Hypertension: Current trends and future perspectives
Affiliation.
- 1 Department of Renal Medicine, Royal Infirmary of Edinburgh & University/BHF Centre for Cardiovascular Science, The Queen's Medical Research Institute, University of Edinburgh, UK.
- PMID: 33733505
- DOI: 10.1111/bcp.14825
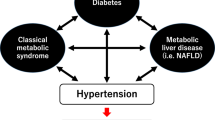
Hypertension is a significant and increasing global health issue. It is a leading cause of cardiovascular disease and premature death worldwide due to its effects on end organs, and through its associations with chronic kidney disease, diabetes mellitus and obesity. Despite current management strategies, many patients do not achieve adequate blood pressure (BP) control. Hypertension-related cardiovascular mortality rates are rising in tandem with the increasing global prevalence of chronic kidney disease, diabetes mellitus and obesity. Improving BP control must therefore be urgently prioritised. Strategies include utilising existing antihypertensive agents more effectively, and using treatments developed for co-existing conditions (such as sodium-glucose cotransporter 2 inhibitors for diabetes mellitus) that offer additional BP-lowering and cardiovascular benefits. Additionally, novel therapeutic agents that target alternative prohypertensive pathways and that offer broader cardiovascular protection are under development, including dual angiotensin receptor-neprilysin inhibitors. Nonpharmacological strategies such as immunotherapy are also being explored. Finally, advancing knowledge of the human genome and molecular modification technology may usher in an exciting new era of personalised medicine, with the potential to revolutionise the management of hypertension.
Keywords: diabetes; hypertension; kidney disease; treatments.
© 2021 The Authors. British Journal of Clinical Pharmacology published by John Wiley & Sons Ltd on behalf of British Pharmacological Society.

Publication types
- Research Support, Non-U.S. Gov't
- Antihypertensive Agents / pharmacology
- Antihypertensive Agents / therapeutic use
- Blood Pressure
- Cardiovascular Diseases* / drug therapy
- Diabetes Mellitus* / drug therapy
- Diabetes Mellitus, Type 2* / drug therapy
- Hypertension* / drug therapy
- Hypertension* / epidemiology
- Antihypertensive Agents
Grants and funding
- SCAF/19/02/CSO_/Chief Scientist Office/United Kingdom
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Mini Review
- Published: 09 September 2024
Hypertension research 2024 update and perspectives: basic research
- Kento Kitada 1
Hypertension Research volume 47 , pages 3304–3309 ( 2024 ) Cite this article
131 Accesses
2 Altmetric
Metrics details
This review article introduces some basic studies that were recently published in this journal, as a part of Hypertension Research 2024 Update and Perspectives. Including recent basic research trends in other scientific journals, we would like to summarize basic research on keywords such as hypertension and its associated organ damage, new treatments, and others. It is expected that the accumulation of basic studies will lead to breakthroughs in hypertension treatment in the future and lead to the definitive treatment of hypertension beyond blood pressure control with anti-hypertensive drugs.

This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
251,40 € per year
only 20,95 € per issue
Buy this article
- Purchase on SpringerLink
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others

Update on Hypertension Research in 2021

Annual reports on hypertension research 2020
2023 update and perspectives
Coste B, Delmas P. PIEZO ion channels in cardiovascular functions and diseases. Circ Res. 2024;134:572–91.
CAS PubMed Google Scholar
Wang H, Yuan Z, Wang B, Li B, Lv H, He J, et al. COMP (cartilage oligomeric matrix protein), a novel Piezo1 regulator that controls blood pressure. Hypertension. 2022;79:549–61.
PubMed Google Scholar
Fei L, Xu M, Wang H, Zhong C, Jiang S, Lichtenberger FB, et al. Piezo1 mediates vasodilation induced by acute hyperglycemia in mouse renal arteries and microvessels. Hypertension. 2023;80:1598–610.
Harraz OF, Klug NR, Senatore AJ, Hill-Eubanks DC, Nelson MT. Piezo1 is a mechanosensor channel in central nervous system capillaries. Circ Res. 2022;130:1531–46.
CAS PubMed PubMed Central Google Scholar
Choi D, Park E, Yu RP, Cooper MN, Cho IT, Choi J, et al. Piezo1-regulated mechanotransduction controls flow-activated lymphatic expansion. Circ Res. 2022;131:e2–e21.
