ] Bachev (2022). | Bulgaria | Analyzing Governance, Efficiency and Development of the AKIS. | ||
| [ ] Koutsouris et al. (2020). | Cyprus | Comprehensive overview of the Cyprus AKIS and the Agricultural Advisory System. | ||
| [ ] Knierim et al. (2019). | Germany | Smart Farming Technologies (SFT) and their degree of perception by farmers. | ||
| [ ] Koutsouris et al. (2020) | Greece | AKIS and agricultural advisory services in Greece. | ||
| [ ] Coquil et al. (2018). | France | The transformations of farmers and AKIS actors’ work during agroecological transitions. | ||
| [ ] Lybaert et Debruyne (2020). | Belgium | Overview of the Belgian AKIS, focusing on agricultural advisory services. | ||
| [ ] Dortmans et al. (2020). | Netherlands | Insight into the Dutch AKIS actors and factors that play a role in the system. | ||
| [ ] Gaborne et al. (2020). | Hungary | The general characteristics of the Hungarian agricultural and forestry sector and AKIS, as well as the historical development of the advisory system. | ||
| [ ] Oliveira et al. (2019). | Portugal | The Portuguese irrigation system of the Lis Valley, within the framework of the EIP AGRI Program of the European Union. | ||
| [ ] Mirra et al. (2020). | Campania region, Italy | Analysis of the implementation of an experimental AKIS model through the RDP. | ||
| [ ] Cristiano et al. (2020). | Italy | An overview of the Italian AKIS and the local Farm Advisory Services (FASs). | ||
| [ ] Todorova (2021). | Bulgaria | A comprehensive description of the Bulgarian AKIS and FAS. | ||
| [ ] Dzelme et Zurins (2021). | Latvia | A description of the AKIS in Latvia and brief outlook of the Forestry AKIS (FKIS). | ||
| [ ] Matuseviciute et al. (2021). | Lithuania | AKIS and FAS in Lithuania. A detailed report. | ||
| [ ] Zimmer et al. (2020). | Luxembourg | Description of the AKIS in Luxembourg. | ||
| [ ] Giagnocavo et al. (2022). | Spain | The reconnection of the farm production system with nature, especially where the production procedure is embedded in less sustainable conventional or dominant regimes and landscapes. | ||
| [ ] Klitgaard (2019). | Denmark | A comprehensive description of the AKIS and FAS in Denmark. | ||
| [ ] Cristiano et al. (2020). | Malta | Description of the AKIS with a focus in the FAS in the Republic of Malta. | ||
| [ ] Knierim et al. (2015) | Belgium, France, Ireland, Germany, Portugal and the UK | The AKIS concept in selected EU member states. | ||
| [ ] Terziev and Arabska (2015). | Bulgaria | Quality assurance and sustainable development in the agri-food sector. | ||
| [ ] Konecna (2020). | Czech Republic | A comprehensive description of theAKIS in the Czech Republic, with a particular focus on farm and forestry advisory services. | ||
| [ ] Kasdorferova et al. (2020). | Slovak Republic | Description of the AKIS and FAS in Slovak Republic. | ||
| [ ] Boczek et al. (2020). | Poland | An overview of the AKIS and FKIS, as well as the FAS in Poland. | ||
| [ ] Ingram et al. (2022). | Europe countries | Evaluation of the advisory services of European countries in the context of sustainable soil management. | ||
| [ ] Herzog et Neubauer (2020). | Austria | Evaluation of the Austrian AKIS. | ||
| [ ] Banninger (2021). | Switzerland | Description of the Swiss AKIS and advisory services. | ||
| [ ] Maher (2020). | Republic of Ireland | Description of the Irish AKIS, with an emphasis on methods of knowledge dissemination and innovation. | ||
| [ ] Dunne et al. (2019). | Laois county, Republic of Ireland | Evaluating the interaction characteristics of public and private Farm Advisory Services in County Laois, Ireland. | ||
| [ ] Knuth and Knierim (2014). | Germany | Scientific bodies and providers of agricultural advisory services: finding ways to strengthen their relationship. | ||
| [ ] Konecna (2018). | Czach Republic | Evaluation of the Institute of Agricultural Economy and Information (IAEI) regarding its innovation potential. | ||
| [ ] Hermans et al. (2019). | England, France, Germany, Hungary, Italy, Latvia, the Netherlands, Switzerland | Effect of AKIS structural factors of eight European countries on cooperative schemes or social learning in innovation networks. | ||