Hirata Y, Nomura K, Kato D, Tachibana Y, Niikura T, Uchiyama K, et al. A Piezo1/KLF15/IL-6 axis mediates immobilization-induced muscle atrophy. J Clin Invest. 2022;132:1–13.
Bartoli F, Debant M, Chuntharpursat-Bon E, Evans EL, Musialowski KE, Parsonage G, et al. Endothelial Piezo1 sustains muscle capillary density and contributes to physical activity. J Clin Invest. 2022;132:e141775.
Matrongolo MJ, Ang PS, Wu J, Jain A, Thackray JK, Reddy A, et al. Piezo1 agonist restores meningeal lymphatic vessels, drainage, and brain-CSF perfusion in craniosynostosis and aged mice. J Clin Invest. 2023;134:e171468.
PubMed PubMed Central Google Scholar
Carrisoza-Gaytan R, Mutchler SM, Carattino F, Soong J, Dalghi MG, Wu P, et al. PIEZO1 is a distal nephron mechanosensor and is required for flow-induced K+ secretion. J Clin Invest. 2024;134:e174806.
He Y, Deng B, Liu S, Luo S, Ning Y, Pan X, et al. Myeloid Piezo1 deletion protects renal fibrosis by restraining macrophage infiltration and activation. Hypertension. 2022;79:918–31.
Ogino S, Yoshikawa K, Nagase T, Mikami K, Nagase M. Roles of the mechanosensitive ion channel Piezo1 in the renal podocyte injury of experimental hypertensive nephropathy. Hypertens Res. 2024;47:747–59.
Ochiai K, Mochida Y, Nagase T, Fukuhara H, Yamaguchi Y, Nagase M. Upregulation of Piezo2 in the mesangial, renin, and perivascular mesenchymal cells of the kidney of Dahl salt-sensitive hypertensive rats and its reversal by esaxerenone. Hypertens Res. 2023;46:1234–46.
Harrison DG, Patrick DM. Immune mechanisms in hypertension. Hypertension. 2024;81:1659–74.
Liang H, Liu B, Gao Y, Nie J, Feng S, Yu W, et al. Jmjd3/IRF4 axis aggravates myeloid fibroblast activation and m2 macrophage to myofibroblast transition in renal fibrosis. Front Immunol. 2022;13:978262.
Huang M, Wang Q, Long F, Di Y, Wang J, Zhun Zhu Y, et al. Jmjd3 regulates inflammasome activation and aggravates DSS-induced colitis in mice. FASEB J. 2020;34:4107–19.
He C, Larson-Casey JL, Gu L, Ryan AJ, Murthy S, Carter AB. Cu,Zn-superoxide dismutase-mediated redox regulation of Jumonji domain containing 3 modulates macrophage polarization and pulmonary fibrosis. Am J Respir Cell Mol Biol. 2016;55:58–71.
Gao Y, Yu W, Song J, Nie J, Cui Z, Wen S, et al. JMJD3 ablation in myeloid cells confers renoprotection in mice with DOCA/salt-induced hypertension. Hypertens Res. 2023;46:1934–48.
Norlander AE, Madhur MS, Harrison DG. The immunology of hypertension. J Exp Med. 2018;215:21–33.
Wilck N, Matus MG, Kearney SM, Olesen SW, Forslund K, Bartolomaeus H, et al. Salt-responsive gut commensal modulates T(H)17 axis and disease. Nature. 2017;551:585–9.
Kim JY, Lee S, Jang S, Kim CW, Gu BH, Kim M, et al. T helper cell polarity determines salt sensitivity and hypertension development. Hypertens Res. 2023;46:2168–78.
Mailankody S, Devlin SM, Landa J, Nath K, Diamonte C, Carstens EJ, et al. GPRC5D-targeted CAR T cells for myeloma. N. Engl J Med. 2022;387:1196–206.
Arcangeli S, Bove C, Mezzanotte C, Camisa B, Falcone L, Manfredi F, et al. CAR T cell manufacturing from naive/stem memory T lymphocytes enhances antitumor responses while curtailing cytokine release syndrome. J Clin Invest. 2022;132:e150807.