| [ ] Klerkx et al. (2017). | Norway | Challenges for advisory services in serving various types of farmers seeking and acquiring farm business advice. | ||
| [ ] Tamsalu (2021). | Estonia | Presentation of the AKIS in Estonia. | ||
| [ ] Kania and Zmija (2016). | Poland | How cooperation between AKIS stakeholders is assessed from the standpoint of the 16 provincial Agricultural Advisory Centers (ODRs). |
| The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
Share and Cite
Kountios, G.; Kanakaris, S.; Moulogianni, C.; Bournaris, T. Strengthening AKIS for Sustainable Agricultural Features: Insights and Innovations from the European Union: A Literature Review. Sustainability 2024 , 16 , 7068. https://doi.org/10.3390/su16167068
Kountios G, Kanakaris S, Moulogianni C, Bournaris T. Strengthening AKIS for Sustainable Agricultural Features: Insights and Innovations from the European Union: A Literature Review. Sustainability . 2024; 16(16):7068. https://doi.org/10.3390/su16167068
Kountios, Georgios, Spyridon Kanakaris, Christina Moulogianni, and Thomas Bournaris. 2024. "Strengthening AKIS for Sustainable Agricultural Features: Insights and Innovations from the European Union: A Literature Review" Sustainability 16, no. 16: 7068. https://doi.org/10.3390/su16167068
Article Metrics
Article access statistics, further information, mdpi initiatives, follow mdpi.

Subscribe to receive issue release notifications and newsletters from MDPI journals

IMAGES
COMMENTS
Don't know how to write a literature review or where to begin? This video will give you a quick run-through of the 5 steps you need to follow when writing a ...
To avoid this, cancel and sign in to YouTube on your computer. Writing an Annotated Bibliography and Literature Review | Simple Strategy |
Writing a Methodology for Literature Review Leigh Zeitz 484 subscribers Subscribed 1.2K 70K views 5 years ago
Learn how to conduct a literature review for your research project with this tutorial video from SAGE Research Methods.
Video Info Claire White explains how to conduct an effective literature review using a literature review sketch.
A literature review is a survey of scholarly knowledge on a topic. Our guide with examples, video, and templates can help you write yours.
The review revealed that each video evaluation study first established search terms, exclusion criteria, and methods to analyze the videos in a consistent manner.
Performing a literature review is a critical first step in research to understanding the state-of-the-art and identifying gaps and challenges in the field. A systematic literature review is a method which sets out a series of steps to methodically organize the review. In this paper, we present a guide designed for researchers and in particular ...
An analysis of the publications revealed that the literature emerged from multiple academic disciplines. The sample of literature included 39 articles and papers describing methods for teaching with YouTube. A total of 99 articles and papers containing the results of research studies were identified and categorized.
Systematic Literature Review (S LR) is a literature review method that identifies, assesses, and in terprets all findings on a research topic, to answ er pre -determined. research questions ...
This chapter discusses the methodological approaches to conducting a literature review and offers an overview of different types of reviews. There are various types of reviews, including narrative reviews, scoping reviews, and systematic reviews with reporting strategies such as meta-analysis and meta-synthesis.
This paper discusses literature review as a methodology for conducting research and offers an overview of different types of reviews, as well as some guidelines to how to both conduct and evaluate a literature review paper. It also discusses common pitfalls and how to get literature reviews published. 1.
Learn how to write a literature review in three straightforward steps. Includes free literature review templates and resources.