Jaspers JE, Khan JF, Godfrey WD, Lopez AV, Ciampricotti M, Rudin CM, et al. IL-18-secreting CAR T cells targeting DLL3 are highly effective in small cell lung cancer models. J Clin Invest. 2023;133:e166028.
Mackensen A, Müller F, Mougiakakos D, Böltz S, Wilhelm A, Aigner M, et al. Anti-CD19 CAR T cell therapy for refractory systemic lupus erythematosus. Nat Med. 2022;28:2124–32.
Rurik JG, Tombácz I, Yadegari A, Méndez Fernández PO, Shewale SV, Li L, et al. CAR T cells produced in vivo to treat cardiac injury. Science. 2022;375:91–96.
Baker DJ, Arany Z, Baur JA, Epstein JA, June CH. CAR T therapy beyond cancer: the evolution of a living drug. Nature. 2023;619:707–15.
Tamura K, Azushima K, Kinguchi S, Wakui H, Yamaji T. ATRAP, a receptor-interacting modulator of kidney physiology, as a novel player in blood pressure and beyond. Hypertens Res. 2022;45:32–39.
Patel KP, Katsurada K, Zheng H. Cardiorenal syndrome: the role of neural connections between the heart and the kidneys. Circ Res. 2022;130:1601–17.
Sotozawa M, Kinguchi S, Wakui H, Azushima K, Funakoshi K, Nakajima W, et al. Enhancement of angiotensin II type 1 receptor-associated protein in the paraventricular nucleus suppresses angiotensin II-dependent hypertension. Hypertens Res. 2024;47:67–77.
Taguchi S, Azushima K, Yamaji T, Suzuki T, Abe E, Tanaka S, et al. Angiotensin II type 1 receptor-associated protein deletion combined with angiotensin II stimulation accelerates the development of diabetic kidney disease in mice on a C57BL/6 strain. Hypertens Res. 2024;47:55–66.
Zhu Y, Chu Y, Wang S, Tang J, Li H, Feng L, et al. Vascular smooth muscle TRPV4 (transient receptor potential vanilloid family member 4) channels regulate vasoconstriction and blood pressure in obesity. Hypertension. 2023;80:757–70.
Adapala RK, Katari V, Kanugula AK, Ohanyan V, Paruchuri S, Thodeti CK. Deletion of endothelial TRPV4 protects heart from pressure overload-induced hypertrophy. Hypertension. 2023;80:2345–56.
Wen X, Peng Y, Peng Y, Zhu Y, Yu F, Geng L, et al. Aortic smooth muscle TRPV4 channels regulate vasoconstriction in high salt-induced hypertension. Hypertens Res. 2023;46:2356–67.
Hu X, Du L, Liu S, Lan Z, Zang K, Feng J, et al. A TRPV4-dependent neuroimmune axis in the spinal cord promotes neuropathic pain. J Clin Invest. 2023;133:e161507.
Avolio E, Katare R, Thomas AC, Caporali A, Schwenke D, Carrabba M, et al. Cardiac pericyte reprogramming by MEK inhibition promotes arteriologenesis and angiogenesis of the ischemic heart. J Clin Invest. 2022;132:e152308.
Quijada P, Park S, Zhao P, Kolluri KS, Wong D, Shih KD, et al. Cardiac pericytes mediate the remodeling response to myocardial infarction. J Clin Invest. 2023;133:e162188.
Alex L, Tuleta I, Hernandez SC, Hanna A, Venugopal H, Astorkia M, et al. Cardiac pericytes acquire a fibrogenic phenotype and contribute to vascular maturation after myocardial infarction. Circulation. 2023;148:882–98.
Lin SL, Kisseleva T, Brenner DA, Duffield JS. Pericytes and perivascular fibroblasts are the primary source of collagen-producing cells in obstructive fibrosis of the kidney. Am J Pathol. 2008;173:1617–27.
Duffield JS. Cellular and molecular mechanisms in kidney fibrosis. J Clin Invest. 2014;124:2299–306.
Ito H, Hirose T, Sato S, Takahashi C, Ishikawa R, Endo A, et al. Pericyte detachment and renal congestion involve interstitial injury and fibrosis in Dahl salt-sensitive rats and humans with heart failure. Hypertens Res. 2023;46:2705–17.
Dai S, Zhao L, Wang G, Chen C, Li C, Xiao B, et al. Celiac ganglia neurolysis suppresses high blood pressure in rats. Hypertens Res. 2023;46:1771–81.
Kamata K, Kinoshita M, Kinoshita I, Imai H, Ogura T, Matsumoto H, et al. Efficacy of EUS-guided celiac plexus neurolysis in combination with EUS-guided celiac ganglia neurolysis for pancreatic cancer-associated pain: a multicenter prospective trial. Int J Clin Oncol. 2022;27:1196–201.
Azizan EAB, Drake WM, Brown MJ. Primary aldosteronism: molecular medicine meets public health. Nat Rev Nephrol. 2023;19:788–806.
Wang X, Luo T, Yang Y, Zhou Y, Hou J, Wang P. Unilateral chemical ablation of the adrenal gland lowers blood pressure and alleviates target organ damage in spontaneously hypertensive rats. Hypertens Res. 2023;46:2693–704.
Tuttle KR, Hauske SJ, Canziani ME, Caramori ML, Cherney D, Cronin L, et al. Efficacy and safety of aldosterone synthase inhibition with and without empagliflozin for chronic kidney disease: a randomised, controlled, phase 2 trial. Lancet. 2024;403:379–90.
Huff AL, Jaffee EM, Zaidi N. Messenger RNA vaccines for cancer immunotherapy: progress promotes promise. J Clin Invest. 2022;132:e156211.
Nakagami H. Challenges in the development of novel therapies, vaccines and siRNAs for the treatment of hypertension. Hypertens Res. 2023;46:1812–5.
Ma Z, Mao C, Chen X, Yang S, Qiu Z, Yu B, et al. Peptide vaccine against ADAMTS-7 ameliorates atherosclerosis and postinjury neointima hyperplasia. Circulation. 2023;147:728–42.
Ke F, Kuang W, Hu X, Li C, Ma W, Shi D, et al. A novel vaccine targeting β1-adrenergic receptor. Hypertens Res. 2023;46:1582–95.
Jana BA, Shivhare P, Srivastava R. Gelatin-PVP dissolving microneedle-mediated therapy for controlled delivery of nifedipine for rapid antihypertension treatment. Hypertens Res. 2024;47:427–34.
Download references

Author information
Authors and affiliations.
Department of Pharmacology, Faculty of Medicine, Kagawa University, Kagawa, 7610793, Japan
Kento Kitada
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Kento Kitada .
Ethics declarations
Conflict of interest.
The author declares no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
Reprints and permissions
About this article
Cite this article.
Kitada, K. Hypertension research 2024 update and perspectives: basic research. Hypertens Res 47 , 3304–3309 (2024). https://doi.org/10.1038/s41440-024-01878-2
Download citation
Received : 31 July 2024
Accepted : 13 August 2024
Published : 09 September 2024
Issue Date : December 2024
DOI : https://doi.org/10.1038/s41440-024-01878-2
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Blood pressure
- Hypertension
- Organ damage
- Basic research
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies

IMAGES
VIDEO
COMMENTS
In the future, genome editing (using CRISPR-Cas9) holds promise for curing genetic hypertension, and in targeting angiotensinogen and other targets, resulting in possible long-term control of essential hypertension.
There have been lessons learned from the COVID-19 pandemic that will impact hypertension research and medicine, including new paradigms in human disease, for example, infection as an important comorbidity in cardiovascular disease, and new approaches in clinical practice, for example, telemedicine.
Hypertension is a significant and increasing global health issue. It is a leading cause of cardiovascular disease and premature death worldwide due to its effects on end organs, and through its associations with chronic kidney disease, diabetes mellitus and obesity.
Hypertension is a significant and increasing global health issue. It is a leading cause of cardiovascular disease and premature death worldwide due to its effects on end organs, and through its associations with chronic kidney disease, diabetes mellitus and obesity.
Hypertension is a global health issue associated with increased cardiovascular morbidity and mortality. This study aimed to investigate contemporary hypertension identification and management trends following the 2017 American College of Cardiology/American Heart Association guidelines.
It is expected that the accumulation of basic studies will lead to breakthroughs in hypertension treatment in the future and lead to the definitive treatment of hypertension beyond blood pressure...