Literature reviews play a critical role in scholarship because science remains, first and foremost, a cumulative endeavour (vom Brocke et al., 2009). As in any academic discipline, rigorous knowledge syntheses are becoming indispensable in keeping up with an exponentially growing eHealth literature, assisting practitioners, academics, and graduate students in finding, evaluating, and ...
The review revealed that each video evaluation study first established search terms, exclusion criteria, and methods to analyze the videos in a consistent manner. The majority of the evaluators devised a scoring system, but variations were innumerable within each study's methods.
The distinction between a systematic literature review and a literature review can often be confusing. This video distinguishes between the two and summarizes the process involved in conducting a ...
Results: The review revealed that each video evaluation study first established search terms, exclusion criteria, and methods to analyze the videos in a consistent manner. The majority of the evaluators devised a scoring system, but variations were innumerable within each study's methods. Conclusions: In comparing the 37 studies, we found that ...
This paper is part of a series of methodological guidance from the Cochrane Rapid Reviews Methods Group. Rapid reviews (RR) use modified systematic review methods to accelerate the review process while maintaining systematic, transparent and reproducible methods. In this paper, we address considerations for RR searches. We cover the main areas relevant to the search process: preparation and ...
This systematic literature review delves into the extensive landscape of emotion recognition, sentiment analysis, and affective computing, analyzing 609 articles. Exploring the intricate relationships among these research domains, and leveraging data from four well-established sources—IEEE, Science Direct, Springer, and MDPI—this systematic review classifies studies in four modalities ...
Recently, the integration of coaching methodologies within educational environments has garnered significant attention due to their potential to enhance student learning outcomes and overall academic performance. While the literature extensively examines the effectiveness of coaching in a plethora of scenarios (e.g., sports, business, and entrepreneurship), there remains a notable research gap ...
Methods: This study used a 5-step scoping review methodology following Arksey and O'Malley's methodology to map relevant literature published in English between January 2012 and March 2024, focusing on health misinformation on social media platforms.
Reviewing the literature requires the ability to juggle multiple tasks, from finding and evaluating relevant material to synthesising information from various sources, from critical thinking to paraphrasing, evaluating, and citation skills [7]. In this contribution, I share ten simple rules I learned working on about 25 literature reviews as a PhD and postdoctoral student. Ideas and insights ...
This study aims to systematically review the literature to examine the direct and indirect effects of economic sanctions on health through a narrative synthesis. Methods. This systematic literature review was limited to papers published between January 1990 and July 2023.
Literature review in research proposal - Writing literature review is a must-have and a transferable skill for every researcher. Literature review is often a part of the introduction to a research ...
Metastatic cancer should be considered in patients with head and neck cancer who have unexplained skin changes at the gastrostomy site. Our experience with this case and review of the literature indicate that, in patients with head and neck cancer, "pull" procedures for placement of gastrostomy tube …
Systematic literature reviews are the highest quality of evidence in research. However, the review process is hindered by significant resource and data constraints. The Literature Review Network (LRN) is the first of its kind explainable AI platform adhering to PRISMA 2020 standards, designed to automate the entire literature review process.
This study aims to report our experience in the use of RS in AES assessing its safety and feasibility, with particular focus on intra- and post-operative complications, conversion rate, and surgical learning curve. Our data were also compared to other experiences though an extensive literature review. Methods
Writing an effective literature review. In the Writer's Craft section we offer simple tips to improve your writing in one of three areas: Energy, Clarity and Persuasiveness. Each entry focuses on a key writing feature or strategy, illustrates how it commonly goes wrong, teaches the grammatical underpinnings necessary to understand it and ...
Matrix method enables you to quickly compare and contrast articles in order to determine the scope of research across time. The good about matrix method can help you easily spot the differences ...
The present literature review was based on the PRISMA (Preferred Reporting Items for Systematic reviews and Meta-Analyses) method, using a checklist, which is linked to a flow diagram of three phases: identification, screening and inclusion. PRISMA is an evidence-based minimum set of items for reporting in systematic reviews and meta-analyses.